Retinal surgeons choose from a variety of instruments and surgical techniques when removing intraocular foreign bodies (IOFBs) from the posterior segment.1-4 The nature and size of the material, as well as concomitant pathology such as the integrity and clarity of the cornea, lens, and anterior segment are all important.5 Our aims are to be as atraumatic as possible and to remove the IOFB on the first attempt, trying to avoid common complications such as the IOFB lodging in the sclerotomy or dropping the IOFB, causing macular injury.
Several commonly used techniques are briefly described below. We would like to highlight our use of the third option, where we deliver the IOFB using an instrument in the inferotemporal port—an approach we believe provides several advantages.
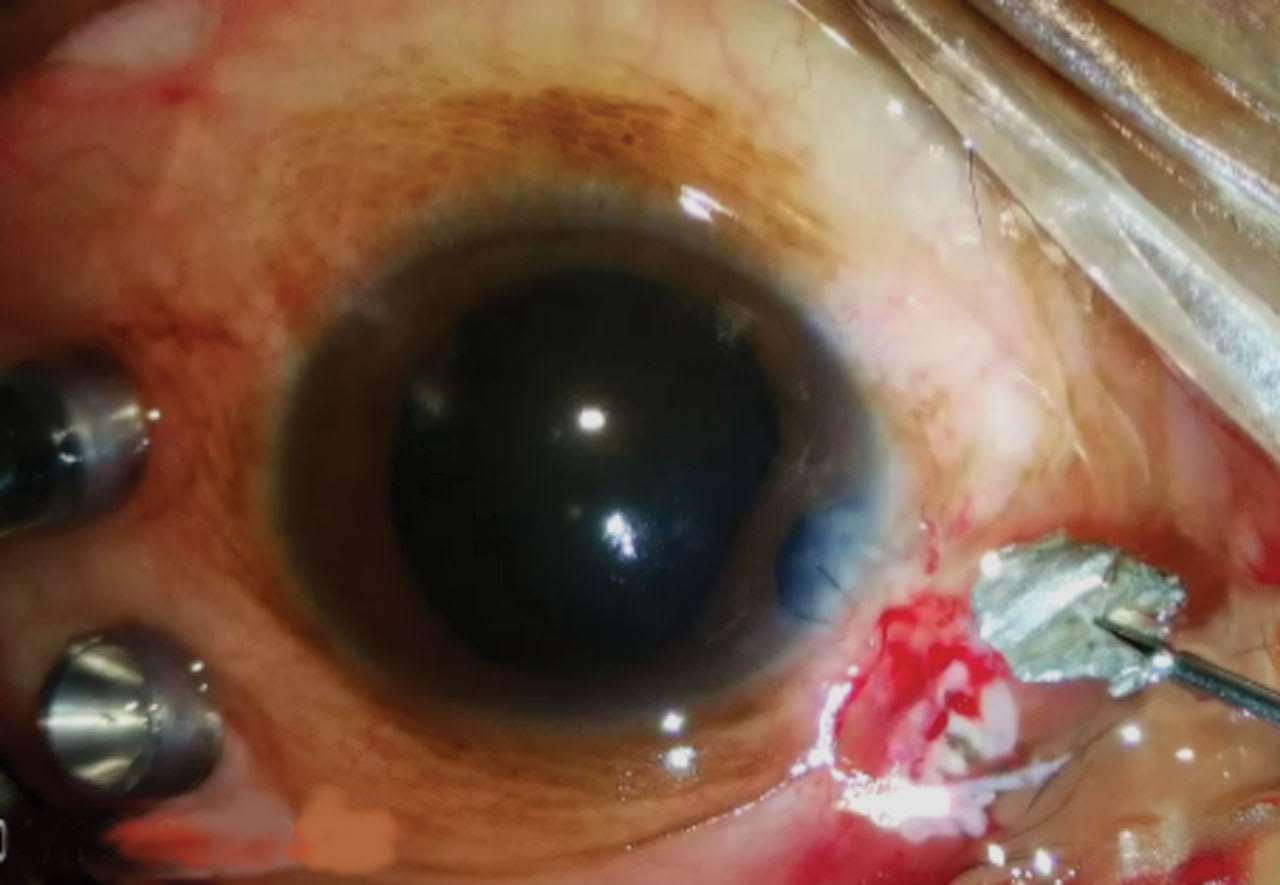
Figure 1. The intraocular foreign body (IOFB) has been extracted directly through the enlarged sclerotomy.
