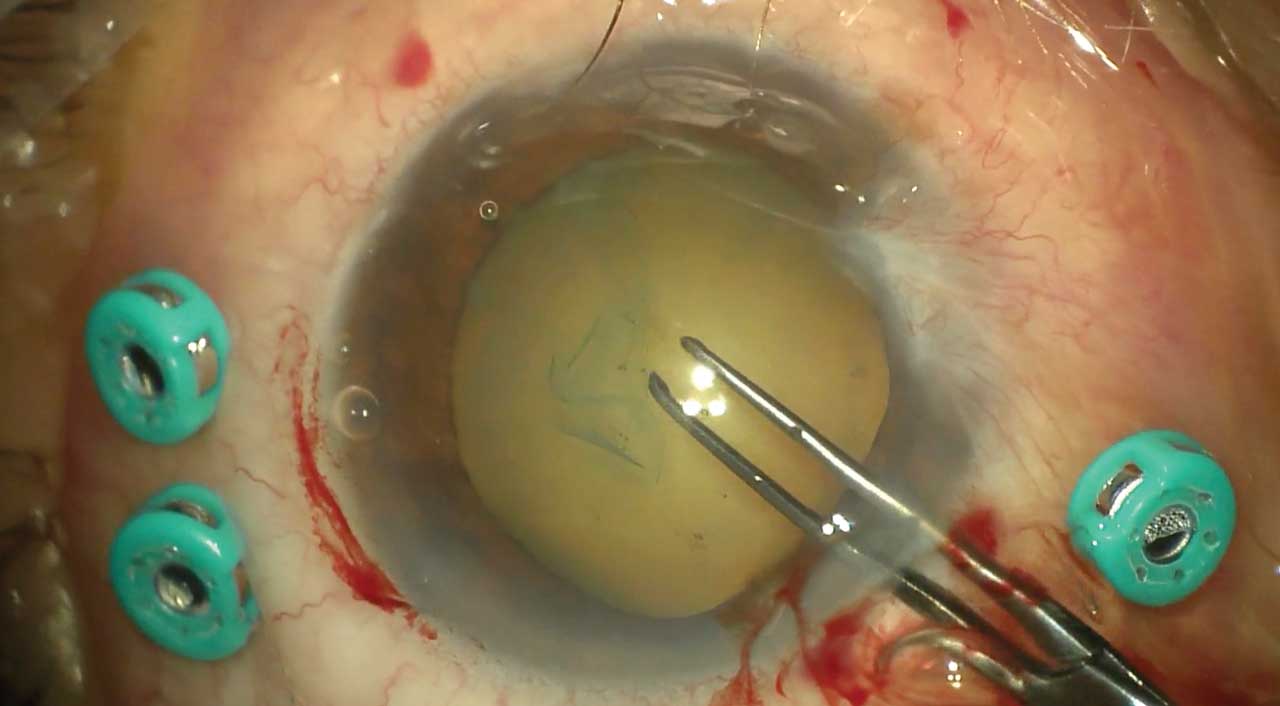
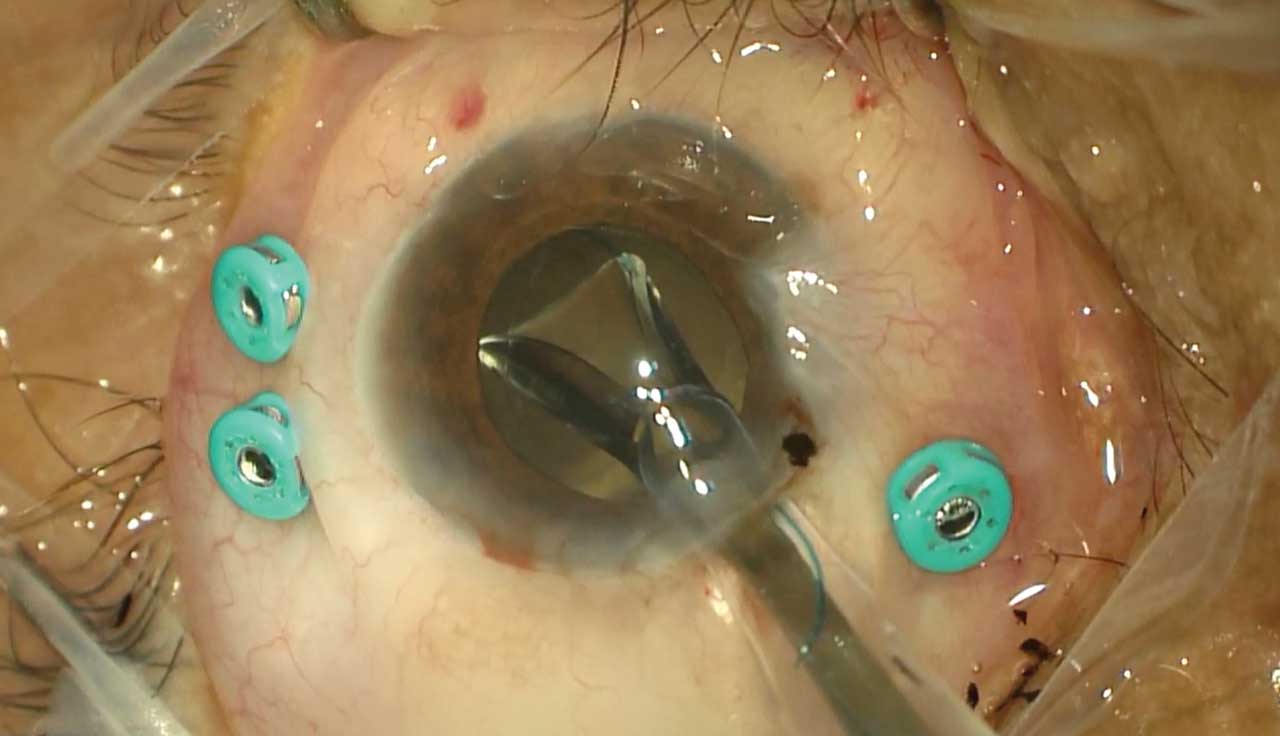
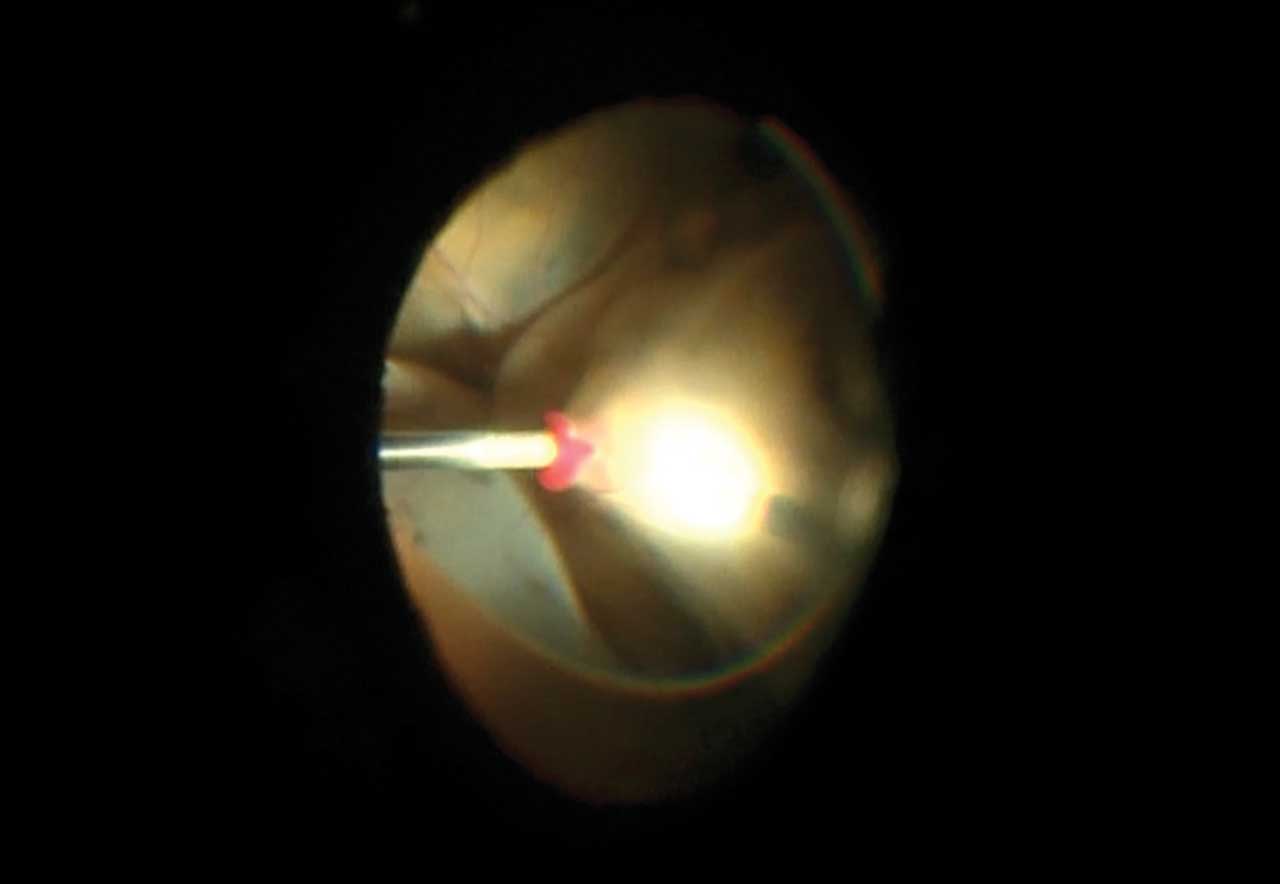
Since its inception in the early 1970s, microincisional vitrectomy surgery instrumentation has significantly improved outcomes in the treatment of complex vitreoretinal pathology.1 With advancements in surgical instrumentation and techniques, there is a growing recognition of the benefits conferred by the combination of phacoemulsification with microincision vitrectomy in patients with retinal pathology and concurrent visually significant cataracts. Extensive literature supports such benefits, including accelerated visual rehabilitation and reduced risks and costs associated with subsequent surgeries.2-4 Phacovitrectomy has been used in the surgical management of many complex retinal pathologies such as ocular trauma, intraocular tumors, retinal detachment, uveitis, pediatric cataracts, vitreous hemorrhage, vitreous opacities, preretinal membranes, and macular holes.5-10 This combined approach can be performed by either a vitreoretinal surgeon or an anterior-segment surgeon alongside a vitreoretinal surgeon, with involvement from multiple subspecialties depending on the etiology and patient demographic (Figures 1-3). This article aims to provide an updated report of techniques, outcomes, and the interspecialty collaborations involved in combined phacovitrectomy.
