Key Takeaways
- Watch videos below for demonstrations.
- For retina specialists encountering cases of dislocated intraocular lens, considering the variety of repositioning and exchange techniques is essential to optimal outcomes.
- Innovative techniques, such as the Yamane technique and its variations, offer sutureless solutions for IOL fixation, reducing complications associated with sutures.
- Future advancements, including new IOL designs, promise to improve outcomes for patients with dislocated IOLs, addressing a need among the growing population of those undergoing caratact surgery.
Cataract surgery is the most common intraocular procedure worldwide, with approximately 10 million surgeries performed annually.1 The prevalence of cataract surgery is driven by its high success rate and the significant improvement in the quality of life it offers patients. However, the cumulative probability of intraocular lens (IOL) dislocation can reach 2% after 25 years, underscoring the importance of effective IOL implantation techniques.2 As life expectancy increases and patients undergo surgery at younger ages, the number of dislocated IOLs is expected to rise, presenting a growing challenge.
Despite the frequency of IOL repositioning and IOL exchange procedures performed, there is no IOL available in the United States designed specifically for implantation in eyes with no capsular support. In the European Union, the Carlevale IOL (MD Tech and Soleko) is available; this lens has 2 T-shaped ends that can be imbricated in the sclera when there is no capsular support. Surgeons in the United States must therefore use creative techniques with available IOLs to achieve visual acuity correction in these challenging cases.
We present various secondary IOL implantation techniques, particularly focusing on cases lacking capsular support. In general, when a 3-piece or a polymethylmethacrylate (PMMA) IOL is dislocated, repositioning it should be considered, because IOL exchanges are associated with increased endothelial cell loss compared to repositionings.3
IOL Implantation and Repositioning Techniques
Intraocular lens implantation techniques can be broadly categorized based on the presence or absence of the anterior capsule, each with specific methods and considerations.
Techniques With Anterior Capsular Support
The ideal method for cases where the anterior capsule is intact involves implanting or repositioning a 3-piece IOL or PMMA IOL in the sulcus, supported by the anterior capsule rim. Optic capture with the anterior capsule is preferred if there is enough capsular support. This approach is favored due to its stability and lower risk of complications. Repositioning a 1-piece acrylic IOL in the sulcus is not recommended due to the potential for iris chafing from the square edges of the IOL. This can lead to complications such as iris atrophy and uveitis-glaucoma-hyphema (UGH) syndrome (Figure 1).4

