Pickleball is a sport that combines elements of tennis, badminton, and ping-pong, played with paddles and a plastic ball. Over the past few years it has been the fastest-growing sport in the country, with the number of pickleball players rising from 4.8 million in 2021 to nearly 9 million last year, according to an estimate from USA Pickleball, the sport’s governing body in the United States.1
In this article, we present 2 cases of ocular trauma secondary to pickleball injuries in middle-aged myopic women. The cases underline the variety of presentations and the extent of retinal repercussions this popular new sport can cause.
Case 1
The first case involves a 47-year-old Caucasian female with a medical history of myopia (-4.00 D OU) as well as LASIK 10 years prior to the visit. Two days after being hit in the left eye while playing pickleball, she presented to the vitreoretinal service for consultation. The patient said that she plays pickleball 4 times a week, on average.
On examination, the patient presented with a best-corrected visual acuity (BCVA) of 20/20 OD and 20/30 OS. Intraocular pressures (IOP) were within normal limits in both eyes. Anterior chamber was within normal limits (WNL) as well. Upon retinal examination, there was a whitish deep retinal lesion within an area that is consistent with commotio retinae on the left eye. Patient was given retinal detachment precautions. When the patient followed up on consultation, the vision had corrected to 20/20 OS and there was a reconstitution of the normal reflectance of the retina in the area in which this lesion was previously apparent.
Case 2
The second case involves a 55-year-old Asian female with a medical history of myopia (-5.00 D OU) corrected with spectacles. The patient was referred by her optometrist for vitreoretinal consultation due to an increase in floaters after trauma to her left eye.
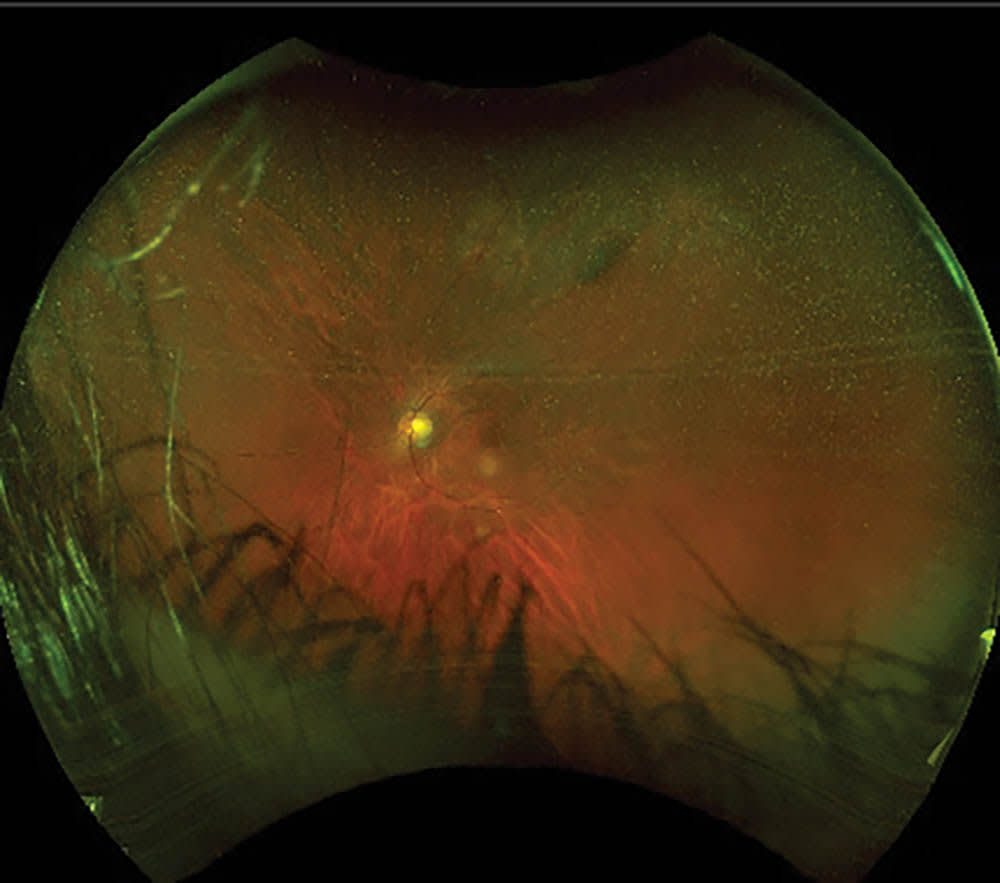
On examination, patient’s BCVA was 20/20 OD and 20/40 OS. IOP was WNL and anterior chamber examination was normal. The vitreous cavity of the left eye exhibited “tobacco dusting” intermixed with a mild vitreous hemorrhage and a mid-peripheral superior retinal tear (Figure 1). Laserpexy was discussed with the patient, and she underwent the procedure uneventfully. Upon return 1 week later, the vitreous hemorrhage had subsided and BCVA returned to 20/20 OS (Figure 2). Patient was advised to wear protective eyewear when engaging in pickleball matches in the future.

