Rhegmatogenous retinal detachment (RRD) remains a vision-threatening emergency requiring timely surgical repair. Although pars plana vitrectomy (PPV) has become the preferred technique for many retinal surgeons, particularly in pseudophakic or complex cases, the role of scleral buckling (SB) in phakic patients is increasingly being reconsidered. Numerous meta-analyses, randomized trials, and registry studies now demonstrate that SB offers superior visual outcomes, reduced retinal displacement, and lower rates of postoperative cataract when compared to PPV in phakic eyes.1-3 Despite these advantages, SB usage has declined significantly in recent decades, largely due to shifts in training and surgical preferences. This trend raises important concerns about the long-term availability of SB expertise and its implications for patient care.4
Historical Overview
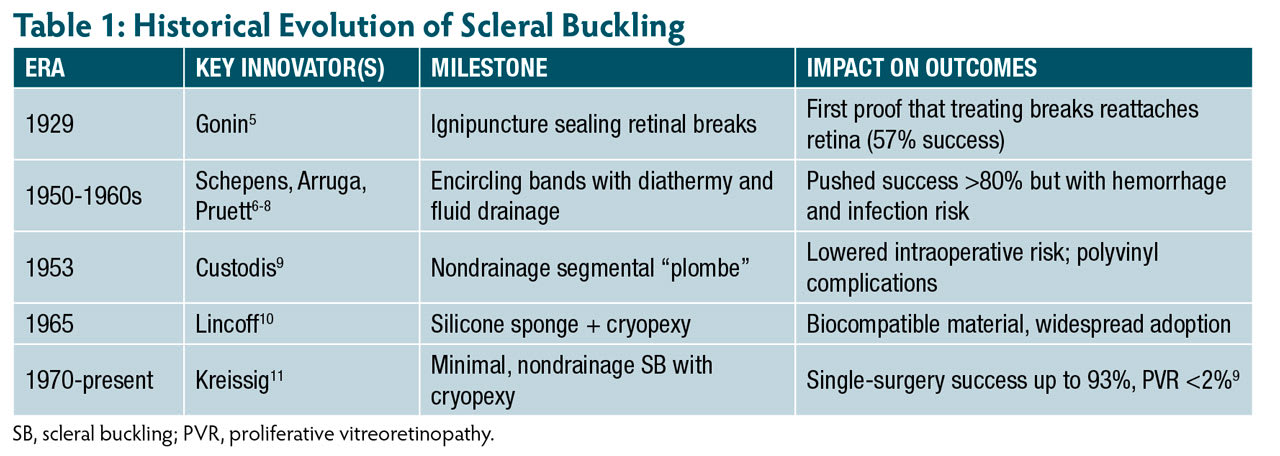
Scleral buckling has undergone a remarkable evolution since its inception in the early 20th century (Table 1). Jules Gonin’s landmark discovery in 1929 identified retinal breaks as the primary cause of RRD and introduced ignipuncture, achieving reattachment rates of 57%.5 In the 1950s and 1960s, Schepens, Arruga, and Pruett advanced the field with the encircling band (cerclage), using diathermy and subretinal fluid drainage to raise success rates above 80%, albeit with increased complication risks, including intraocular hemorrhage and endophthalmitis.6-8
Custodis introduced a nondrainage SB technique using a segmental elastic plombe and diathermy, reducing intraoperative risks but initially limited by material-related complications.9 In 1965, Lincoff refined this approach by replacing polyvinyl elements with silicone sponges and applying cryopexy, setting the foundation for modern SB.10 More recently, Kreissig and others have demonstrated that minimal, nondrainage SB can achieve single-surgery success rates up to 93%, with proliferative vitreoretinopathy (PVR) rates below 2%.11
