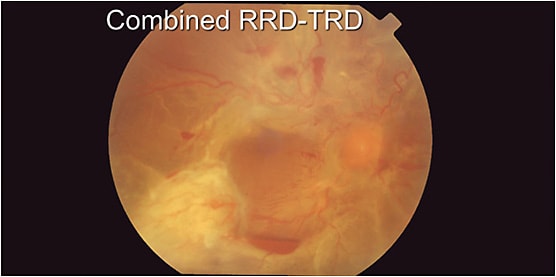
Ultimately, the goal of tractional retinal detachment (TRD) repair with diabetic retinopathy is to remove vitreous opacities, release traction, attach the retina, and complete the panretinal photocoagulation (PRP), so the patient can see. It was standard of care several years ago to leave a TRD that did not affect the macula or even the fovea, because it was considered stable and it was not going to really change if you did enough PRP.
But now that we have better surgical techniques, we can go to the OR sooner—leading to better vision much faster.
CONSIDERATIONS IN TRD
How quickly is the disease progressing? Is surgery urgent, or has the patient been functioning like this for a while? If vision cannot be saved, then contemplate what you are really trying to accomplish. How much peripheral vision the patient will retain is determined by how aggressively you peel peripheral membranes and perform PRP.
Consider the fellow eye. If the patient is monocular, avoid manipulating the fovea and inserting long-acting gas. You always want to avoid causing breaks, but be extra careful with a monocular patient. If you are going to patch them after surgery, admit them to hospital.
OIL, GAS, AND GAUGE
Ideally, 5,000 centistokes (cSt) oil is preferred over 1,000 cSt oil because it can be left in the eye for longer. The 1,000 cSt oil breaks down after a few months and it can emulsify, causing other issues.
When using gas, consider how long-acting it is; C3F8 (long) vs SF6 (short).
With a smaller gauge, such as a 27 or 25 gauge, the port of the vitrectomy cutter is closer to the tip, which can help dissect membranes; and if you refrain from suturing, there is less post-op pain. The sphere of influence is less of an issue and making peripheral breaks is less of a concern because you will be doing a thorough PRP.
The disadvantage of smaller-gauge surgery is that it is slow, especially when instilling 5,000 cSt oil. However, you can always enlarge a sclerotomy to introduce the oil through a 20 gauge. Small-gauge instruments are not as stiff and have a smaller mouth. If there are thick membranes, they may not eat them as well. There may also be fewer small-gauge tools available.
BRINGING IT ALL TOGETHER
Start with the peripheral vitrectomy, working posterior to anterior. Remove the macular membranes, start segmenting around the disc, but get all the blood out of the way so you can see what you are doing. If you peel the ILM, try to stay along the surface of the retina. Lifting the hyaloid releases traction from the fovea without damaging it, but it can be sticky, so you might have to segment it.
Passively drain out of a back-flush cannula by releasing your finger from the back flush part. Then finish the PRP under air, particularly anterior PRP, through a well-dilated pupil because you might not have the opportunity in the clinic in the future. The PRP spots will grow over time, so the patient will not have any peripheral vision; but they probably didn’t already.
POST-VITRECTOMY
Post-vitrectomy considerations include re-proliferation of membranes, which can act as a scaffold for neovascularization in place of the hyaloid. Intraocular pressure is always an issue. Neovascular glaucoma zips up the angle and this can lead to blindness and removal of the eye.
Now that we have expanded our indications for diabetic vitrectomy and have better tools, we see better results. But you must be aggressive; if a patient gets to this point with their diabetes, they were probably noncompliant to begin with.