Outcomes of Combined Phacovitrectomy
The visual and anatomic outcomes of combined phacovitrectomy have been extensively studied. Muns et al reviewed 648 cases of combined phacovitrectomy in patients with intraocular tumors, epiretinal membranes, or tractional retinal detachments and found that visual acuity improved significantly from 20/192 at baseline to 20/46 at the 12-month follow-up.11 Delayed postoperative adverse events included vitreous hemorrhage in 21 eyes (3.2%) and progressive retinal detachment in 12 eyes (1.8%). Epiretinal membrane formation was observed in 11 eyes (1.7%), and posterior chamber intraocular lens displacement was present in 4 eyes (0.06%). There were no reports of endophthalmitis in any eye. In eyes with rhegmatogenous retinal detachment (RDD), the anatomic success rate of combined surgery was comparable to that of pars plana vitrectomy alone (84.3% vs 89.2%, P=.311), with no significant differences in mean visual acuity outcomes; additionally, combined surgery prevented the need for a second surgery for cataract extraction in 78% of cases.12
A randomized study by Mora et al comparing pars plana vitrectomy to combined phacovitrectomy for RRD found comparable outcomes in terms of best-corrected visual acuity, intraocular pressure, and central macular thickness between the 2 groups, although a higher recurrence rate of redetachment was observed in the combined surgery group without statistical significance.13 Moreover, a retrospective review of 427 eyes undergoing either sequential or simultaneous pars plana vitrectomy and cataract extraction demonstrated a significant difference in corrected distance visual acuity at postoperative month 1 and month 12, favoring sequential surgery; however, all groups achieved improved vision, particularly in cases of vitrectomy for epiretinal membrane or vitreous opacities.14 Additionally, a recent systematic review comparing sequential vs combined surgery for epiretinal membrane management found comparable proportions of eyes achieving Snellen visual acuity of at least 20/40 at 12 to 24 weeks in both procedures.15 It is possible that the ability to achieve similar outcomes either with sequential or simultaneous phacoemulsification and vitrectomy surgery is dependent on the surgeon’s expertise with combined surgery.
