Key Takeaways
- Recent advancements in surgical techniques, such as autologous retinal transplant (ART) and amniotic membrane graft (AMG), have improved outcomes for treating complicated macular holes, particularly those that are refractory to initial surgery.
- Scaffold-based approaches like ART and AMG, along with expansion-based techniques involving subretinal blebs, offer tailored solutions to achieve better anatomic and functional outcomes in eyes with large or complicated macular holes.
- The retracting-door internal limiting membrane (ILM) flap technique helps preserve ILM for potential future use and reduces the risk of flap displacement, making it a useful method for first-time macular hole surgeries.
Since the original report by Kelly and Wendel in 1991, macular hole surgery has become one of the most successful vitreoretinal surgeries.1 Although treatment approaches have improved over the last 30 years and surgeons are routinely able to achieve >90% closure rates in typical macular holes, large complicated macular holes, particularly refractory macular holes, remain a challenge due to lower anatomic closure rates with conventional approaches.
An area of focus over the past decade has been to improve surgical techniques in eyes with complicated macular holes wherein prognosis for successful macular hole closure and improved visual acuity is less favorable. Complicated macular holes are typically defined as those associated with high myopia (often with concurrent posterior staphyloma), retinal detachment, genetic conditions such as Alport Syndrome, or refractory macular holes. Refractory macular holes are those where the hole remains open despite adequate removal of the internal limiting membrane (ILM) and gas tamponade during initial surgery.2 When a macular hole does not close after an initial surgery, the macular hole is more difficult to treat because the ILM already has been removed either partially or completely around the macular hole.
New Techniques