Techniques Without Anterior Capsular Support
Techniques for IOL fixation without capsular support can be divided into 2 categories: sutured and sutureless.
Sutured Techniques
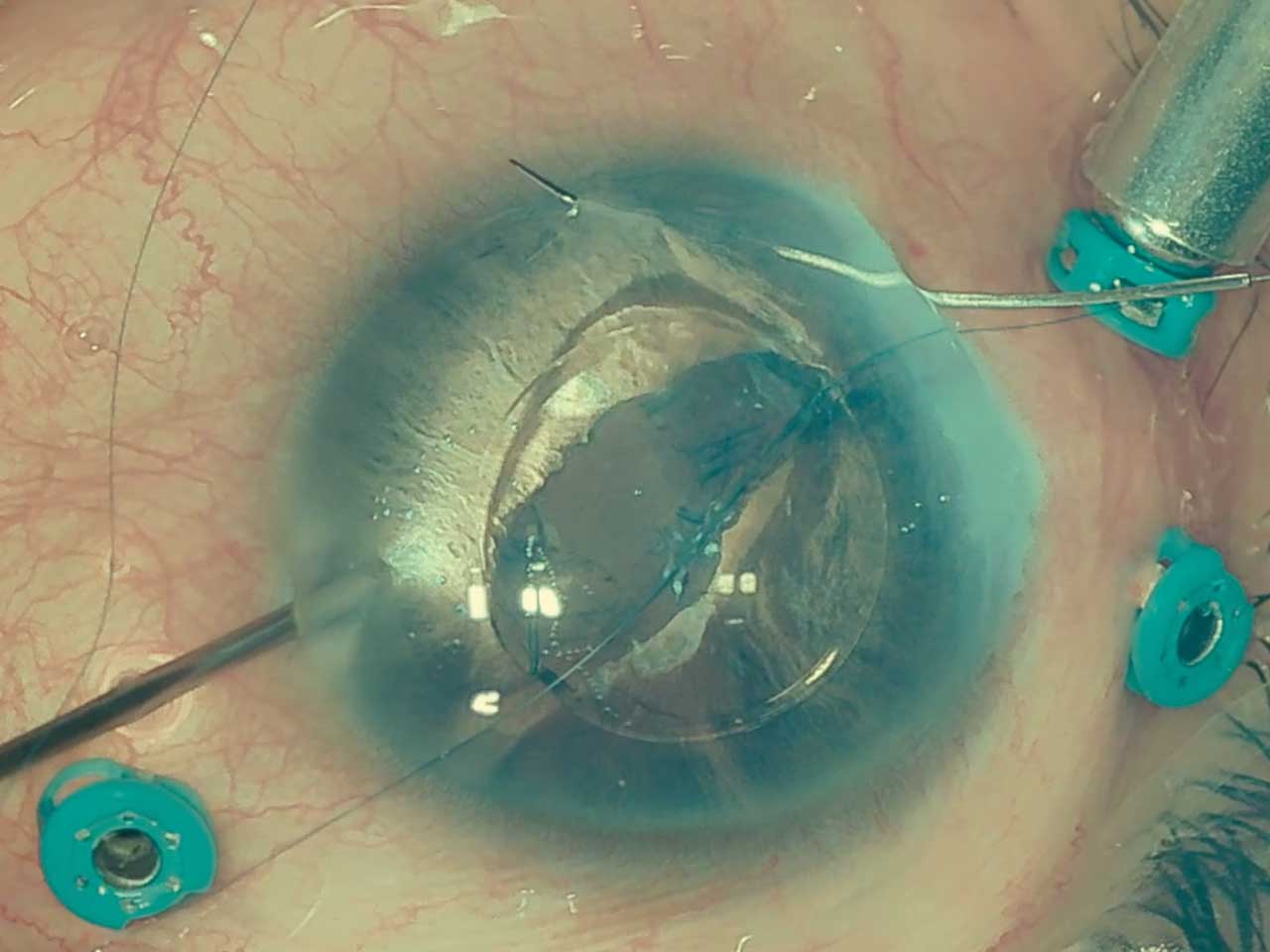
Iris suturing: This method uses polypropelene (Prolene; Johnson & Johnson) sutures to attach 3-piece or 1-piece PMMA IOLs directly to the iris. Described by McCannel in 1976, the technique involves placing the IOL in the sulcus and capturing the optic anterior to the iris for enhanced stability during suturing (Figure 2). A McCannel Prolene suture is passed through cornea-iris, haptic-iris-cornea, and the 2 ends tied on the iris to hold the haptics. The same procedure is repeated with the second haptic.5 Published series of this technique do not show an increased incidence of cystoid macular edema.6 Nevertheless, the Prolene sutures can erode through the iris, resulting in IOL dislocation over time.
Scleral suturing: Techniques such as 4-point fixation with Gore-Tex 7-0 CV-8 (Gore-Tex) sutures offer excellent stability. This technique was described with the Akreos AO60 (Bausch + Lomb) lens, which has 4 eyelets. These are sutured to the sclera 2 mm to 3 mm from the limbus through incisions 6 mm to 7 mm apart with a 4-point fixation with Gore-Tex.7 The Gore-Tex does not erode over time, so future dislocation is infrequent. Downsides of this technique are that the IOL is hydrophilic, and the optic can opacify over time, particularly if gas or silicone are left in the eye.8 As such, it is not ideal for cases that have vitreoretinal pathologies that may require a tamponade. Another Gore-Tex 4-point fixation technique uses a 1-piece foldable hydrophobic acrylic IOL (Envista MX60T; Bausch + Lomb).9 Because this IOL is hydrophobic, opacification is a reduced concern compared to the Akreos. Although 4-point fixation provides stability, potential complications are tilt, decentration, and breakage of the IOL when the Gore-Tex suture is tighter on one side than the other. Variations of this technique use 6–0 polypropylene monofilament suture (Ethicon Inc) to create a 3-point fixation using flanged cauterized prolene embedded in the sclera.10
Sutureless Techniques
Sutureless techniques encompass the Yamane technique and its many variations. This innovative approach involves embedding the haptics of a 3-piece IOL in the sclera without the use of sutures. The benefits include reduced complications related to suture erosion and a more streamlined surgical process. However, the technique requires precise execution to prevent common issues such as tilt and astigmatism.