Refractive Outcomes and IOL Formula Considerations
There are varying results in the literature regarding refractory outcomes of phacovitrectomy, with most studies reporting mean absolute prediction errors of <1.0 D.8 For example, the use of intraoperative gas for retina tamponade has not been shown to cause a statistically significant difference in predicted vs actual postoperative refractive outcomes between the cataract alone surgery vs phacovitrectomy.16 Additionally, degree of myopia has not been shown to significantly affect refractive outcomes.17 However, myopic shifts are commonly observed after phacovitrectomy surgery.17-20 Myopic shifts have been attributed to effective lens position change after vitrectomy but more commonly associated with pre-existing retinal pathology such as RRD and epiretinal membranes owing to changes in axial lengths after vitrectomy.18,21-23
Several recent studies have been aimed at determining which IOL power formulas may offer increased refractive accuracy for phacovitrectomy. Choi et al reported that patients undergoing phacovitrectomy with gas tamponade showed no significant differences in mean error and mean absolute error among 4 main intraocular lens power formulas.24 Likewise, the authors report that there was no significant effect in outcomes when comparing high myopia and non–high myopia patients across the formulas. Interestingly, a study reviewed 301 eyes undergoing combined vitrectomy, silicone oil removal, and cataract surgery, and the authors found that the Barrett Universal II formula produced the most accurate refractive outcomes overall, with a median absolute error of 0.39 D.25 However, Ma et al demonstrated satisfactory refractive outcomes in highly myopic eyes with the combined use of SRK II and SRK/T proving comparable to the Barrett Universal II formula.17
Complications
The primary postoperative complication of combined phacovitrectomy is posterior capsular opacification, occurring in 5% to 17% of cases.14,26 Although posterior capsular opacification is common, routine posterior capsulotomy during phacovitrectomy may not be necessary for preventing its occurrence and can be safely performed after the initial 3-month postoperative period.27 Other reported complications include intraocular inflammation, corneal edema, glaucoma, hypotony, and cystoid macular edema.28,29
Regarding intraoperative complications, myosis is commonly faced during combined surgery.30 A more challenging complication is posterior capsular rupture which has been reported to occur in up to 10% of cases.26,30,31 Despite a higher incidence of posterior capsule rupture and iatrogenic retinal trauma in some phacovitrectomy series compared to cataract surgery alone, combined surgery does not seem to predict these complications.15 More recently, Hwang et al compared combined phacovitrectomy to cataract surgery alone in patients with diabetic retinopathy (DR) while employing an illuminated chopper-assisted cataract surgery method in both groups. They found no variance in the occurrence of posterior capsule rupture or operation time between the 2 procedures, suggesting that the use of this technique during phacovitrectomy could improve surgical outcomes.30 Similarly, a study by Ben et al did not find significant differences in postoperative complications between vitrectomy alone and phacovitrectomy in patients with proliferative DR.28
Additional Combined Procedures and Adjuvant Techniques
Temporary keratoprosthesis use in combination with vitrectomy has been reported since the 1990s.32-35 This innovative approach facilitates improved visualization of the posterior segment during vitrectomy, suggesting potential benefits in simultaneously addressing corneal opacification and vitreoretinal disorders. The combination of corneal transplant (penetrating keratoplasty or Descemet stripping automated endothelial keratoplasty), pars plana vitrectomy, and scleral IOL fixation has been described, and patients experienced enhanced visual outcomes, with significant improvements in best spectacle-corrected visual acuity of around 0.7 logMAR.32,35 In a recent case study, a 3-stage procedure was implemented, involving the temporary application of a soft contact lens as a keratoprosthesis, followed by vitrectomy and penetrating keratoplasty in a patient with significant ocular trauma; improved visual and anatomic outcomes were reported.36 Furthermore, reports show that integrating total pars plana vitrectomy during type 1 Boston Keratoprosthesis implantation can reduce postoperative complication rates. These complications include the development of glaucoma or vision loss due to glaucoma progression, retroprosthetic membrane formation, endophthalmitis, and the need for secondary procedures.37-38 Thus, vitreocorneal surgery proved effective in managing complex comorbidities of the eye.39
Additionally, Wang et al explored the combination of magnetic conduction technique and phacovitrectomy in the repair of intraocular foreign bodies (IOFBs).40 The authors describe the use of an external magnet to capture IOFBs with a magnetized vitrectomy cutter, facilitating their extraction through a corneal phacoemulsification incision. This approach achieved a final best-corrected visual acuity of 20/200 or better in 57.1% of patients, indicating the safety and feasibility of this combined approach for IOFB removal in the posterior segment.
