Uveitis refers to a large group of inflammatory ocular diseases that can cause significant visual morbidity.1 Determining the degree of ocular inflammation is critical, not only for diagnosis, but also for monitoring response to therapy. Inflammation can also lead to cystoid macular edema (CME) or retinal vasculitis; the former can be observed by optical coherence tomography (OCT) while the latter requires identification by angiography.
Fluorescein angiography (FA) is an invasive procedure that commonly requires a skilled photographer, especially for patients with uveitis, which can make photography challenging due to miosis, cataracts and/or inflammatory haze. Therefore, there could be significant benefits to finding an alternative for FA when screening for retinal vasculitis.
In some uveitis patients, macular retinal thickening on OCT suggests the presence of retinal vascular leakage on FA. Both the Spectralis (Heidelberg Engineering) and Cirrus (Zeiss) machines can produce retinal thickness maps from OCT macular volume scans. Previous studies2-5 have shown that OCT macular thickness can act as a surrogate of active uveitic retinal vasculitis. Furthermore, OCTA generated retinal thickness maps also demonstrate correlation between capillary leakage and macular thickening.6 This article will illustrate the association of retinal vasculitis on FA with OCT macular thickness by providing 3 examples and discussing general guidelines that may be used by retinal physicians.
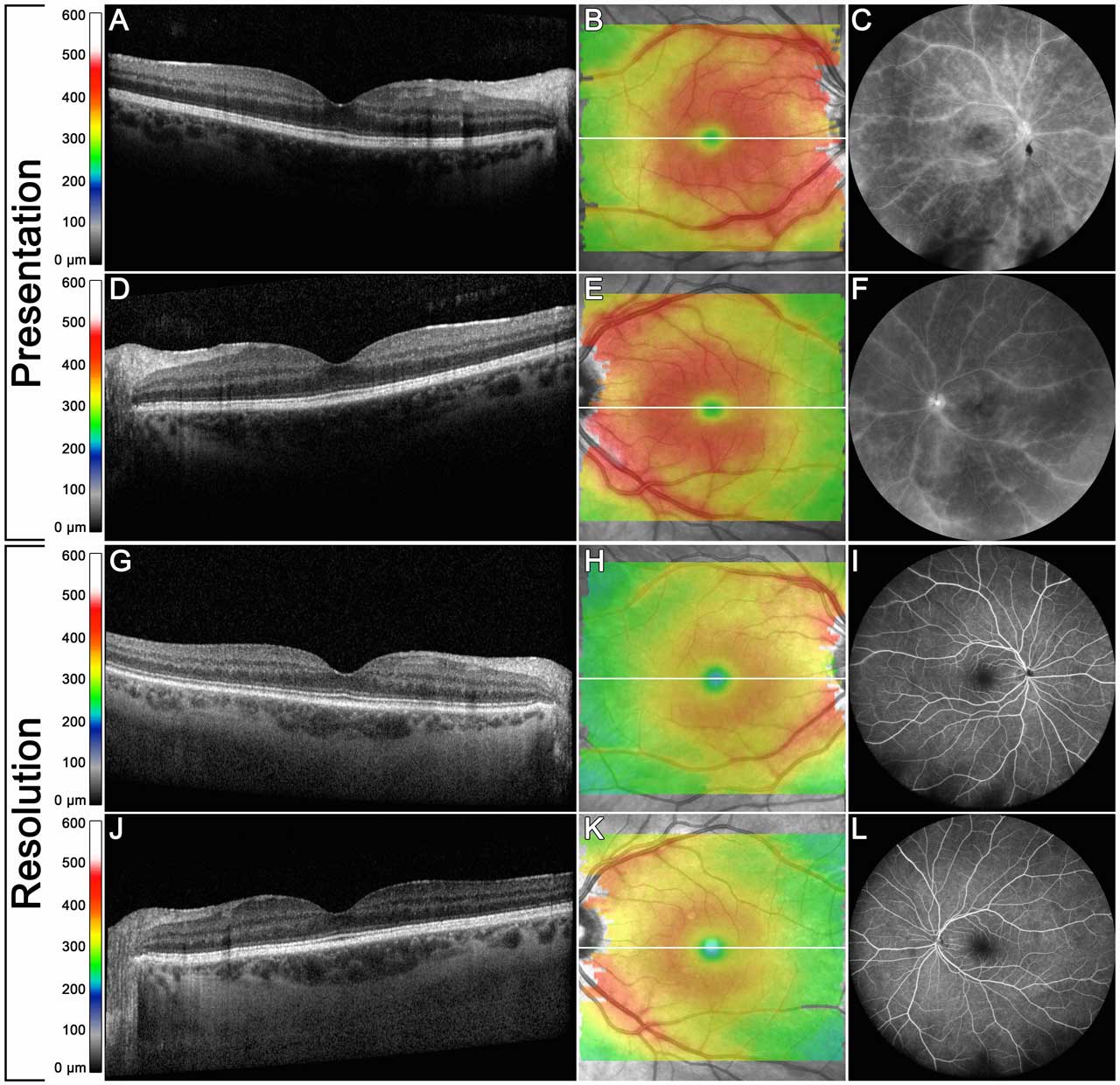
Case 1