Recent advancements to the surgical armamentarium have provided more options to achieve better anatomic and functional outcomes in these eyes. For refractory macular holes, surgeons can adopt either a scaffold-based approach or a macular expansion‒based approach. Scaffold based approaches include the autologous retinal transplant (ART), amniotic membrane graft (AMG), or ILM flap or graft.3,4 Expansion-based approach includes subretinal blebs, often with adjunct macular mobilization performed with an instrument such as a nitinol loop.5
In the absence of significant chorioretinal scarring, retinal ischemia, or in an adult eye, some surgeons prefer the ART approach. The key tip in ART is to select a harvest site that is easily accessible. Using a vertical scissors the graft is created, which is typically about 25% larger than the size of the hole, and a small island is left attached. Perfluorocarbon is then placed to beyond the anterior edges of the harvest site and a forceps such as the MaxGrip forceps (Alcon) is used to hold the graft, sever the residual attached area, and mobilize it toward the macular hole under perfluorocarbon. Performing this maneuver under perfluorocarbon facilitates visualization and orientation of the graft as well as confirmation of its placement over the macular hole.
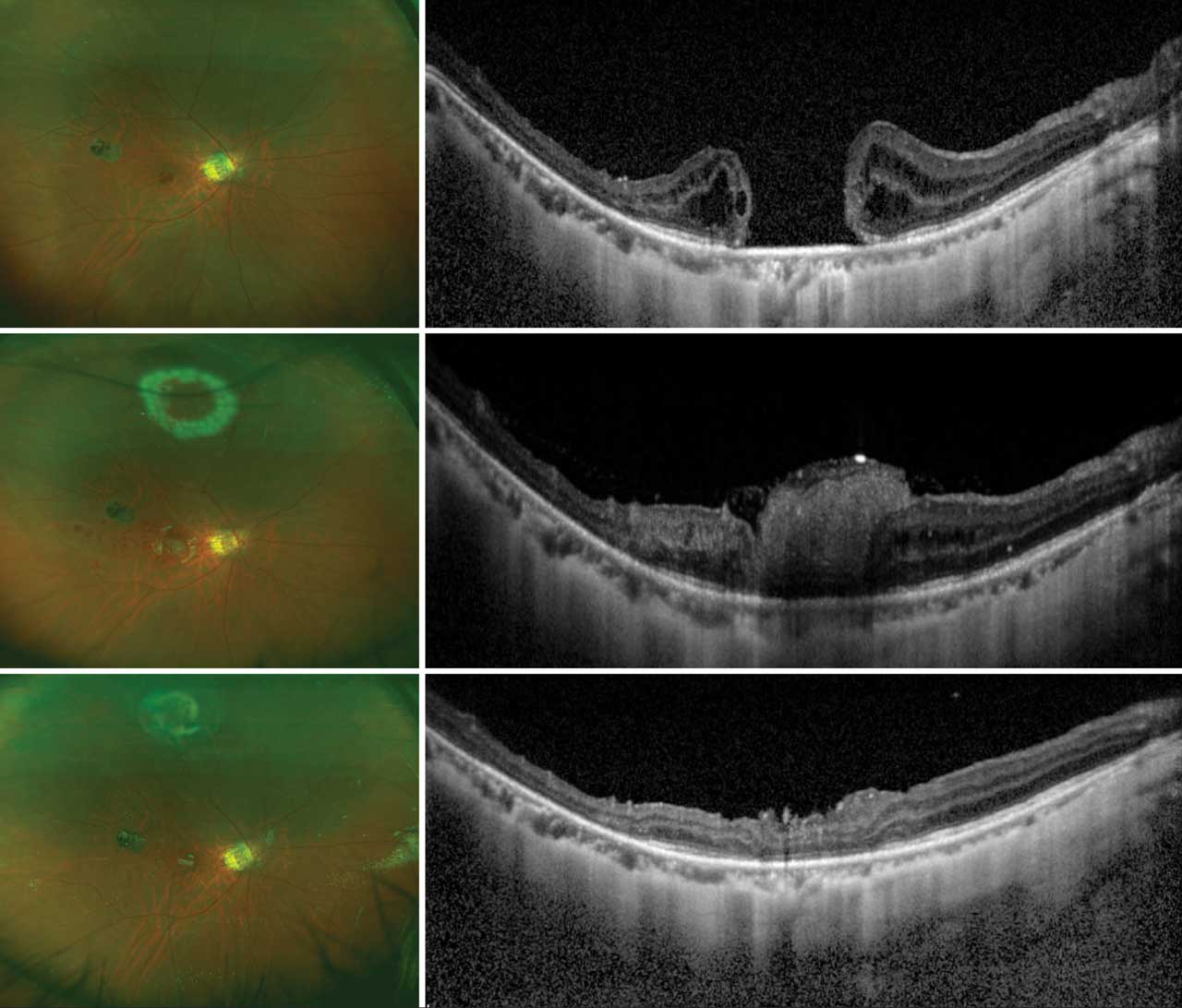
Silicone oil tamponade can be useful for ART cases (a direct perfluorocarbon to silicone oil exchange can be performed), with removal of the oil at 4 to 6 weeks postoperatively. In myopic eyes with a deep posterior staphyloma, adjunctive platelet rich plasma (prepared by centrifuging venous blood obtained from the antecubital vein intraoperatively) can be used to secure the ART in position intraoperatively. This can, anecdotally, help reduce risk of ART graft displacement.6 Unlike other procedures in which scaffolds are used to help macular tissue movement to close the hole, ART bridges the gap by adding retinal tissue that has potential to integrate within the macular tissue and closes the hole. Better final visual outcome following ART is associated with hole closure, reconstitution of the ellipsoid zone, and alignment of the neurosensory layers between grafted peripheral retina and macular tissue (Figure 1).