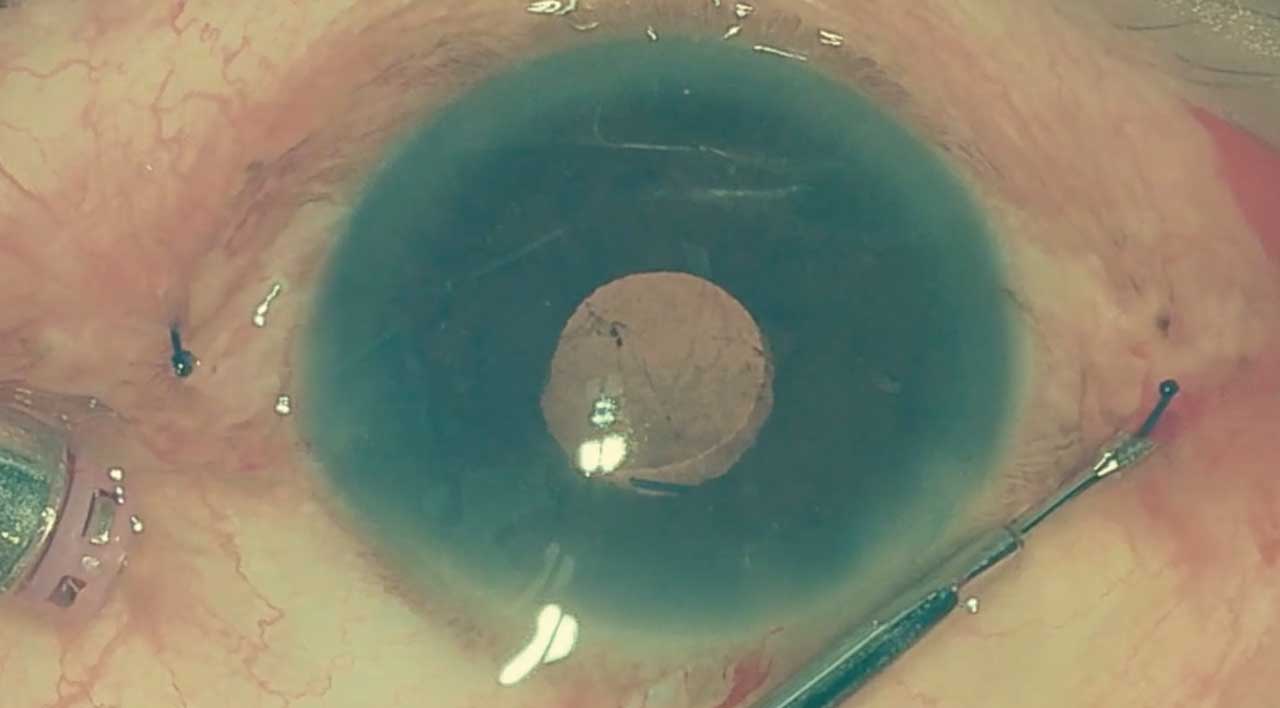
The original Yamane technique uses a 3-piece IOL with polyvinylidene (PVDF) haptics, similar to the CT Lucia 3-piece IOL (Carl Zeiss Meditec).11 These are sturdier than Prolene haptics in older IOLs. Two thin-walled 30-gauge needles (TSK Steriject; TSK Laboratory) are passed into the eye 2 mm from the limbus in a tunneled fashion in opposite directions 180 degrees apart. The haptics are threaded into the hub of the needles and brought out through the sclera and conjunctiva. Once outside, the tip is cauterized to create a small flange, and this is buried into the sclera on both sides (Figure 3). Care must be taken to measure the entry points adequately to prevent tilt (Video 1).
The most popular of several variations is the modified Yamane, which uses 27-gauge or 25-gauge trocars to remove the haptics through the trocars with intravitreal forceps instead of through the needles. In our practice, the preferred variation is the streamlined 27-gauge trocar technique that only uses 3 trocars (Figure 4; Videos 2 and 3). Other techniques include making scleral pockets to cover the ends of the flanged Prolene, because the cauterized tip can erode through the conjunctiva, and using tissue glue to fix the haptics to scleral flaps, as described by Agarwal.12

When the IOL-capsular bag complex is dislocated, several techniques can be used. If the IOL is a 1-piece acrylic IOL and the bag is adequately fibrosed, the bag can be sutured to the sclera with Prolene or Gore-Tex. This is done by passing a suture to thread the haptics and capsule and fixing it at 2 points on each side of the sclera. If the bag has a 3-piece IOL and the haptics do not show distortion, the bag can be removed from the IOL, and the IOL fixated by the Yamane technique or sutured to the iris. A very elegant new technique for repositioning a dislocated 1-piece IOL and capsule complex involves an IOL punch that creates a hole in the IOL near the haptic.13 A 5.0 Prolene suture with a cauterized end is passed through the hole, and the other end is passed through the sclera and fixed by cauterizing the end and burying it into the sclera, similar to how the Yamane haptics are cauterized and buried. This technique would allow for repositioning of 1-piece multifocal and toric (premium) IOLs. The punch is still not commercially available but is being developed by Diamatrix.
Anterior chamber (AC) IOLs are still used in some cases, and good visual acuity gains can be achieved, but long-term complications of AC IOLs include glaucoma, cystoid macular edema, corneal edema, inflammation, and progressive endothelial cell loss. These lenses are best reserved for the elderly, because corneal decompensation can occur over time.
