Early data from a first-in-human trial of the Luca robotic system for vitreoretinal surgery demonstrates that robotic assistance may improve surgical precision and reproducibility without compromising patient safety. Fanny Nerinckx, MD, presented the early results at the 2025 Retina World Congress in Fort Lauderdale, Florida. She described the study as an initial proof of concept that supports the feasibility of robotic vitreoretinal surgery using commercially available instruments.
“Robots could overcome our limitations and eventually in the future we’ll be able to perform procedures we are not able to perform now,” Dr. Nerinckx, a senior vitreoretinal surgeon at Ghent University Hospital in Belgium and Chirec-Delta Hospital in Brussels, said during her presentation. She cited vascular cannulation and subretinal injections requiring sustained stability as examples of procedures that could one day be performed by robotic systems.
The Luca system, developed by French start-up Acusurgical, uses 2 robotic arms positioned on either side of the patient’s head. It is designed to translate surgeon gestures from a piloting station to the surgical field with precision up to 10 µm (Figure 1). Unlike some earlier robotic systems, Luca is intended to support full vitreoretinal surgeries rather than single-step procedures.
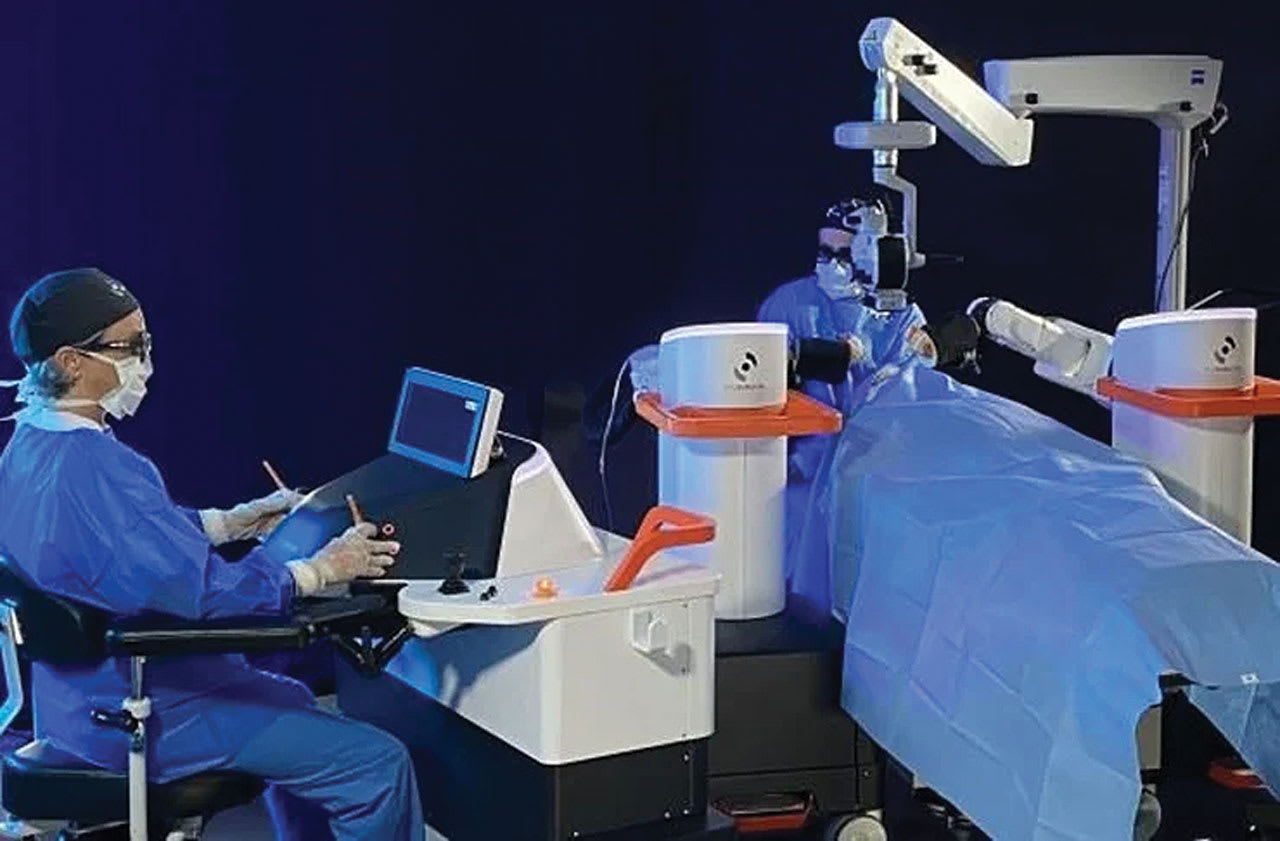
Figure 1. The Luca robotic system includes 2 independent robotic arms, which the surgeon controls from an ergonomic piloting station to ensure stability and accuracy.