Clinical Evidence
A robust body of literature supports SB as the preferred technique for phakic RRDs (Table 2). The Scleral Buckling vs Primary Vitrectomy in RRD study (SPR), a prospective randomized, multicenter trial, found that phakic eyes treated with SB had significantly better best-corrected visual acuity (BCVA) at 1 year compared to those treated with PPV (P=.0005). Cataract progression was notably higher in the PPV group.12
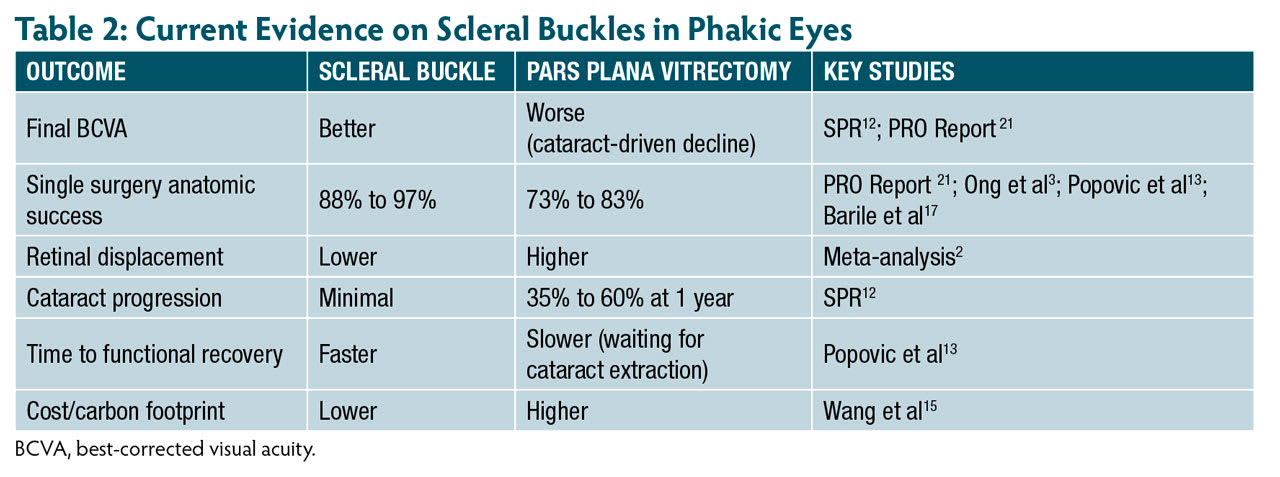
The Primary Retinal Detachment Outcomes (PRO) Study Report 2, a large multicenter analysis of nearly 3,000 eyes, confirmed these findings. Scleral buckling in phakic eyes achieved the best visual results and higher single surgery anatomic success (SSAS) rates (91.7% vs 83.1% for PPV).1 Real-world registry data further support SB’s superiority in uncomplicated detachments, reporting SSAS rates of 80.3% for SB vs 72.8% for PPV.3
Meta-analyses of more than 15,000 eyes show SB results in better visual outcomes, faster visual rehabilitation, and lower cataract risk than PPV, with similar or higher SSAS rates.2,13 Scleral buckling is also associated with less retinal displacement, which has been linked to reduced dysphotopsias and better postoperative quality of vision.2 Large, aggregated data—15,947 eyes in a 2022 meta-analysis—confirm that SB in phakic RRDs achieves equal or superior anatomic success with better visual outcomes than PPV.2
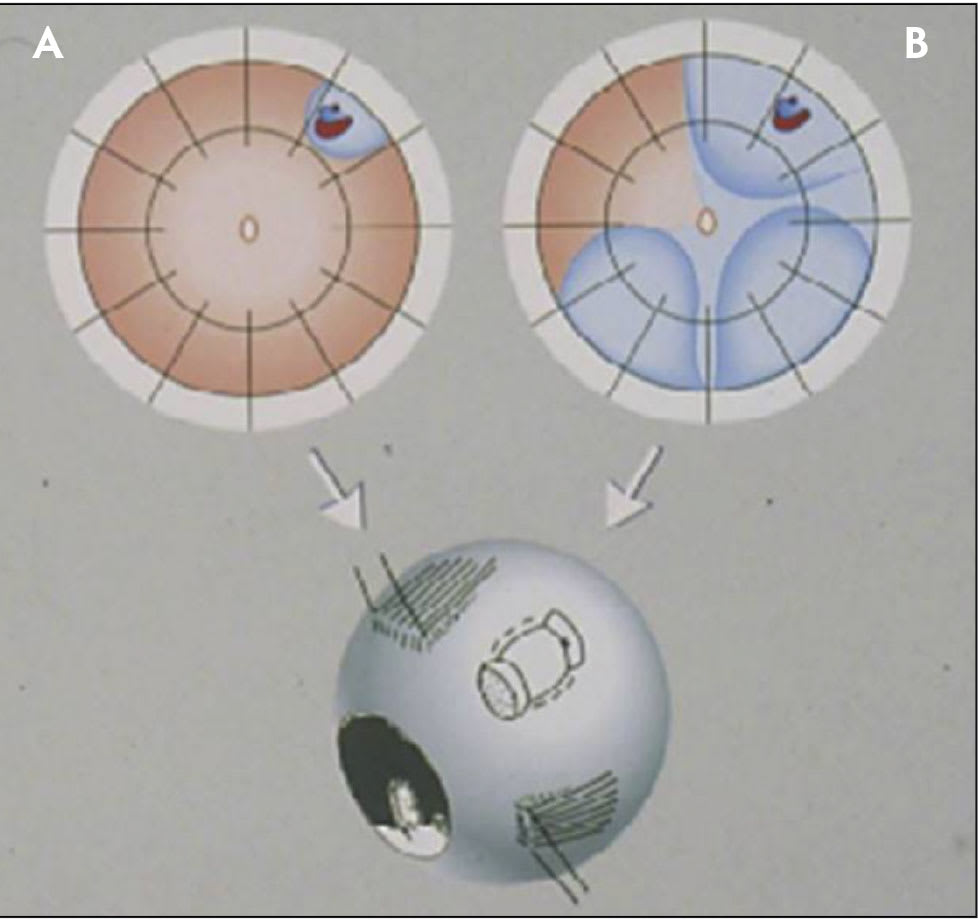