Discussion
USA Pickleball estimates that about 17% of pickleball players are 65 and older.1 “Visual impairment is more common in this population because of cataract, macular degeneration, and other causes, making it more challenging for participants to see and avoid a wayward ball or racquet,” the researchers said in a study performed on patients who experienced retinal tears while playing pickleball.1
A study by Atkinson et al outlined two cases of pickleball players who suffered retinal tears secondary to direct projectile injury while playing pickleball.2 In one case, a 66-year-old male patient presented with a symptomatic retinal tear with a localized retinal detachment and mild vitreous hemorrhage 9 days after he was hit in his left eye while playing pickleball. The retinal tear was successfully treated with cryotherapy. In the second case, a 60-year-old patient presented with a posterior vitreous detachment and a symptomatic retinal tear 1 month after blunt trauma to her left eye from a pickleball injury. This patient underwent successful laser retinopexy treatment, just as in our Case 2 described previously.
The weight of a pickleball is 22.11 g to 26.51 g, less than half the weight of a tennis ball (56.0 to 59.4 g).3 Amateur pickleball players can hit the ball around 30 to 40 mph,3 compared to a amateur tennis player’s serve speed of 60 to 80 mph.4 However, pickleball players interact in closer proximity than in tennis, given the configuration of the pickleball court, so the risk of injury exists given short deceleration distances and requiring high reaction times. Given the morphology and speed of the projectile in pickleball, there are not documented instances in which there are separations of the vitreous base, retinal dialysis, or bullous retinal detachments requiring vitrectomy or pneumatic retinopexy, as is commonly observed in instances of severe ocular trauma. Lesions are limited to the retinal mid-periphery in most documented instances. Most cases are amenable to in-clinic treatment.
Although the use of eye protection is not a requirement in the game of pickleball, use of protective eyewear such as sports glasses should be strongly recommended to patients with myopia or other ocular comorbidities that would alter patient’s response times. Protective eyewear might be a consideration given that a large demographic of pickleball players might overlap with the older population that is prone to age-related macular degeneration, which further hampers vision and, consequently, reaction times.
According to the American Academy of Ophthalmology (AAO), about 40% of eye injuries each year occur during sports and recreational activities.5 Moreover, the AAO notes there are about 30,000 sports-related eye injuries annually in the United States.
The costs of all pickleball injuries, including eye-related issues, could result in health insurance costs ranging from $250 million to $500 million in 2023 alone, according to estimates from the investment bank UBS.6 In a note issued in June 2023, UBS calculated medical costs for the year and forecast 67,000 emergency room visits, 366,000 outpatient visits, 8,800 outpatient surgeries, 4,700 hospitalizations, and 20,000 follow-up visits related to injuries caused by pickleball, including eye injuries.
It is important to note that ophthalmologists, as well as avid pickleball players, should familiarize themselves with the possible eye injuries related to the sport. Players that have experienced any type of eye injury while playing should visit an ophthalmologist, and prompt referral to a vitreoretinal specialist is necessary if equivocal retinal findings are present. The choice to wear protective eyeglasses remains optional, but should be strongly suggested for patients with high myopia or other underlying visual pathology.
Conclusion
Pickleball-related injuries appear more commonly in the equatorial retina. Given the type of projectile and configuration of the court on which the game is played, pickleball does not appear to cause injury that would alter the peripheral vitreoretinal dynamics. It is our recommendation that habitual pickleball players with a history of myopia, those with ocular comorbidities affecting play, or those with lesions that could increase the risk of retinal detachment, wear protective eyewear. NRP
References
1. USA Pickleball. SFIA topline report tabs pickleball as America’s fastest-growing sport for third consecutive year. February 22, 2023. Accessed February 26, 2024. https://usapickleball.org/news/sfia-topline-report-tabs-pickleball-as-americas-fastest-growing-sport/
2. Atkinson CF, Patron ME, Joondeph BC. Retinal tears due to pickleball injury. Retin Cases Brief Rep. 2022;16(3):312-313. doi:10.1097/ICB.0000000000000965.
3. Net World Sports. The ultimate guide to pickleball balls. Accessed March 7, 2024. https://www.networldsports.com/buyers-guides/pickleball-ball-guide
4. Sampson M. Average tennis serve speed. Tennis Universe. March 27, 2023. Accessed March 7, 2024. https://tennisuniverse.org/average-serve-speed/
5. Turbert D. Eye injury prevention. American Academy of Ophthalmology. April 14, 2021. Accessed March 7, 2024. https://www.aao.org/eye-health/tips-prevention/preventing-injuries
6. Bohannon M. Pickleball injuries cost Americans nearly $400 million this year—and seniors are hit the hardest. Forbes. Jun 27, 2023. Accessed March 7, 2024. https://www.forbes.com/sites/mollybohannon/2023/06/26/pickleball-injuries-cost-americans-nearly-400-million-this-year---and-seniors-are-hit-hardest