Addressing Human Limitations
Dr. Nerinckx emphasized that robotic systems may help overcome fundamental human limitations in microsurgery—especially for tasks that require extremely precise motor control. Traditional retinal surgery involves working within spaces only fractions of a millimeter wide, on delicate structures such as the macula or retinal blood vessels. Challenges for human surgeons include physiologic tremors, reduced fine motor control over time, and limited depth perception during visualization.
“We have an intrinsic tremor of about 200 µm, and we have to manipulate tissues that we sometimes don’t even sense,” she said. “The reproducibility of the surgeries is really difficult, and there is a large learning curve.”
Dr. Nerinckx cited evidence from wet lab testing that demonstrated smoother and faster tool trajectories when using the Luca system compared to manual techniques (Figure 2). The system allows the use of standard disposable surgical instruments, including subretinal cannulas, and integrates with common 3D visualization platforms.
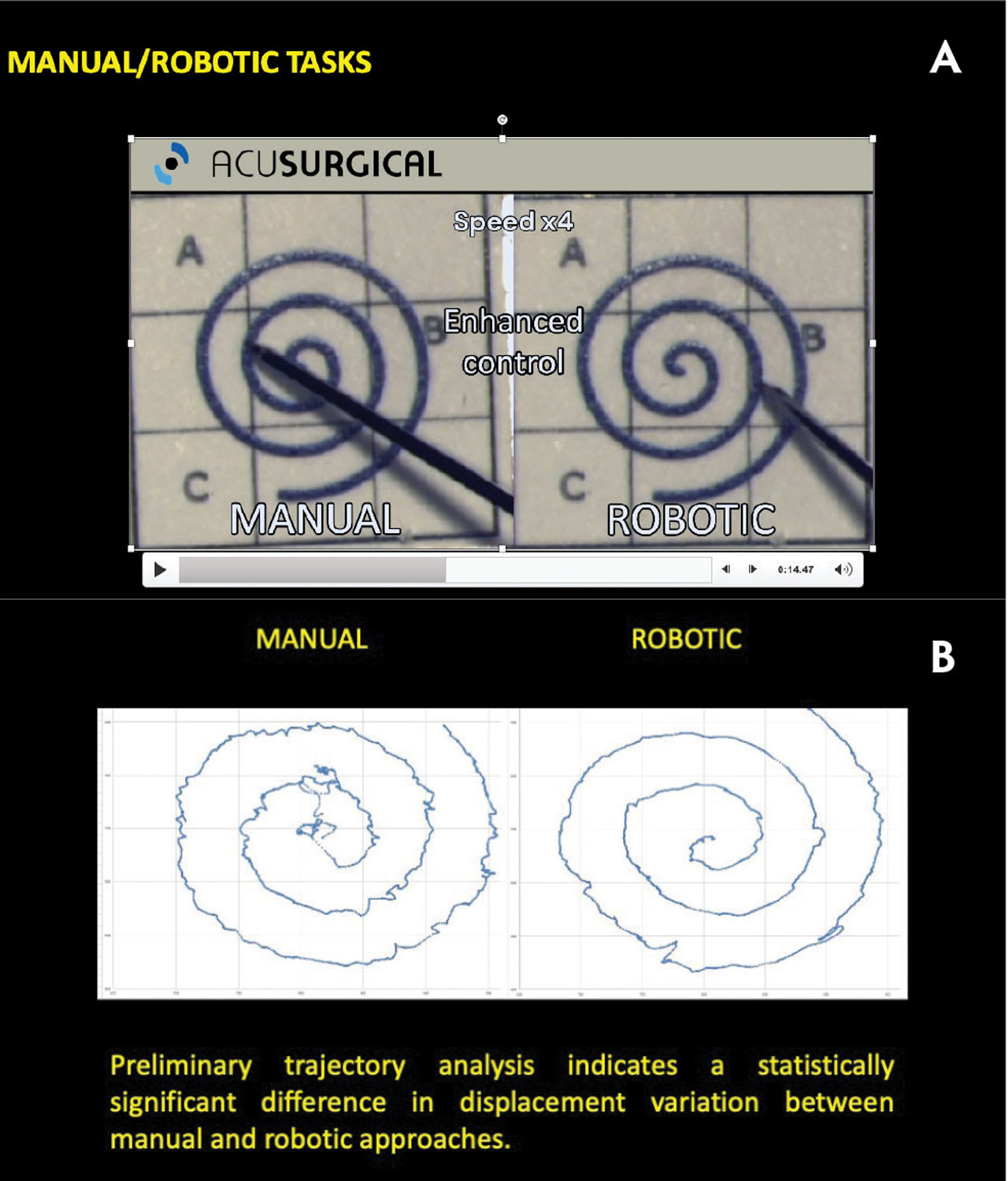
Figure 2. The diameter of a retinal vein is 120 µm, while the human hand has an intrinsic tremor of 200 µm. The Luca system can operate with 20 times less tremor than a human, reported Fanny Nerinckx, MD, enabling greater surgical precision.
Ongoing Clinical Trial
The Luca system is being evaluated in a prospective, interventional, open-label, noncontrolled trial in Belgium. The study is still enrolling, with plans for up to 15 evaluable subjects undergoing vitreoretinal surgery to treat intravitreal hemorrhage and macular pucker. The primary outcome relates to the safety of the robotic surgical system, with an assessment of the incidence and severity of adverse events that were definitely or probably related to the investigational device over a 3-month period.
During the Retina World Congress, Dr. Nerinckx presented data on 6 patients who underwent vitrectomy or posterior vitreous detachment (PVD) induction for macular pathology. One case involved a macular hole. All procedures were completed successfully using the robotic system, and no adverse events related to the device were observed, she said.