A 41-year-old female presented with central photopsias and floaters in both eyes persisting for 2 years. She had been previously treated with topical and oral corticosteroids. Clinical examination demonstrated a quiet anterior chamber and 1-2+ anterior vitreous cell in both eyes. The fundus examination revealed mild arteriolar attenuation, mild periphlebitis, and inferior snowballs in both eyes. There were no retinal or choroidal lesions. The serologic workup was unrevealing. Optical coherence tomography showed no evidence of CME (Figure 1A, 1D); however, retinal thickness maps generated from the OCT macular volume scan demonstrated diffuse thickening with perivenular edema (Figure 1B, 1E). Fluorescein angiography showed extensive phlebitis from the posterior pole to the periphery in both eyes (Figure 1C, 1F).
The patient was initially treated with mycophenolate, as well as adalimumab with minimal clinical/imaging improvement. She was subsequently switched to subcutaneous tocilizumab 162 mg every week, which led to resolution of the intermediate uveitis and retinal vasculitis. The retinal thickness maps showed significant reduction (Figure 1H, 1K) in concert with resolution of the vasculitis on FA (Figure 1I, 1L).
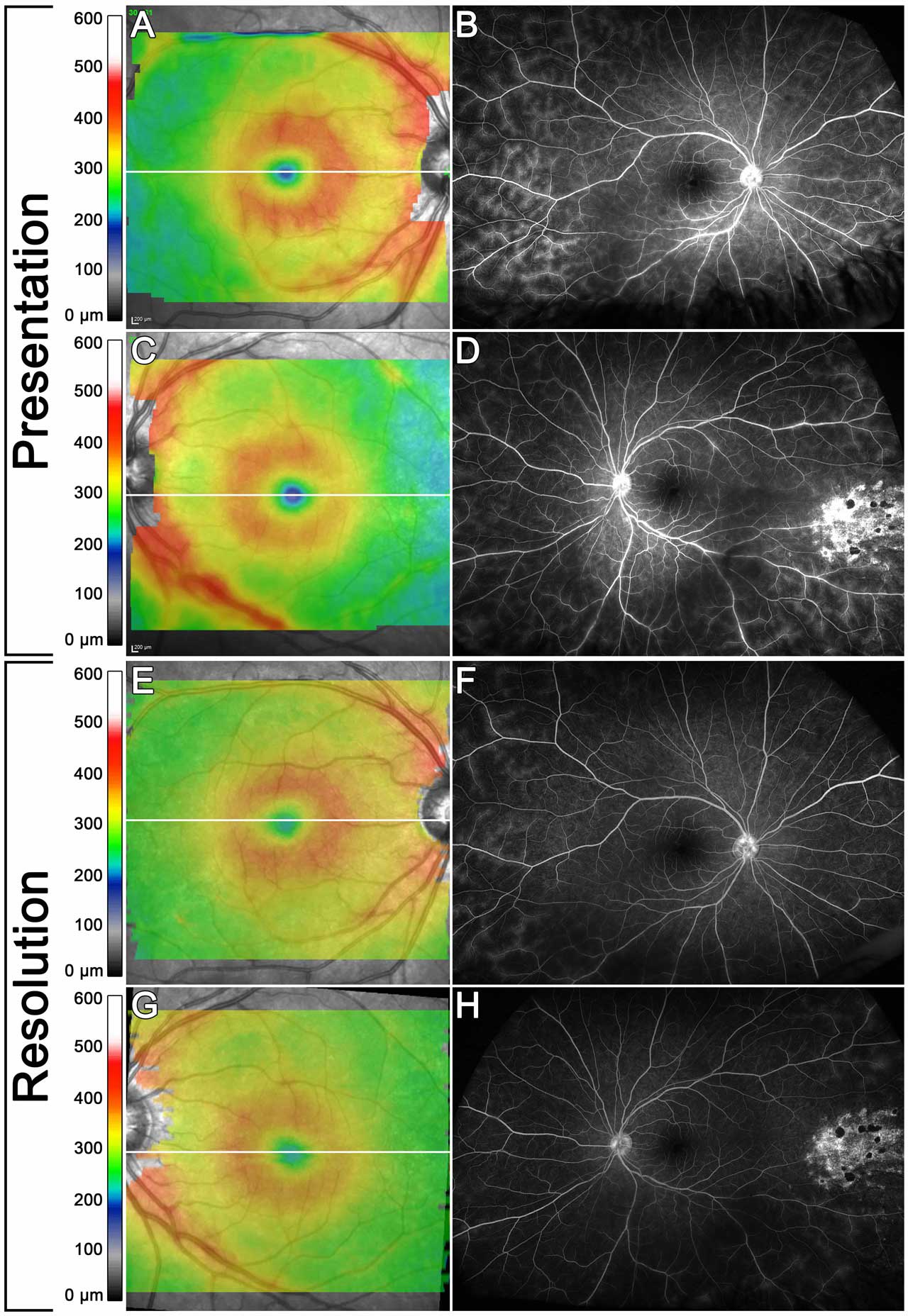
Case 2
A 17-year-old male presented with progressive floaters in both eyes for 1 year. Examination revealed 3-4+ vitreous cells and large snowballs in both eyes. The fundus exam demonstrated clinical vasculitis and inferior shallow retinoschisis in both eyes. Retinal thickness maps showed perivascular and perifoveal thickening (Figure 2A, 2C). Fluorescein angiography showed large-vessel vasculitis, mainly in the midperiphery. Serologic evaluation was negative, except for minimally elevated angiotensin converting enzyme (113 unit/L, normal range 13-100 unit/L). Chest X-ray revealed no abnormalities. He was initially treated with oral