Macular telangiectasia (MacTel) is a capillary disorder affecting the fovea and central retina. It has also been called idiopathic juxtafoveal or perifoveal telangiectasia. Researchers have broadly described 2 manifestations, type 1 and type 2. Type 1 MacTel is often a developmental or congenital disease limited to 1 eye, and is a part of a wider range of vascular disease characteristics found in Coats disease. Type 2 MacTel is a bilateral variant present in middle-aged and elderly persons, is likely acquired, and is the predominant form encountered in a retina clinic. This article will focus on type 2 MacTel.
In large epidemiologic studies, MacTel was found in 0.1% of the population with an average age of 63 years at time of identification.1 Given bilateral presentation, some evidence suggestive of vertical transmission and high incidence among monozygotic twins there has been a suspicion of genetic influence.3-5 However, a single candidate causative genetic change has not been discovered.6
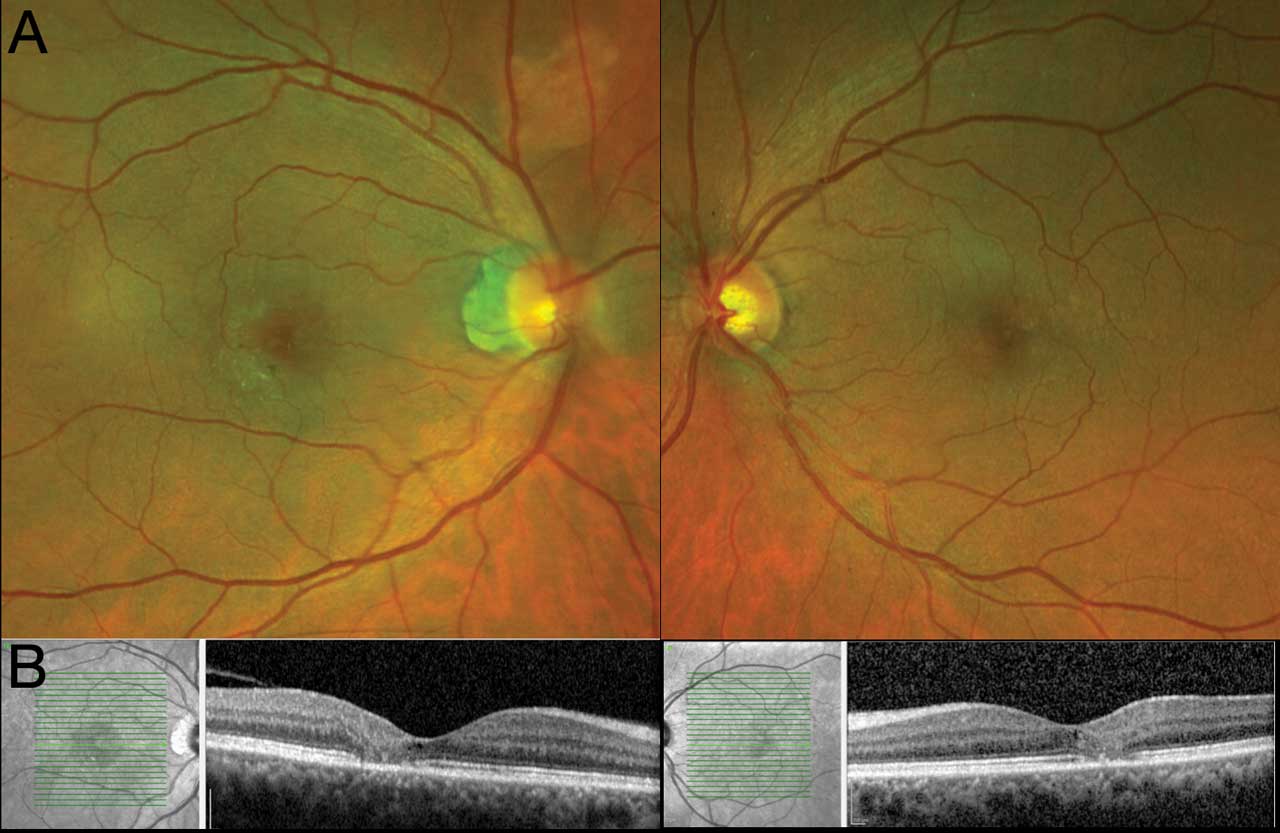
In the initial stages of the disease, the area temporal to the fovea becomes less transparent, affecting 1 eye more than the other. Vision is generally unaffected. However, over decades, the retinal vasculature that supplies the fovea and perifovea develop ectactic capillaries, crystalline deposits, and hard exudates. There can be retinal pigment epithelium (RPE) cell migration and atrophy of all layers of the retina (Figure 1). The final resulting vision tends to be in the 20/60 range, although many can develop such substantial atrophy or injury due to reactive neovascularization producing approximately 20/200 vision.