In all 6 procedures, Luca reproduced the surgeon’s intended gestures. “I felt actually more accurate with the robot in 4 out of 6 patients,” Dr. Nerinckx noted (Video 1, Video 2). She added that the robotic system prevented abrupt movements, which could otherwise risk damaging sensitive retinal structures.
Workflow and Safety
Although robotic setup is more time-consuming than manual surgery, Dr. Nerinckx described the process as manageable. “To set up the system for the very first surgery, it takes about 30 minutes,” she explained. “But once you start the surgical sessions, in between sessions you just have to move 1 pod so the patient can leave the OR and you can bring in the next patient.”
For the initial trial, all patients were under general anesthesia and their heads were stabilized using surgical tape. Dr. Nerinckx noted that future studies will explore the use of Luca under local anesthesia, aided by a patient movement detection feature to address intraoperative motion. This feature is currently in development.
The Luca system also includes a safety override, allowing the surgeon to immediately regain manual control of the instrument if needed.
Standardization and Training
Among the potential long-term advantages of robotic systems are improved surgical reproducibility, lower complication rates, and reduced training burdens. Dr. Nerinckx cited standardization of technique and a shorter learning curve for fellows as key benefits.
“Robots could eventually help us train fellows more efficiently,” she said. “And in the future, robots may allow us to perform procedures we currently avoid due to risk.”
A multicenter study is planned to further evaluate the precision and clinical utility of the Luca system. Future iterations are also expected to incorporate enhanced imaging, artificial intelligence–based guidance, and real-time tissue interaction monitoring.
Although still early, the Luca trial marks a key milestone in bringing robotic assistance into routine retinal care. “It was feasible to perform VR surgery with the Luca robot,” Dr. Nerinckx said. “We had an initial positive and safe profile.”
For now, the technology remains investigational. But with rapid advances in robotics and imaging, Dr. Nerinckx and colleagues see the potential for a more standardized, ergonomic, and precise surgical future. RP








