The Centers for Medicare and Medicaid Services (CMS) has released its final 2026 payment regulation for hospital outpatient departments and ambulatory surgery centers (ASCs), setting a 2.6% increase to overall ASC payment rates. The update reflects a 3.3% hospital market basket adjustment, reduced by a 0.7% productivity offset, and applies across all ASC procedures.
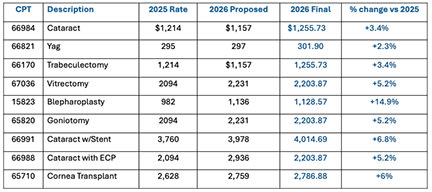
Table 1: Final 2026 ASC Payment Rule for Ophthalmic Services
Cataract surgery was a central point of contention in the rulemaking process. CMS had proposed a 4.7% payment reduction for 2026, prompting objections from the Outpatient Ophthalmic Surgery Society (OOSS) and the American Academy of Ophthalmology (AAO), which argued that the agency relied on a flawed calculation. CMS ultimately revised the payment upward, finalizing a 2026 rate of $1,255, which represents a rate 8.4% hgher than the proposed amount and 3.3% higher than the 2025 rate.
“This is a phenomenal result for cataract surgeons, ophthalmic ASCs and our patients,” said Michael Romansky, JD, general counsel to OOSS. “It demonstrates that an aggressive and coordinated advocacy effort by the ophthalmology community can have a meaningful impact on CMS’s deliberations.”
The rule also extends through 2026 the policy that applies the hospital market basket to ASC updates, a change OOSS has advocated for more than 2 decades. The policy was originally intended for re-evaluation during this cycle, but CMS cited pandemic-related data limitations as the reason for continuing the trial period.
CMS also finalized payment adjustments across key ophthalmic procedures, including increases for vitrectomy, trabeculectomy, blepharoplasty, and cataract surgery with stent placement (Table 1). The agency removed several ASC quality-reporting measures opposed by ophthalmology groups and declined to advance quality reporting proposal ASC-11, that would have required facilities to report postoperative visual function outcomes. RP