Direct Sclerotomy Extraction
One technique for IOFB removal involves direct extraction through an enlarged sclerotomy (Figure 1). In this approach, the surgeon inserts a suitable instrument through a sclerotomy that is appropriately sized to accommodate the foreign body. The IOFB is grasped and removed directly; in some cases, the sclerotomy is only enlarged at the time of extraction. This method allows the use of the surgeon’s dominant hand; avoids the need to transfer the IOFB between instruments, which reduces the risk of dropping it; and helps preserve a clear crystalline lens.
However, there are potential drawbacks. The foreign body may become dislodged when it is withdrawn through the sclerotomy, possibly becoming trapped or falling back into the posterior segment, increasing the risk of retinal injury. A large sclerotomy also carries risks of hemorrhage and choroidal pigment dispersion. If a large sclerotomy is created at the outset, excessive leakage may lead to intraocular turbulence and hypotony, which can further increase the risk of bleeding.
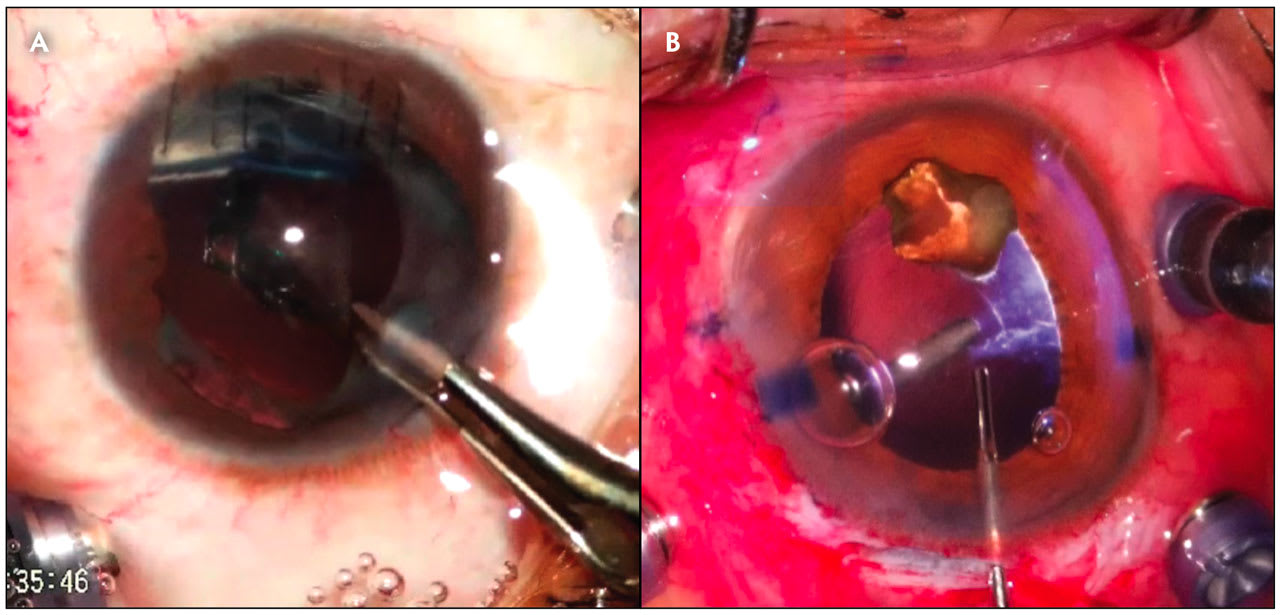
Figure 2. (A) Handshake technique with extraction through a scleral tunnel. In this case, a piece of glass is held by a lasso and then retrieved by the forceps. (B) The IOFB is placed on iris/capsule scaffold, assisted by OVD, and extracted through a scleral tunnel.
Controlled Transfer Through Anterior Segment
Another approach to IOFB removal involves extraction through limbal or scleral tunnel incisions using a “handshake” technique (Figure 2). This method is appropriate when the lens capsule is already disrupted—often the case due to the foreign body’s entry trajectory—or after intentional lens removal.6,7 The surgeon elevates the IOFB from the posterior segment using an instrument inserted through a conventional superior trocar. A second instrument, introduced through a limbal or scleral tunnel incision, then receives the IOFB in a controlled transfer and extracts it through the anterior segment.