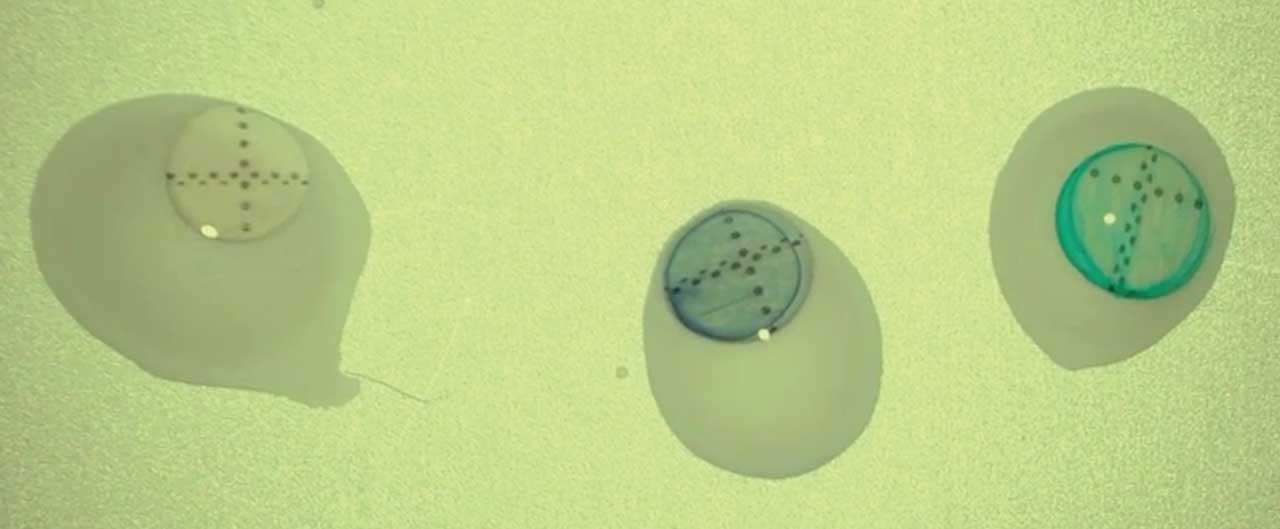
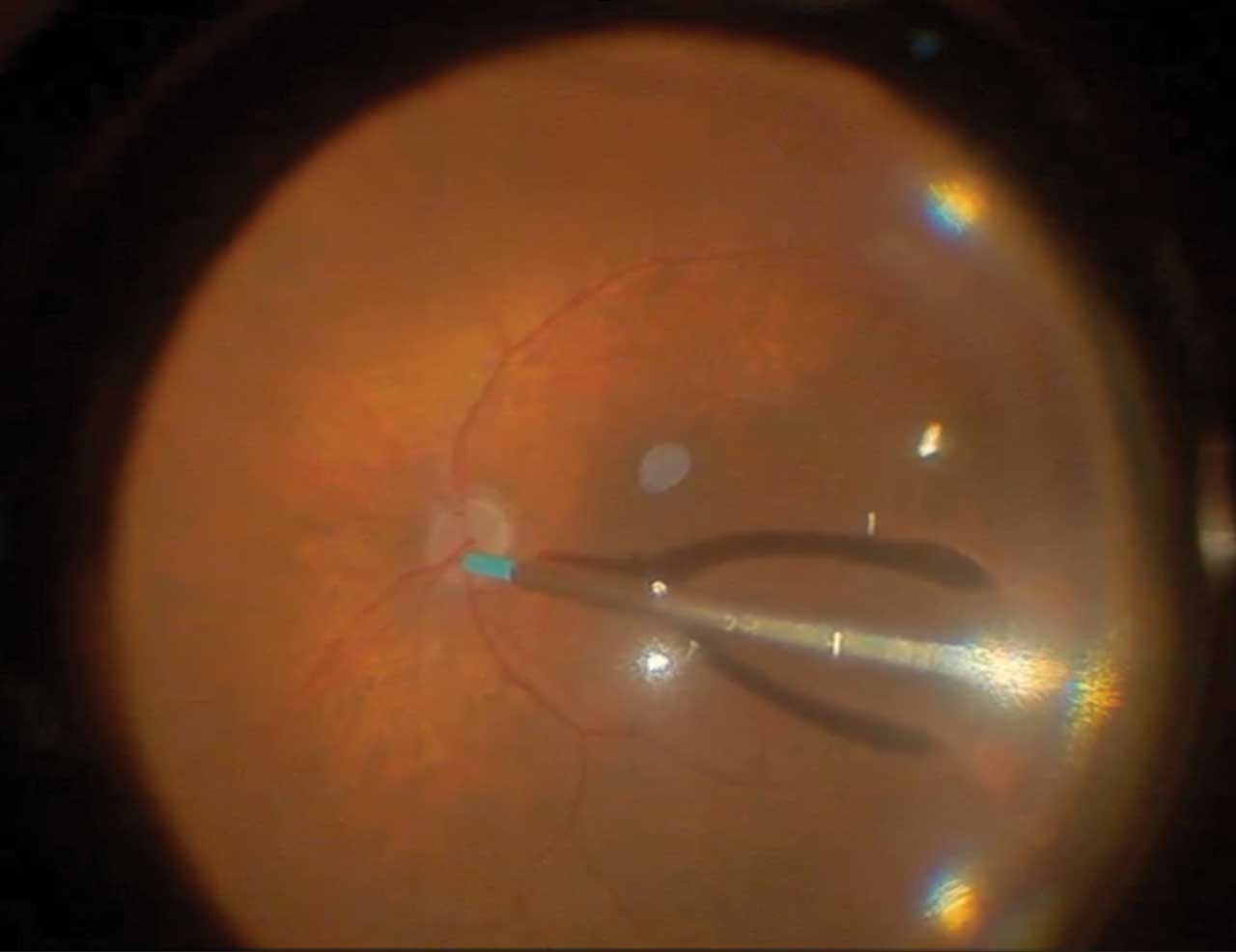
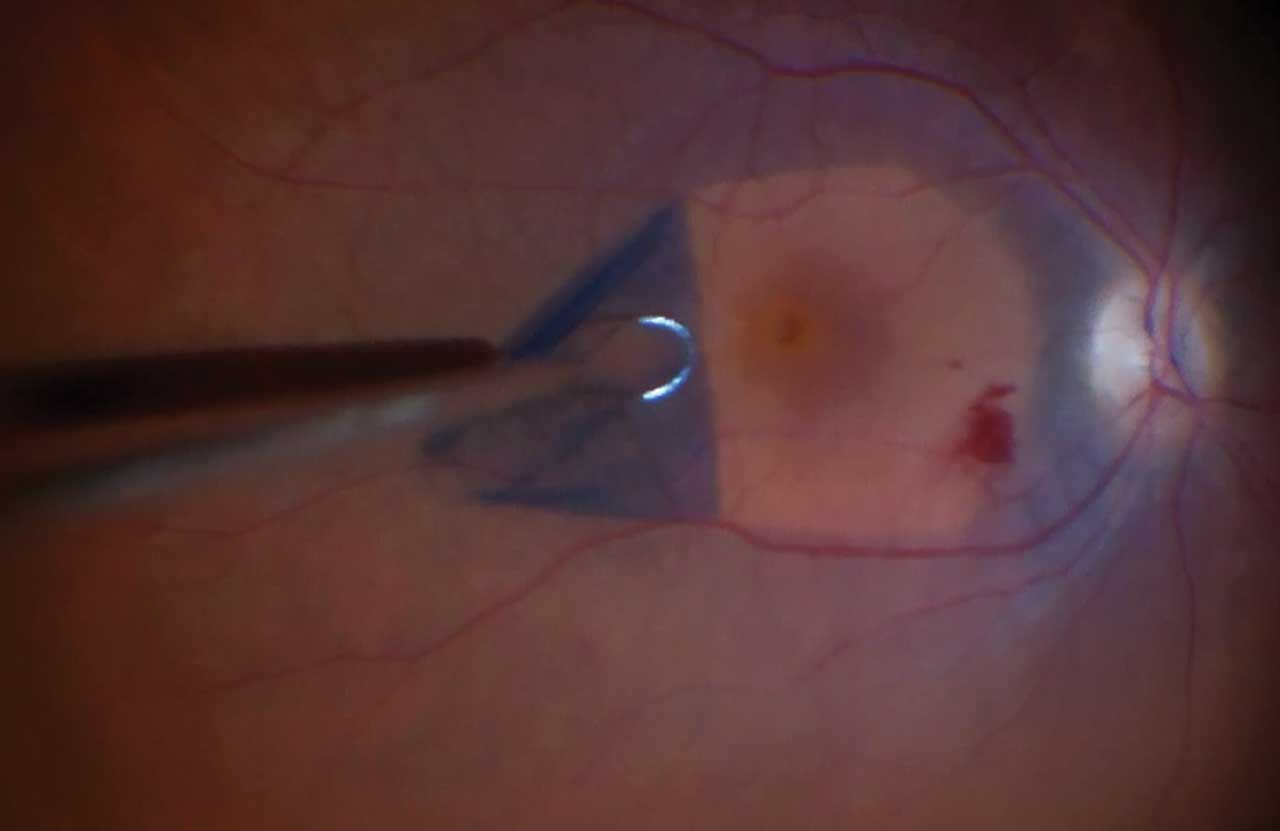
The ART approach should be avoided in eyes with extensive chorioretinal scarring precluding availability of a good ART harvest site, in eyes with history of proliferative vitreoretinopathy or significant ischemia, and in pediatric eyes. Using the ART approach in these cases could cause harvest site complications, and ART harvested from an ischemic retina likely carries poor prognosis. The AMG approach or subretinal blebs may be preferred for expansion in such cases. With AMG, consider staining the graft with brilliant blue or trypan blue (Figure 2). This allows easy visualization of the graft at all steps including the fluid-air exchange. It is also important to gently place the AMG under the hole edge to lower the risk of dislocation (Figure 3). A scaffold-based approach facilitates closure of the macular hole by creating an interface to promote glial migration and proliferation to bridge the macular defect.