Surgical Considerations and Patient Outcomes
Patient selection, technique, and postoperative care must all be considered for optimal outcomes. Patient-specific factors such as age, ocular anatomy, and the presence of other ocular conditions are important in the choice of IOL implantation technique. Tailoring the approach to individual needs is crucial for optimizing outcomes. Surgeons also often modify standard techniques to adapt to the unique challenges presented by each case. These variations can include adjustments in the placement of sutures or the selection of IOL type based on the patient’s specific anatomical and physiological characteristics. Postoperative care that is essential for ensuring the success of IOL implantation includes managing inflammation, monitoring for signs of dislocation, erosion, and other complications.
Future Directions
The development of new IOLs specifically designed for implantation in eyes without capsular support could significantly improve outcomes for a substantial patient demographic in the US. Ongoing research and innovation in this area are crucial for advancing the field of ophthalmology and improving surgical techniques. Repositioning techniques for toric and multifocal one-piece IOL, like the punch technique, would be useful as more and younger patients are implanted with multifocal IOLs.
Conclusion
As IOL repositioning techniques continue to evolve, addressing the challenges posed by demographic changes and clinical needs becomes increasingly important. Vitreoretinal surgeons need to familiarize themselves with the many techniques and choose the ones that work best for them and the dislocated IOLs they may encounter. Continued advancements are expected to drive improvements in safety, efficacy, and patient satisfaction. RP
Hear discussion of this article at retinapodcast.com.
References
1. Lee GI, Lim DH, Chi SA, et al. Incidence and characteristics of intraocular lens dislocation after phacoemulsification: an eight-year, nationwide, population-based study. J Clin Med. 2021;10(17):3830. doi:10.3390/jcm10173830
2. Pueringer SL, Hodge DO, Erie JC. Risk of late intraocular lens dislocation after cataract surgery, 1980-2009: a population-based study. Am J Ophthalmol. 2011;152(4):618-623. doi:10.1016/j.ajo.2011.03.009
3. Kang YK, Park DH, Ryu G, Kim HK, Kim DH, Do JR. Repositioned versus exchanged flanged intraocular lens fixation for intraocular lens dislocation [published correction appears in Sci Rep. 2024 Mar 27;14(1):7279]. Sci Rep. 2024;14(1):6181. doi:10.1038/s41598-024-54694-6
4. Mehta R, Aref AA. Intraocular lens implantation in the ciliary sulcus: challenges and risks. Clin Ophthalmol. 2019;13:2317-2323. doi:10.2147/OPTH.S205148
5. Stutzman RD, Stark WJ. Surgical technique for suture fixation of an acrylic intraocular lens in the absence of capsule support. J Cataract Refract Surg. 2003;29(9):1658-1662. doi:10.1016/s0886-3350(03)00054-3
6. Condon GP, Masket S, Kranemann C, Crandall AS, Ahmed II. Small-incision iris fixation of foldable intraocular lenses in the absence of capsule support. Ophthalmology. 2007;114(7):1311-1318. doi:10.1016/j.ophtha.2007.04.018
7. Khan MA, Gupta OP, Smith RG, et al. Scleral fixation of intraocular lenses using Gore-Tex suture: clinical outcomes and safety profile. Br J Ophthalmol. 2016;100(5):638-643. doi:10.1136/bjophthalmol-2015-306839
8. Belin PJ, Kim JH, Sheikh A, Winokur J, Rhee D, Deramo V. Incidence and risk of scleral-fixated Akreos (AO60) lens opacification: a case series. J Vitreoretin Dis. 2020;5(2):157-162. doi:10.1177/2474126420946605
9. Khan MA, Gupta OP, Pendi K, et al. Pars plana vitrectomy with anterior chamber versus Gore-Tex sutured posterior chamber intraocular lens placement: long-term outcomes. Retina. 2019;39(5):860-866. doi:10.1097/IAE.0000000000002042
10. Canabrava S, Canêdo Domingos Lima AC, Ribeiro G. Four-flanged intrascleral intraocular lens fixation technique: no flaps, no knots, no glue. Cornea. 2020;39(4):527-528. doi:10.1097/ICO.0000000000002185
11. Yamane S, Ito A. Flanged fixation: Yamane technique and its application. Curr Opin Ophthalmol. 2021;32(1):19-24. doi:10.1097/ICU.0000000000000720
12. Agarwal A, Kumar DA, Jacob S, Baid C, Agarwal A, Srinivasan S. Fibrin glue-assisted sutureless posterior chamber intraocular lens implantation in eyes with deficient posterior capsules. J Cataract Refract Surg. 2008;34(9):1433-1438. doi:10.1016/j.jcrs.2008.04.040
13. Micheletti JM, Weber N, McCauley MB, Doe EA, Coffee RE, Caplan MB. Punch and rescue technique for scleral fixation of dislocated single-piece intraocular lenses. J Cataract Refract Surg. 2022;48(2):247-250. doi:10.1097/j.jcrs.0000000000000845