In some variations of this technique, the IOFB is first placed temporarily on the inferior iris or residual capsular support. The extracting instrument is then introduced through the limbal wound or scleral tunnel to remove the foreign body. The use of ophthalmic viscosurgical devices (OVD) can help stabilize the IOFB in the anterior chamber during instrument exchange, improving control and reducing the risk of posterior displacement.3
This technique avoids the need for a large sclerotomy and its associated risks, allowing the IOFB to be removed through conventional anterior segment incisions. However, the maneuver does carry a risk of the foreign body being dropped during the transfer between instruments, particularly due to turbulence that may occur when the anterior chamber is opened. In addition, induced hypotony and corneal distortion can impair visualization. These challenges can be mitigated to some extent through liberal use of OVD to stabilize the chamber and reduce intraocular turbulence.
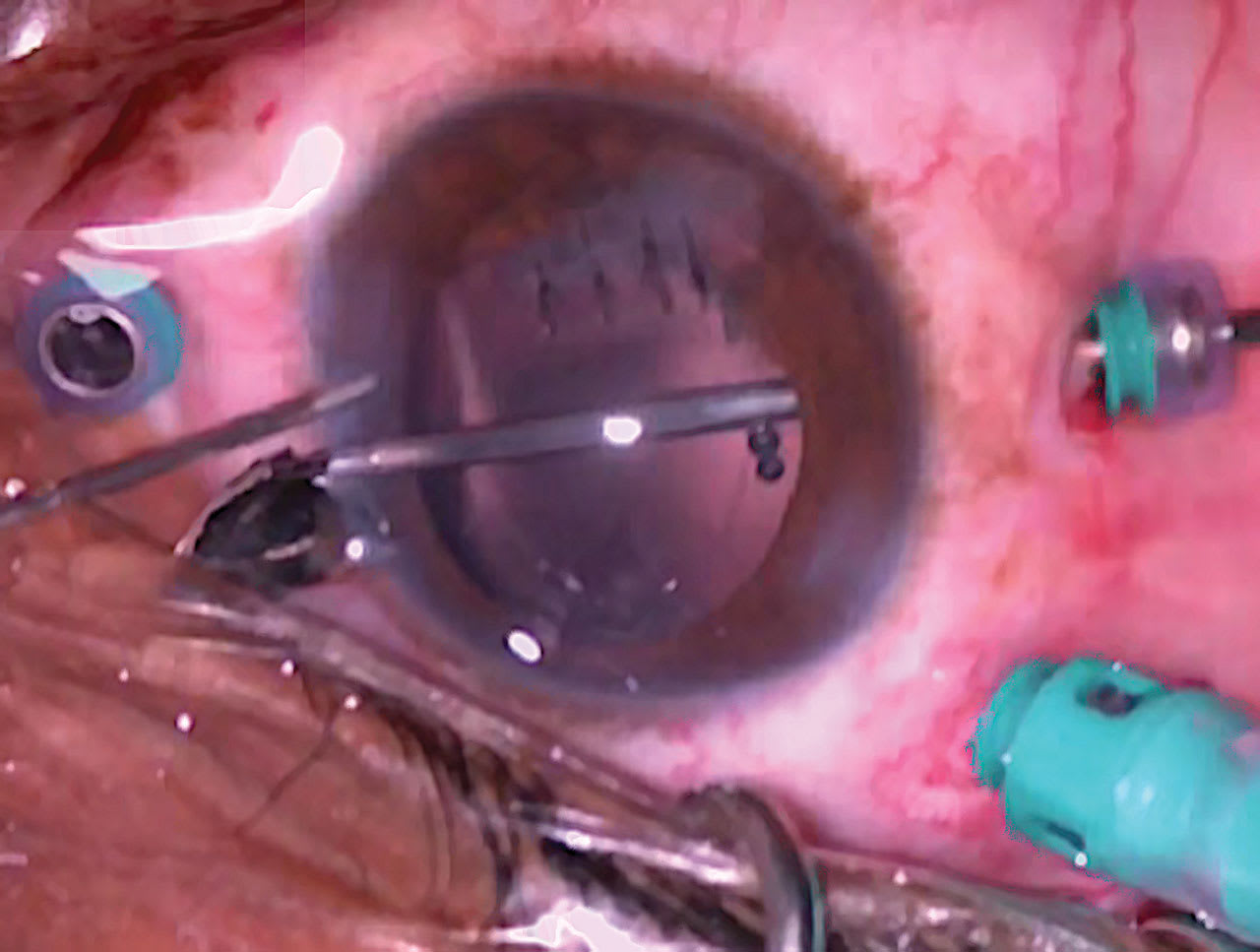
Figure 3. Using an instrument through the inferior port, the IOFB is pushed through a corneal incision.