Figure 1. For minimal segmental buckling without drainage, so-called extraocular minimal surgery, the treatment is limited to the area of the break and not determined by the extent of the detachment. The small (A) and the more extensive detachment (B) are caused by the same horseshoe tear at 1 o’clock. The treatment of both detachments is the same, consisting of buckling the tear either by a segmental sponge (as depicted) or a temporary balloon without drainage of subretinal fluid. From Kreissig I. A Practical Guide to Minimal Surgery for Retinal Detachment: Diagnostics, Segmental Buckling Without Drainage, Case Presentations. Stuttgart, Germany: Thieme; 1999. Reprinted with permission.
Technical Refinements
Modern SB techniques have greatly improved in precision, safety, and reproducibility. One of the most impactful innovations is the adoption of nondrainage minimal SB, particularly using segmental or radial silicone sponges. These elements allow surgeons to customize the degree and location of indentation based on the configuration and number of retinal breaks. The compressible nature of silicone sponges facilitates controlled and broad indentation while minimizing focal stress on the sclera (Figure 1, Figure 2).
Avoiding subretinal fluid drainage significantly reduces the risk of serious complications such as globe perforation, intraocular hemorrhage, retinal incarceration, and endophthalmitis. These nondrainage methods also reduce axial elongation and myopic shift, preserving refractive integrity in phakic eyes. They further mitigate the risk of anterior-segment ischemia.
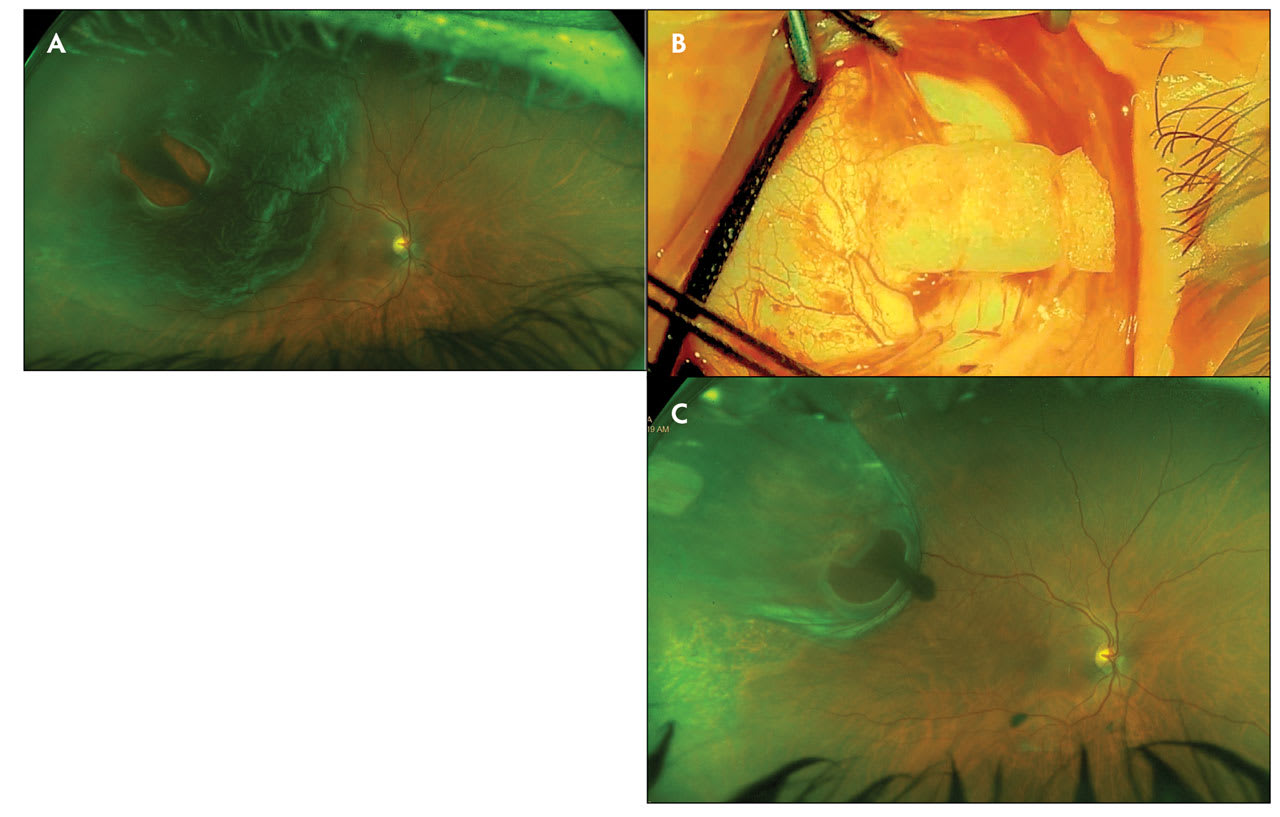
Figure 2. Preoperative Optos image of right eye of a 61-year-old female who presented with visual acuity 20/400 and rhegmatogenous retinal detachment (A). Intraoperative image of radial sponge placement (B). Two weeks after radial buckle and cryotherapy scleral buckle surgery, visual acuity in the right eye has improved to 20/30 (C).