Interspecialty Collaborations
Combined phacoemulsification and pars plana vitrectomy (PPV) can usually be conducted by a single surgeon in most cases. Although cases necessitating 2 separate surgeons for each stage of the procedure may benefit from the expertise of each surgeon, they also present logistical challenges such as scheduling and operating room coordination. Despite a lack of literature comparing outcomes between combined procedures performed by different surgeons vs those by a single surgeon, numerous studies indicate that a single surgeon undertakes both stages, suggesting its safety and efficacy. However, for patients with underlying conditions like uveitis or glaucoma, or in pediatric cases, effective communication between specialists is crucial to address their respective needs in the preoperative and postoperative period. A multidisciplinary approach facilitates personalized care plans, ensuring the best possible outcomes for each patient while addressing the complexities associated with combined phacoemulsification and vitrectomy surgeries across different patient populations and pathologies.
Conclusion
Literature consistently supports the effectiveness of combined phacovitrectomy surgery, emphasizing improved visual outcomes, reduced patient discomfort, and lower healthcare costs. Advancements in microincisional vitrectomy surgery underscore the importance of addressing both anterior-segment and posterior-segment issues for comprehensive treatment of complex vitreoretinal pathology. Patient selection remains critical for successful outcomes, considering factors like age, uveitis, and postoperative complication risk. Studies on refractive outcomes and lens calculations in combined surgeries show promising results, with various formulas demonstrating accuracy and minimal myopic shifts, highlighting the importance of precise preoperative calculations. Collaborative efforts among different specialties are essential for optimizing patient care and managing complex cases efficiently. RP
Hear discussion of this article at retinapodcast.com.
References
1. Ribeiro L, Oliveira J, Kuroiwa D, et al. Advances in vitreoretinal surgery. J Clin Med. 2022;11(21):6428. doi:10.3390/jcm11216428
2. Port AD, Nolan JG, Siegel NH, Chen X, Ness SD, Subramanian ML. Combined phaco-vitrectomy provides lower costs and greater area under the curve vision gains than sequential vitrectomy and phacoemulsification. Graefes Arch Clin Exp Ophthalmol. 2021;259(1):45-52. doi:10.1007/s00417-020-04877-4
3. Hertzberg SNW, Veiby NCBB, Bragadottir R, et al. Cost-effectiveness of the triple procedure - phacovitrectomy with posterior capsulotomy compared to phacovitrectomy and sequential procedures. Acta Ophthalmol. 2020;98(6):592-602. doi:10.1111/aos.14367
4. Xiao K, Dong YC, Xiao XG, et al. Effect of pars plana vitrectomy with or without cataract surgery in patients with diabetes: a systematic review and meta-analysis. Diabetes Ther. 2019;10(5):1859-1868. doi:10.1007/s13300-019-0672-9
5. Rating P, Bornfeld N, Schlüter S, et al. Long-term results after intraocular surgery in treated retinoblastoma eyes. Ocul Oncol Pathol. 2022;8(3):161-167. doi:10.1159/000524610
6. Conrady CD, Shakoor A, Patel R, et al. Combined phacoemulsification and pars plana vitrectomy for the treatment of cataract in patients with noninfectious uveitis. J Vitreoretin Dis. 2020;4(5):393-400. doi:10.1177/2474126420930489
7. Guber J, Bentivoglio M, Sturm V, Scholl HP, Valmaggia C. Combined pars plana vitrectomy with phacoemulsification for rhegmatogenous retinal detachment repair. Clin Ophthalmol. 2019;13:1587-1591. doi:10.2147/OPTH.S215352
8. Daud F, Daud K, Popovic MM, et al. Combined versus sequential pars plana vitrectomy and phacoemulsification for macular hole and epiretinal membrane: a systematic review and meta-analysis. Ophthalmol Retina. 2023;7(8):721-731. doi:10.1016/j.oret.2023.03.017