Direct Delivery via Inferior Approach
A third technique involves using the inferior port to perform a pick-up-and-push maneuver (Figure 3). This approach requires repositioning the infusion line and inserting a suitable instrument inferotemporally, either through the inferotemporal trocar or a nearby sclerotomy. The foreign body is then grasped, elevated, and delivered directly through a superior limbal or scleral tunnel incision, eliminating the need to transfer it between instruments.
This method offers the advantage of avoiding the “handshake” transfer, thereby reducing the risk of dropping the IOFB. The optics of the globe remain stable until the moment of delivery, and fluid outflow from the opened incision helps facilitate extraction. This technique is especially useful for spherical foreign bodies, which are typically difficult to hand off and are better managed with a basket-type instrument.
However, this technique may require the surgeon to operate with the nondominant hand, which can be a limitation. Additionally, this technique is not suitable in lens-sparing scenarios, because it involves passing the IOFB through the anterior segment.
Tips for the Pick-Up-and-Push Technique
To optimize IOFB removal using the pick-up-and-push approach (Video 1), it is important to pre-plan the location of the inferotemporal trocar. The goal is to establish a straight, comfortable trajectory from this port to the superior clear corneal incision or scleral tunnel. The surgeon’s temporal hand must be able to lower sufficiently to allow the instrument tip to enter the anterior chamber. For patients with deep-set eyes or prominent orbital rims, a more temporal placement of the trocar paired with a more nasal exit wound may be required.
At the time of FB removal, the infusion line should be repositioned to the superotemporal trocar. Using the temporal hand, a suitable forceps or aspirating cannula is introduced through the inferotemporal trocar—or through a separate sclerotomy if a magnet or larger forceps is needed. The FB is grasped and elevated to the level of the pupil. Once the indirect viewing system is removed, the handle of the instrument is dropped below the iris plane to guide the FB into the anterior chamber. Maintaining the light pipe in its trocar during this step can provide counterforce and stabilize the globe.
As the FB approaches the inner aspect of the anterior segment incision, a second instrument or cannula is used to open the wound. The natural egress of fluid at this point assists in the FB’s delivery. Because the FB is already aligned with the internal wound edge at the moment of opening, visual disruption is minimized. This approach can be especially useful when corneal clarity is compromised, because it avoids the need to regrasp the FB in challenging anterior segment conditions.
If specialized forceps, an intraocular magnet, or a basket device is being used and cannot pass through the trocar, a separate scleral incision should be created near the inferotemporal port. This allows for direct access to the FB using the chosen instrument.
This method has certain limitations. It may require unconventional instrument angles and use of the non-dominant hand. However, when aspiration alone provides sufficient grip, these challenges can be mitigated. Notably, this technique is not suitable when preservation of the crystalline lens is necessary. RP
References
1. Bapaye M, Shanmugam MP, Sundaram N. The claw: a novel intraocular foreign body removal forceps. Indian J Ophthalmol. 2018;66(12):1845-1848. doi:10.4103/ijo.IJO_759_18
2. Singh R, Bhalekar S, Dogra MR, Gupta A. 23-gauge vitrectomy with intraocular foreign body removal via the limbus: an alternative approach for select cases. Indian J Ophthalmol. 2014;62(6):707-710. doi:10.4103/0301-4738.116458
3. Gonzalez-Cortes JH, Bages-Rousselon Y, Gonzalez-Cantu JE, Mohamed-Hamsho J. Minimally invasive surgery for the removal of posterior intraocular foreign bodies. J Ophthalmic Vis Res. 2017;12(2):236-240. doi:10.4103/jovr.jovr_109_16
4. Acar N. A new design intraocular foreign body forceps. Retina. 2017;37(12):2378-2380. doi:10.1097/IAE.0000000000001839
5. Yeh S, Colyer MH, Weichel ED. Current trends in the management of intraocular foreign bodies. Curr Opin Ophthalmol. 2008;19(3):225-233. doi:10.1097/ICU.0b013e3282fa75f1
6. Rice JC, Steffen J. Outcomes of eye injuries with retained intraocular foreign material at Groote Schuur Hospital, Cape Town. Trauma. 2016;18(4):276-282. doi:10.1177/1460408616640304
7. Baskaran P, Bhandari S, Govindarajan MV. Posterior vitrectorhexis: a surgical modification for intraocular foreign body removal through limbal route. Retin Cases Brief Rep. 2019;13(4):361-363. doi:10.1097/ICB.0000000000000598