prednisone and oral methotrexate. The oral prednisone was tapered and the dose of methotrexate was titrated up to 25 mg weekly with minimal change in vasculitis. He was then switched to adalimumab 40 mg every 2 weeks, which led to significant improvement in retinal vasculitis. The retinal thickness map showed significant reduction (Figure 2E, 2G) in perivenular thickening, corresponding to significant improvement on FA (Figure 2F, 2H).
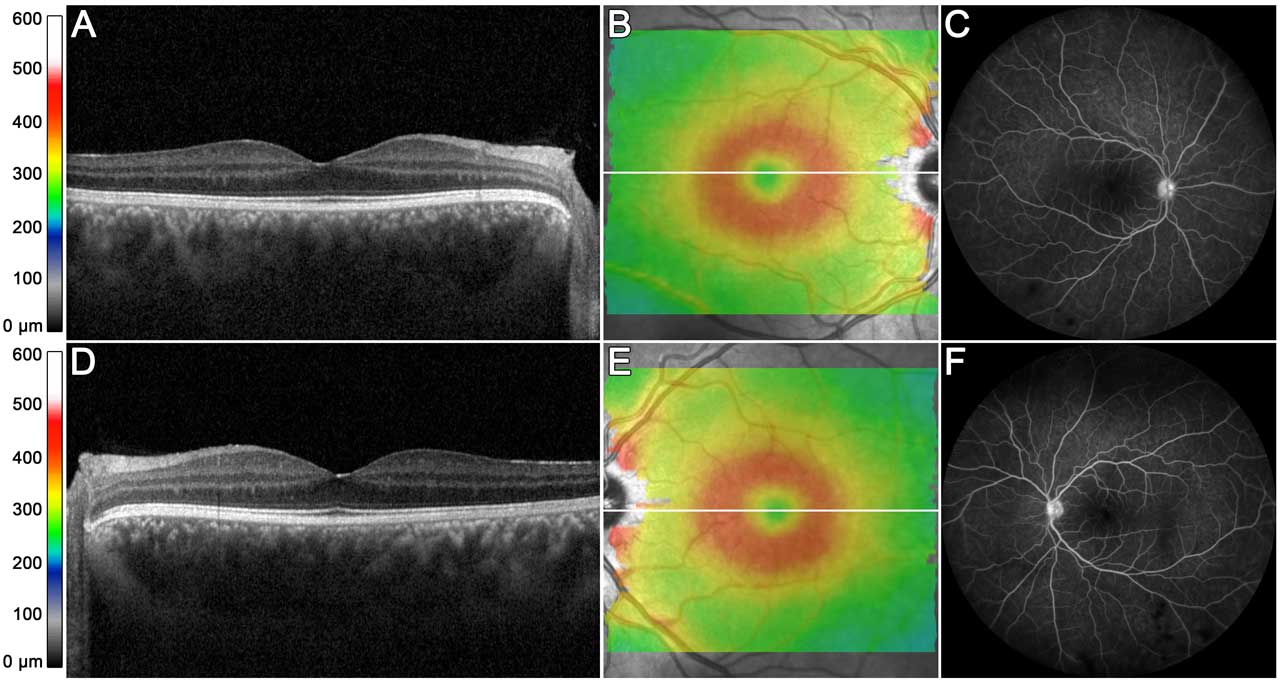
Case 3
A 21-year-old male presented with intermittent blurring of vision in both eyes. Clinical examination demonstrated 1-2+ cells in the anterior chamber in both eyes, 3-4+ anterior vitreous cell in the right eye and 2+ anterior vitreous cell in the left eye. The dilated examination was notable for multiple inferior snowballs in each eye. There was no evidence of clinical vasculitis. OCT macula demonstrated no CME (Figure 3A, 3D), and minimal perifoveal retinal thickening (Figure 3B, 3E). Fluorescein angiography (Figure 3C, 3F) demonstrated a few patches of far peripheral vasculitis but no posterior pole or midperipheral retinal vasculitis.
Discussion
In our clinical workflow, retinal thickness maps help provide a cursory view of retinal vascular leakage. We commonly use it in patients with intermediate uveitis to assess response to therapy or monitor inflammation between visits. Because obtaining an FA every visit can be burdensome for the patient — especially for our pediatric population — retinal thickness maps can serve as a proxy assessment of vasculitis between FAs. The amount of retinal thickness is displayed as a “heat map” (warmer colors for increasing thickness), which allows the physician to glean information quickly, and patients may find it easier to understand as compared to FA.