Visualization tools have evolved in parallel. The key to success in SB surgery is visualizing and identifying all the breaks and treating them. Traditional SB depended heavily on indirect ophthalmoscopy and loupes. However, the integration of wide-angle viewing systems, chandelier-assisted endoillumination, and operating microscopes now enables panoramic retinal visualization and optimized viewing for the surgeon and assistants. These tools enhance accuracy in locating breaks, administering cryotherapy, and confirming buckle placement.
Furthermore, video recording and digital overlays facilitate intraoperative teaching, improving SB training and adoption.11,14 Global educational initiatives, such as Kreissig’s more than 130 nondrainage SB training courses, have helped restore proficiency by promoting minimally invasive techniques.11 Web conferencing with surgical videos has evolved as a superb teaching tool to reach anyone with online connectivity.
Patient Selection Considerations
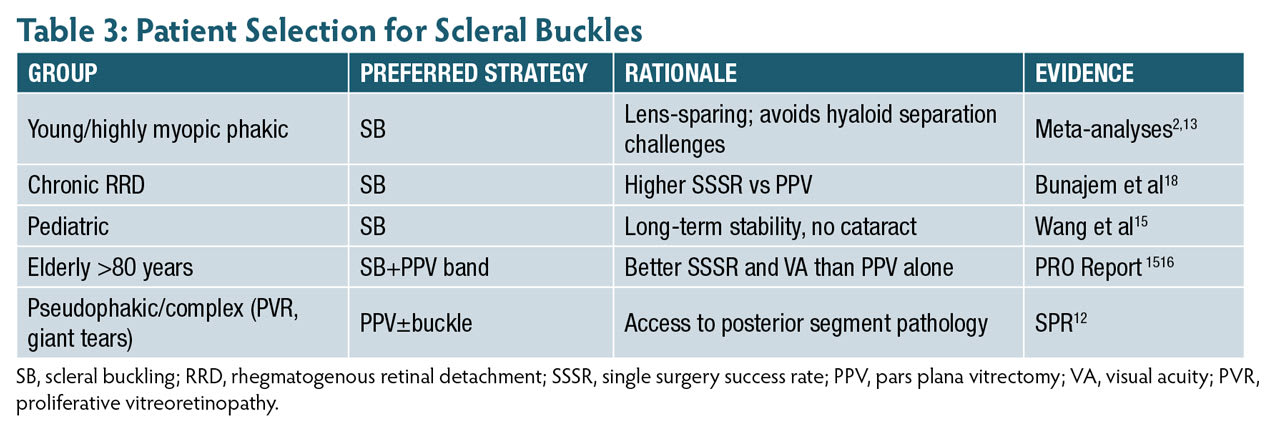
Scleral buckling remains particularly advantageous in specific patient populations (Table 3). In young, phakic individuals, SB preserves the crystalline lens and avoids the technical challenges of hyaloid separation required in PPV. In chronic or pediatric RRDs, SB has shown superior anatomic and functional outcomes.15 The PRO 15 study suggests that in patients over 80 years of age, combining SB with PPV yields higher SSAS rates and better visual outcomes than PPV alone.16
Contraindications to encircling SB include ischemic ocular conditions, thin sclera, or prior surgeries such as strabismus repair where anatomic limitations exist. In such cases, segmental buckles or PPV may be more appropriate.