9. Günaydın NT, Oral AYA. Pediatric traumatic cataracts: 10-year experience of a tertiary referral center. BMC Ophthalmol. 2022;22(1):199. doi:10.1186/s12886-022-02427-6
10. Patel SB, Snyder ME, Riemann CD, Osher JM, Mi CW, Sisk RA. Combined phacoemulsification surgery with multifocal intraocular lens implantation and pars plana vitrectomy for symptomatic vitreous opacities. Retin Cases Brief Rep. 2021;15(6):724-729. doi:10.1097/ICB.0000000000000873
11. Muns SM, Villegas VM, Murray TG, Latiff A, Gold AS. Clinical outcomes of combined phacoemulsification with intraocular lens placement and microincision vitrectomy in adult vitreoretinal disease. J Vitreoretin Dis. 2022;7(1):27-32. doi:10.1177/24741264221118185
12. Tan A, Bertrand-Boiché M, Angioi-Duprez K, Berrod JP, Conart JB. Outcomes of combined phacoemulsification and pars plana vitrectomy for rhegmatogenous retinal detachment: a comparative study. Retina. 2021;41(1):68-74. doi:10.1097/IAE.0000000000002803
13. Mora P, Favilla S, Calzetti G, et al. Parsplana vitrectomy alone versus parsplana vitrectomy combined with phacoemulsification for the treatment of rhegmatogenous retinal detachment: a randomized study. BMC Ophthalmol. 2021;21(1):196. doi:10.1186/s12886-021-01954-y
14. Awidi AA, Mathews PM, Shekhawat N, Woreta FA, Srikumaran D, Daoud YJ. Comparison of simultaneous vs sequential pars plana vitrectomy and cataract surgery. BMC Ophthalmol. 2023;23(1):74. doi:10.1186/s12886-023-02801-y
15. Fouad YA, Soliman MK, Elhusseiny AM, Yang YC, Sallam AB. Visual outcomes and complications of combined versus sequential pars plana vitrectomy and phacoemulsification for epiretinal membrane. Eye (Lond). doi:10.1038/s41433-024-03004-5
16. Kokame GT, Tanji TT, Yanagihara RT, Shantha JG, Nirwan RS, Tanji TM. Refractive outcomes of combined cataract surgery and vitrectomy compared to cataract surgery alone. Ophthalmologica. 2023;246(1):39-47. doi:10.1159/000526039
17. Ma IH, Wang SW, Huang WL, et al. Comparison of refractive outcomes in patients with highly myopic versus non-highly myopic eyes undergoing phacovitrectomy. Ophthalmol Ther. 2023;12(2):1025-1032. doi:10.1007/s40123-023-00655-7
18. Kim YK, Woo SJ, Hyon JY, Ahn J, Park KH. Refractive outcomes of combined phacovitrectomy and delayed cataract surgery in retinal detachment. Can J Ophthalmol. 2015;50(5):360-366. doi:10.1016/j.jcjo.2015.07.003
19. Choi YJ, Jee D. Postoperative refractive outcomes of biometric formulas in phacovitrectomy with gas tamponade. Korean J Ophthalmol. 2023;37(4):322-327. doi:10.3341/kjo.2023.0012
20. Liu BS, Cui WN, Niu R, et al. Refractive outcomes after vitrectomy combined with phacoemulsification of idiopathic macular holes. Int J Ophthalmol. 2021;14(2):250-254. doi:10.18240/ijo.2021.02.11
21. Crincoli E, Savastano A, Ferrara S, et al. Refractive outcome in combined phacovitrectomy: anterior segment changes and corrective factor for IOL power calculation improvement. Eur J Ophthalmol. 2024;34(2):549-557. doi:10.1177/11206721231184502
22. Bellucci C, Romano A, Ramanzini F, Tedesco SA, Gandolfi S, Mora P. Pars plana vitrectomy alone or combined with phacoemulsification to treat rhegmatogenous retinal detachment: a systematic review of the recent literature. J Clin Med. 2023;12(15):5021. doi:10.3390/jcm12155021
23. Chen X, Zhao H, Ren JY, et al. Axial length, vitreoretinal pathology, and anterior chamber depth can predict postoperative refractive outcomes in phacovitrectomy/silicone oil removal. Int J Ophthalmol. 2023;16(4):554-562. doi:10.18240/ijo.2023.04.09
24. Fan H, Zhang M, Tzekov R, et al. Postoperative outcome of combined phacovitrectomy in eyes with excessive myopia (>-30 D). Case Rep Ophthalmol Med. 2023;2023:7367922. doi:10.1155/2023/7367922