There is no FDA-approved intervention to arrest the progression of atrophy in MacTel, although research into the potential of ciliary neurotrophic factor (CNTF) is ongoing. A phase 2 randomized trial investigating CNTF compared with placebo in 99 eyes was published in 2019.2 It met its primary endpoint at 24 months demonstrating a rate of 0.22 mm2 photoreceptor loss in the group receiving CNTF, which was statistically less than 0.27 mm2 rate of progression in the sham group. There was 31% greater progression of neurodegeneration in the latter group. The phase 3 study of the same molecule has recently completed enrollment including 115 participants in 22 centers with the same study design.7 The last update from this study was from February 2023, but no results have been published.
Neovascularization
In some cases, patients may demonstrate neovascular events or exudative consequences of neovascularization, including intraretinal thickening or subretinal or intraretinal hemorrhage. One result of these processes can be disciform scarring if untreated and can lead to significant deterioration in vision. This form of MacTel has also been called “proliferative” MacTel.
Neovascular structures that develop in MacTel differ from those more commonly encountered in retinal clinics for conditions such as neovascular age-related macular degeneration (AMD), where the origin of neovessels is in the choroid. In MacTel, subretinal neovascularization is believed to originate from the deeper retinal circulation.19 There are connections between different layers of the retina, including retinal-retinal and retinal-subretinal anastomoses. Adjacent to these connections, there are expanded and leaking aneurysms that trigger the growth of new vessels. In most cases, a patient’s visual acuity declines significantly from baseline when neovascularization occurs, and clinical examinations may reveal visible intraretinal or subretinal bleeding (Figure 2). Studies such as fluorescein angiography (FA) and optical coherence tomography (OCT) can detect exudative aneurysms and reactive neovessels. Additionally, the presence of subretinal and intraretinal fluid that wasn’t present before the onset of neovascularization becomes apparent (Figure 3).


Reviewing existing literature can provide insight into the potential prevalence of neovascularization. In 2006, Yanuzzi et al reported 36 patients diagnosed with MacTel over a 3-year period. Of these patients, 10 eventually developed “aneurysmal” telangiectasia or neovascularization. The timeframe between presentation and diagnosis of neovascular disease was not described.8 Another study by Gass and Blodi reviewed 182, eyes 25 of which progressed to stage 5 or a neovascular state.9 Among 72 patients followed for 2 years or longer (range 24 to 316 months, mean 91 months), 37 experienced legal blindness (20/200 or worse). This was primarily attributed to foveal atrophy in 26 cases, neovascularization in 10, and cataract in 1. Other epidemiologic studies have been published but have only made a diagnosis distally with the use of color photos, which may give an incomplete assessment of the prevalence and incidence of neovascularization.1,10,11 Therefore, what limited information is available seems to indicate that neovascularization may occur in as much as 13% of reported populations.
In cases of neovascular disease, treatment may not always be necessary. In situations where fibrovascular proliferation damages photoreceptors, attempting to reduce exudation might not be effective, similar to the situation in chronic, inactive neovascular AMD following foveal or macular damage. Inactive yet neovascular MacTel type 2 disease cases with acuity of 20/200 or worse were reviewed in 1 study and treated; no functional changes were observed over time when intervention was not considered feasible for improvement.12 This suggests that, akin to neovascular AMD patients, early intervention before fibrosis sets in is crucial.
Photodynamic therapy (PDT) was among the first nondestructive approaches tested for neovascular MacTel. The largest study included 6 patients who received an average of 2.4 treatments based on a standardized protocol. The mean follow-up time after the last treatment was 21 months, and visual acuity showed stability in 5 out of 6 eyes.13
With the introduction of anti-VEGF therapies, numerous studies have explored their effectiveness. The most extensive study available was a retrospective case series involving 16 treatment-naive eyes of 16 patients. They were treated with intravitreal ranibizumab or bevacizumab monotherapy, with a mean of 1.9 injections needed during a mean follow-up of 12 months.14 Visual acuity improved significantly from 20/120 to 20/70. There have also been reports of combining PDT with ranibizumab, with 1 patient experiencing visual acuity improvement from 20/125 to 20/60 within a 9-month follow-up period.15,16
Compared to the extensive studies conducted for neovascular AMD, the evidence for MacTel is less robust. It’s important to note that all treatments have been used off-label. Nonetheless, the author’s experience aligns with improved visual function when treating the neovascular lesion before fibrosis develops (Figure 3). When encountering a patient with MacTel type 2, the author’s preference is to recommend semiannual screening using angiography and OCT, along with the use of an Amsler grid at home. By informing patients about the potential for vision loss, the likelihood of permanent damage to vision might be reduced through enhanced understanding and accurate diagnosis.