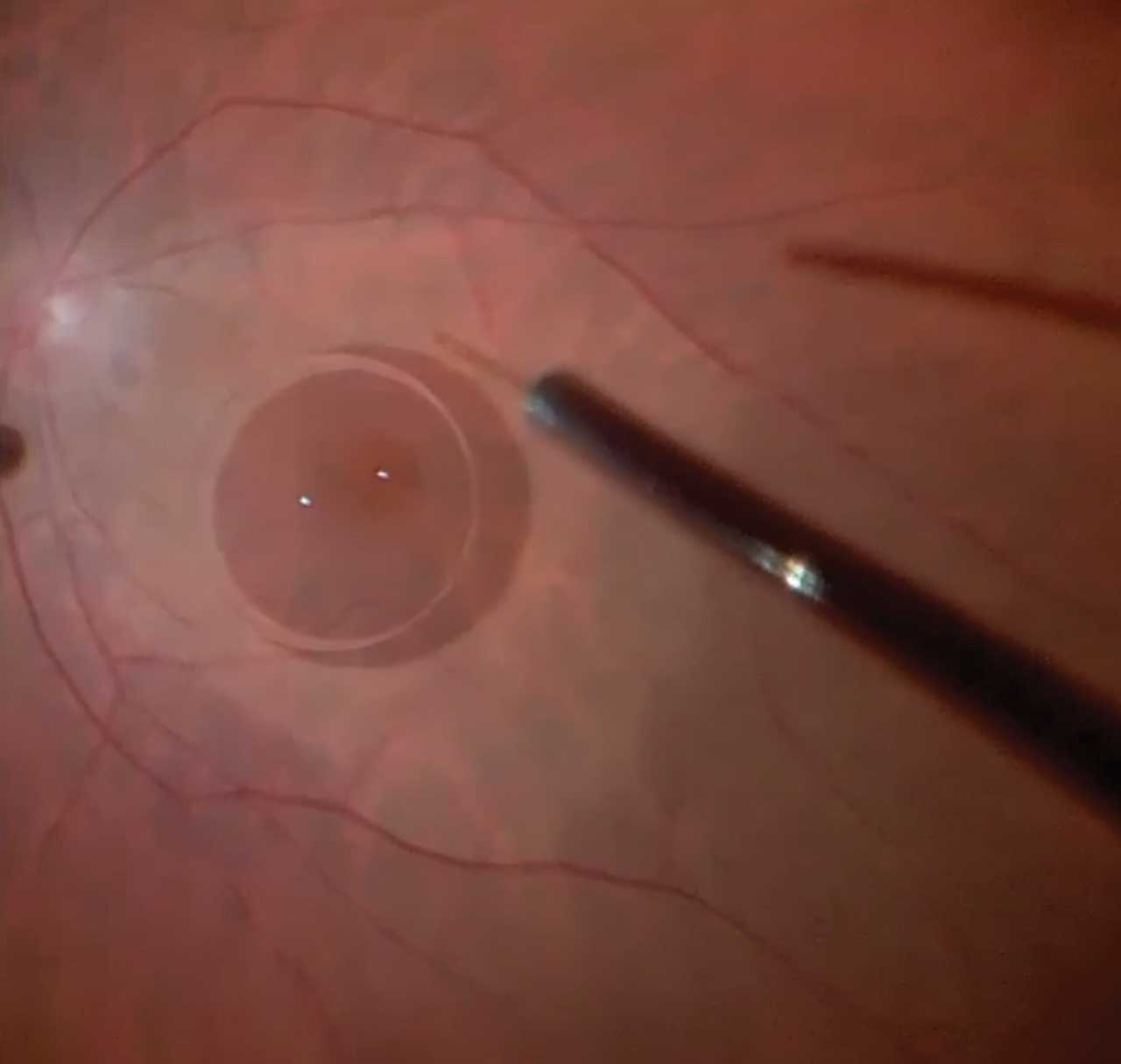
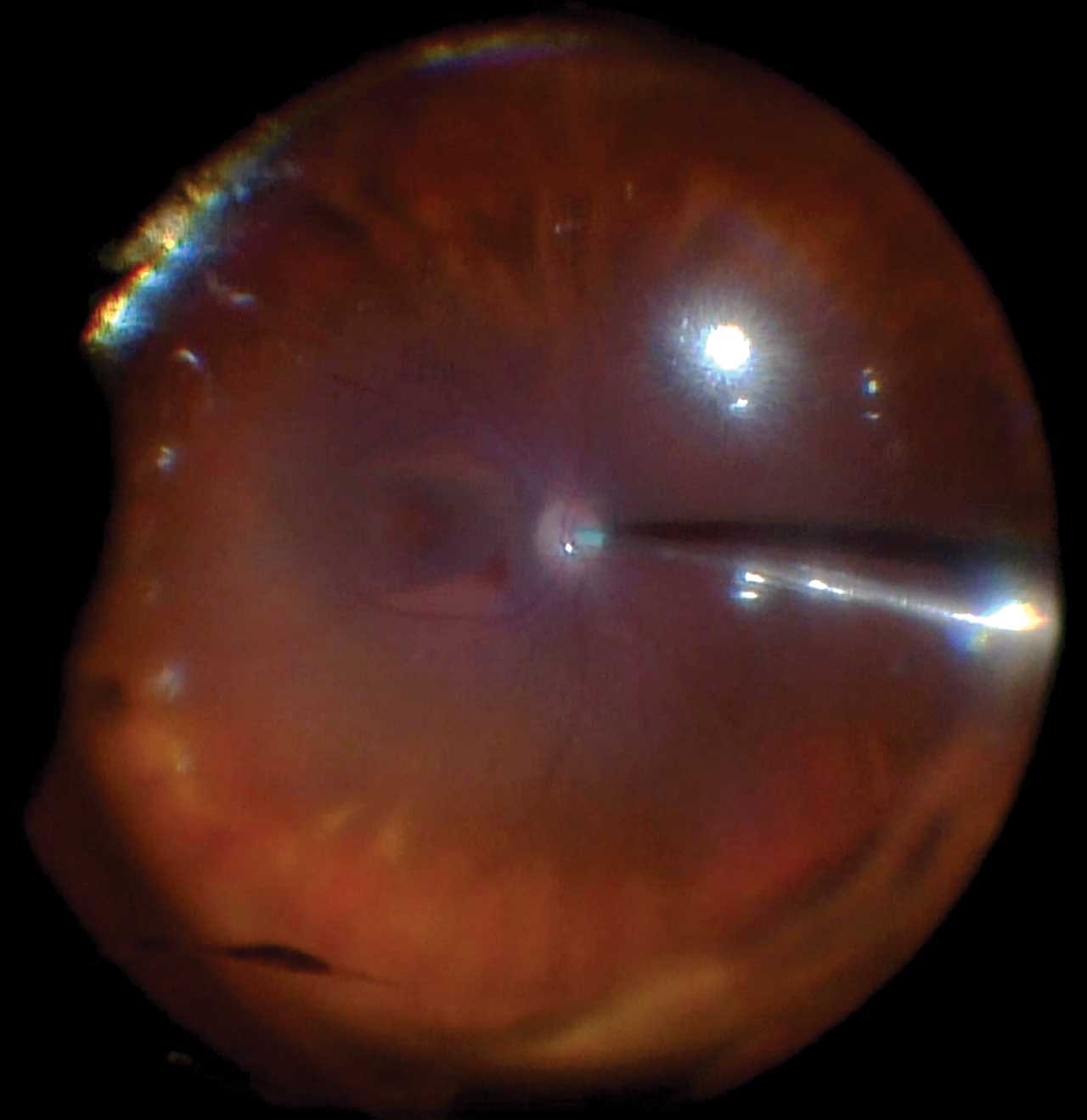
For subretinal bleb creation, it is helpful to use a 41-gauge cannula such as the MedOne subretinal PolyTop Cannula with an inner diameter of 41-gauge and outer diameter of 38 gauge (MedOne). This can be combined with microinjection systems such as the Inicio which is compatible with the Eva Nexus (DORC/Carl Zeiss Meditec) and allows foot pedal–based precise and controlled administration of the fluid into the subretinal space. Once the initial bleb is visualized, the injection pressure should be reduced to allow creation of a large uniform bleb. Placing a small bubble of perfluorocarbon over the macular hole reduces the risk of the bleb migrating into the hole and inadvertently enlarging the hole (Figure 4). Creating 3 to 4 blebs will surround the macular hole, and a nitinol Finesse Flex loop (Alcon) can then be used to mobilize the macula and gently approximate the edges of the hole.