25. Chen X, Zhao H, Xu Y, et al. Accuracy of new intraocular lens calculation formulae in eyes undergoing silicone oil removal/pars plana vitrectomy-cataract surgery. Retina. 2023;43(9):1579-1589. doi:10.1097/IAE.0000000000003846
26. Moraru AD, Costin D, Moraru RL, Branisteanu DC. Outcomes of simultaneous vs. sequential pars plana vitrectomy and cataract surgery. Exp Ther Med. 2020;20(6):183. doi:10.3892/etm.2020.9313
27. Jin KW, Woo SJ, Park KH. Efficacy and safety of primary posterior capsulotomy during phaco-vitrectomy for epiretinal membrane. BMC Ophthalmol. 2022;22(1):4. doi:10.1186/s12886-021-02226-5
28. Ben Addou Idrissi S, Bengebara O, Filali Sadouk M, et al. Comparison of pars plana vitrectomy and combined pars plana vitrectomy with phacoemulsification for proliferative diabetic retinopathy: a retrospective study about 120 eyes. Indian J Ophthalmol. 2024;72(Suppl 2):S287-S292. doi:10.4103/IJO.IJO_1976_23
29. Elhusseiny AM, Soliman MK, Shakarchi AF, Fouad YA, Yang YC, Sallam AB. Visual outcomes and complications of combined vs sequential cataract surgery and pars plana vitrectomy: multicenter database study. J Cataract Refract Surg. 2023;49(2):142-147. doi:10.1097/j.jcrs.0000000000001059
30. Hwang SH, Kim H, Lee DY, Nam DH. Intraoperative challenges and complications of cataract surgery between cataract surgery alone and phacovitrectomy in eyes with diabetic retinopathy: efficacy of illuminated chopper-assisted cataract surgery. BMC Ophthalmol. 2023;23(1):236. doi:10.1186/s12886-023-02982-6
31. Sizmaz S, Esen E, Isik P, Cam B, Demircan N. Outcome and complications of combined phacoemulsification and 23-gauge pars plana vitrectomy. J Ophthalmol. 2019;2019:7918237. doi:10.1155/2019/7918237
32. Yokogawa H, Kobayashi A, Okuda T, Mori N, Masaki T, Sugiyama K. Combined keratoplasty, pars plana vitrectomy, and flanged intrascleral intraocular lens fixation to restore vision in complex eyes with coexisting anterior and posterior segment problems. Cornea. 2018;37 Suppl 1:S78-S85. doi:10.1097/ICO.0000000000001716
33. Yu J, Shalaby WS, Shiuey EJ, et al. Graft Outcomes after temporary keratoprosthesis in combined penetrating keratoplasty and vitreoretinal surgery. Cornea. 2023;42(5):584-589. doi:10.1097/ICO.0000000000003207
34. Cooney T, Kinast R, Juratli L, Pedreira PN. Combined penetrating keratoplasty and vitreoretinal surgery with temporary keratoprosthesis. Cornea Open. 2023;2(2):e0012. doi:10.1097/coa.0000000000000012.
35. Hayashi T, Yasutsugu I, Shimizu T, et al. Pars plana vitrectomy combined with penetrating keratoplasty and transscleral-sutured intraocular lens implantation in complex eyes: a case series. BMC Ophthalmol. 2020;20(1):369. doi:10.1186/s12886-020-01639-y
36. Cisiecki S, Bonińska K, Bednarski M. Temporary keratoprosthesis combined with vitrectomy for severe globe injury. Retin Cases Brief Rep. 2023;17(6):785-787. doi:10.1097/ICB.0000000000001299
37. Lim JI, Machen L, Arteaga A, et al. Comparison of visual and anatomical outcomes of eyes undergoing type i boston keratoprosthesis with combination pars plana vitrectomy with eyes without combination vitrectomy. Retina. 2018;38 Suppl 1(Suppl 1):S125-S133. doi:10.1097/IAE.0000000000002036
38. Perez VL, Leung EH, Berrocal AM, et al. Impact of total pars plana vitrectomy on postoperative complications in aphakic, snap-on, type 1 Boston keratoprosthesis. Ophthalmology. 2017;124(10):1504-1509. doi:10.1016/j.ophtha.2017.04.016
39. Hayashi S, Osawa T, Tohyama K. Comparative observations on corneas, with special reference to Bowman’s layer and Descemet’s membrane in mammals and amphibians. J Morphol. 2002;254(3):247-258. doi:10.1002/jmor.10030
40. Wang Y, Chen B, Liu S, Gong Y, Zhang L. Combined phacovitrectomy with metallic intraocular foreign body removal through corneal incision using a novel “magnetic conduction” technique. Retina. 2023;43(12):2157-2161. doi:10.1097/IAE.0000000000003647