Conclusion
Despite the increasing dominance of PPV in retinal detachment repair, scleral buckling continues to offer superior outcomes in phakic RRD. Its benefits—preserved lens clarity, faster recovery, fewer complications, and lower costs—make it an essential part of the vitreoretinal surgeon’s armamentarium. As evidence mounts and surgical tools advance, maintaining and restoring SB proficiency must be a priority in fellowship programs and clinical practice alike. RP
References
1. Ryan EH, Ryan CM, Forbes NJ, et al. Primary Retinal Detachment Outcomes study report number 2: phakic retinal detachment outcomes. Ophthalmology. 2020;127(8):1077-1085. doi:10.1016/j.ophtha.2020.03.007
2. Dhoot AS, Popovic MM, Nichani PAH, et al. Pars plana vitrectomy vs scleral buckle: a comprehensive meta-analysis of 15,947 eyes. Surv Ophthalmol. 2022;67(4):932-949. doi:10.1016/j.survophthal.2021.12.005
3. Ong SS, Ahmed I, Gonzales A, et al. Management of uncomplicated rhegmatogenous retinal detachments: a comparison of practice patterns and clinical outcomes in a real-world setting. Eye (Lond). 2023;37(4):684-691. doi:10.1038/s41433-022-02028-z
4. Fallico M, Alosi P, Reibaldi M, et al. Scleral buckling: a review of clinical aspects and current concepts. J Clin Med. 2022;11(2):314. doi:10.3390/jcm11020314
5. Gonin J. Ignipuncture and treatment of retinal detachment. Ann Ocul (Paris). 1930.
6. Schepens CL. Retinal Detachment and Allied Diseases. Vol 1–3. W.B. Saunders Company; 1983.
7. Arruga H. Encircling techniques in retinal detachment. Arch Ophthalmol. 1958.
8. Pruett RC. Complications associated with scleral buckling procedures. Int Ophthalmol Clin. 1976;16(2):215-229.
9. Custodis E. Treatment of retinal detachment by scleral indentation without drainage of subretinal fluid. Ber Zusammenkunft Dtsch Ophthalmol Ges. 1953;58:102-105.
10. Lincoff H, Kreissig I. Segmental buckling without drainage. Trans Am Acad Ophthalmol Otolaryngol. 1965;69:577-583.
11. Kreissig I. A 50-year review of minimal extraocular surgery. Eye (Lond). 2020;34(2):285-289. doi:10.1038/s41433-019-0683-9
12. Heimann H, Bartz-Schmidt KU, Bornfeld N, et al. Scleral buckling vs primary vitrectomy in rhegmatogenous retinal detachment: a prospective randomized multicenter clinical study. Ophthalmology. 2007;114(12):2142-2154. doi:10.1016/j.ophtha.2007.09.013
13. Popovic MM, Muni RH, Nichani P, Kertes PJ. Pars plana vitrectomy, scleral buckle, and pneumatic retinopexy for the management of rhegmatogenous retinal detachment: a meta-analysis. Surv Ophthalmol. 2022;67(1):184-196. doi:10.1016/j.survophthal.2021.05.008
14. Cruz-Pimentel M, Huang CY, Wu L. Scleral buckling: a look at the past, present, and future in view of recent findings on the importance of photoreceptor realignment following retinal reattachment. Clin Ophthalmol. 2022;16:1971-1984. doi:10.2147/OPTH.S359309
15. Wang KY, Adams OE, Yu MD, Yonekawa Y. The necessity and role of scleral buckling for rhegmatogenous retinal detachment. Curr Opin Ophthalmol. 2024;35(5):376-381. doi:10.1097/ICU.0000000000001065
16. Starr MR, Ryan EH, Yonekawa Y. Primary retinal detachment outcomes study: summary of reports number 1 to number 18. Curr Opin Ophthalmol. 2023;34(3):211-217. doi:10.1097/ICU.0000000000000942
17. Barile GR, Gupta R, Engelbert M et al. Nondrainage scleral buckling in the modern vitrectomy era. Retina. 2025;45(6):1070-1075. doi:10.1097/IAE.00000000000004428.
18. Bunajem M, Ahmad K, Al Zaidi N, Al Bloushi B, Al Zahrani Y. Scleral buckle versus pars plana vitrectomy in the management of primary chronic rhegmatogenous retinal detachment: a comparison of anatomical and visual outcomes. Middle East Afr J Ophthalmol. 2021;28(2):65-70. doi:10.4103/meajo.MEAJO_441_20