In eyes undergoing their first surgery, the retracting door ILM flap technique described by Dr. Tamer Mahmoud can be effective, wherein the ILM is peeled (and not removed) nasally to temporally over the hole with a large temporal hinge (Figure 5) and then draped back over the macular hole at the end of the fluid-air exchange (Figure 6).7 This technique allows removal of the taut ILM and relieves the tractional forces while maintaining the natural orientation of ILM and Müller cell processes with respect to the macula. The retracting door technique also allows preserving the ILM for use as a graft in any future surgeries in case the hole does not close. The flap is also less susceptible to displacement by fluid currents.
Although it is now relatively rare to encounter adequate residual ILM identified in eyes with a large refractory macular hole that have undergone prior surgery, in cases where there is adequate residual ILM, the eye is not a pathologic myope, and the macular hole inner opening diameter is <1,000 μm, the inverted or the autologous ILM flap technique can be effective.
For large macular hole–associated retinal detachments, a scaffold-based technique is required, and the AMG or ART techniques can be effective coupled with draining the subretinal fluid using a separate retinotomy.
Finally, in eyes with significant macular ischemia, advanced glaucoma, or optic atrophy causing significant vision impairment that is unlikely to improve following closure of the large macular hole, it is important to recognize the limited visual prognosis. In these cases, observation is often the best approach.
Conclusion
Given the rare occurrence of refractory holes and the heterogeneity across presentations, it is not possible to accurately compare outcomes across techniques. It is helpful for vitreoretinal surgeons to have multiple techniques in their surgical toolbox that they can modify according to their personal preference and customize the technique to each patient. Future work may facilitate development of an algorithm to guide a tailored surgical approach to different types of macular holes to achieve better anatomic and functional outcomes, while reducing the number of procedures needed to reach such outcomes. RP
Hear discussion of this article at retinapodcast.com.
References
1. Kelly NE, Wendel RT. Vitreous surgery for idiopathic macular holes. Results of a pilot study. Arch Ophthalmol. 1991;109(5):654-659. doi:10.1001/archopht.1991.01080050068031
2. Rossi T, Bacherini D, Caporossi T, et al. Macular hole closure patterns: an updated classification. Graefes Arch Clin Exp Ophthalmol. 2020;258(12):2629-2638. doi:10.1007/s00417-020-04920-4
3. Grewal DS, Mahmoud TH. Autologous neurosensory retinal free flap for closure of refractory myopic macular holes. JAMA Ophthalmol. 2016;134(2):229-230. doi:10.1001/jamaophthalmol.2015.5237
4. Caporossi T, Governatori L, Gambini G, et al. Treatment of recurrent high myopic macular hole associated with retinal detachment using a human amniotic membrane. Jpn J Ophthalmol. 2022;66(6):518-526. doi:10.1007/s10384-022-00953-w
5. Meyer CH, Borny R, Horchi N. Subretinal fluid application to close a refractory full thickness macular hole. Int J Retina Vitreous. 2017;3:44. doi:10.1186/s40942-017-0094-7
6. Shields RA, Mahmoud TH. Management of autologus retinal transplant complications: a case series. Retina. 2023;43(11):2030-2033. doi:10.1097/IAE.0000000000003329
7. Finn AP, Mahmoud TH. Internal limiting membrane retracting door for myopic macular holes. Retina. 2019;39 Suppl 1:S92-S94. doi:10.1097/IAE.0000000000001787