Conclusion
Macular telangiectasia type 2 is a spontaneous, sporadic retinal vascular disorder that is present in 0.1% of the US population, affecting both eyes asymmetrically. While there may be indications of heritability, so far no specific genetic mutation has been described as its primary cause. Most patients who develop vision loss have atrophy for which medical therapies may be available in the future, but none are FDA approved currently. Neovascular complications can occur in as much as 10% of patients with the condition and can be treated with currently available options including anti-VEGF injection and photodynamic therapy. Screening and surveillance are important aspects in the care of patients with this diagnosis. RP
References
- Klein R, Blodi BA, Meuer SM, Myers CE, Chew EY, Klein BE. The prevalence of macular telangiectasia type 2 in the Beaver Dam eye study. Am J Ophthalmol. 2010;150(1):55-62.e2. doi:10.1016/j.ajo.2010.02.013
- Chew EY, Clemons TE, Jaffe GJ, et al. Effect of ciliary neurotrophic factor on retinal neurodegeneration in patients with macular telangiectasia type 2: a randomized clinical trial. Ophthalmology. 2019;126(4):540-549. doi:10.1016/j.ophtha.2018.09.041
- Gillies MC, Zhu M, Chew E, et al. Familial asymptomatic macular telangiectasia type 2. Ophthalmology. 2009;116(12):2422-2429. doi:10.1016/j.ophtha.2009.05.010
- Chew EY, Murphy RP, Newsome DA, Fine SL. Parafoveal telangiectasis and diabetic retinopathy. Arch Ophthalmol. 1986;104(1):71-75. doi:10.1001/archopht.1986.01050130081025
- Parmalee NL, Schubert C, Figueroa M, et al. Identification of a potential susceptibility locus for macular telangiectasia type 2. PLoS One. 2012;7(8):e24268. doi:10.1371/journal.pone.0024268
- Parmalee NL, Schubert C, Merriam JE, et al. Analysis of candidate genes for macular telangiectasia type 2. Mol Vis. 2010;16:2718-2726.
- ClinicalTrials.gov Identifier: NCT03316300
- Yannuzzi LA, Bardal AM, Freund KB, Chen KJ, Eandi CM, Blodi B. Idiopathic macular telangiectasia. Arch Ophthalmol. 2006;124(4):450-460. doi:10.1001/archopht.124.4.450
- Gass JD, Blodi BA. Idiopathic juxtafoveolar retinal telangiectasis: update of classification and follow-up study. Ophthalmology. 1993;100(10):1536-1546.
- Aung KZ, Wickremasinghe SS, Makeyeva G, Robman L, Guymer RH. The prevalence estimates of macular telangiectasia type 2: the Melbourne Collaborative Cohort study. Retina. 2010;30(3):473-478. doi:10.1097/IAE.0b013e3181bd2c71
- Sallo FB, Leung I, Mathenge W, et al. The prevalence of type 2 idiopathic macular telangiectasia in two African populations. Ophthalmic Epidemiol. 2012;19(4):185-189. doi:10.3109/09286586.2011.638744
- Engelbrecht NE, Aaberg TM Jr, Sung J, Lewis ML. Neovascular membranes associated with idiopathic juxtafoveolar telangiectasis. Arch Ophthalmol. 2002;120(3):320-324. doi:10.1001/archopht.120.3.320
- Potter MJ, Szabo SM, Sarraf D, Michels R, Schmidt-Erfurth U. Photodynamic therapy for subretinal neovascularization in type 2A idiopathic juxtafoveolar telangiectasis. Can J Ophthalmol. 2006;41(1):34-37. doi:10.1016/S0008-4182(06)80063-3
- Narayanan R, Chhablani J, Sinha M, et al. Efficacy of anti-vascular endothelial growth factor therapy in subretinal neovascularization secondary to macular telangiectasia type 2. Retina. 2012;32(10):2001-2005. doi:10.1097/IAE.0b013e3182625c1d
- Rishi P, Shroff D, Rishi E. Combined photodynamic therapy and intravitreal ranibizumab as primary treatment for subretinal neovascular membrane (SRNVM) associated with type 2 idiopathic macular telangiectasia. Graefes Arch Clin Exp Ophthalmol. 2008;246(4):619-621. doi:10.1007/s00417-007-0732-0
- Ruys J, De Laey JJ, Vanderhaeghen Y, Van Aken EH. Intravitreal bevacizumab (Avastin) for the treatment of bilateral acquired juxtafoveal retinal telangiectasis associated with choroidal neovascular membrane. Eye (Lond). 2007;21(11):1433-1434. doi:10.1038/sj.eye.6702946
- Chew EY, Clemons TE, Jaffe GJ, et al. Effect of ciliary neurotrophic factor on retinal neurodegeneration in patients with macular telangiectasia type 2: a randomized clinical trial. Ophthalmology. 2019;126(4):540-549. doi:10.1016/j.ophtha.2018.09.041
- Zhang Q, Wang RK, Chen CL, et al. Swept source optical coherence tomography angiography of neovascular macular telangiectasia type 2. Retina. 2015;35(11):2285-2299. doi:10.1097/IAE.0000000000000840