Reproducible high-quality FA can be challenging in uveitis given the inflammatory sequelae that limit clear image acquisition. However, OCT volume scans can be technically easy to acquire, especially in pediatric populations. In circumstances where the FA is of poor image quality, we use macular OCT thickness maps in tandem with the clinical exam to stratify risk of posterior pole leakage. If the volume scan shows “normal” thickness, we may favor close observation as opposed to modulation of therapy.
Retinal vasculitis can lead to vascular leakage and exudation, as well as global “sponge-like” changes in the macula, resulting in overall increased retinal thickness with or without classic CME.7 Although isolated far peripheral (outside the vortex vein) vasculitis may not cause long-term sequelae and may be observed, posterior pole vasculitis can cause CME, vascular occlusions, or macular ischemia,8 and is generally treated.
Although macular OCT thickness maps are helpful, this tool is neither an equivalent nor an alternative to FA. We recommend gold standard FA in all cases of uveitis that necessitate evaluation for retinal vasculitis. Furthermore, in diseases with occlusive vasculitis (eg, Behcet disease9), FA is paramount for monitoring disease activity and assessing response to treatment. Lastly, artifacts can be observed with retinal thickness maps, so caution is required during interpretation; for example, epiretinal membranes can cause an artifactual increase in thickness whereas highly myopic eyes that have significant vasculitis would be in the “normal” range, given the baseline myopic thinning.
Conclusion
Optical coherence tomography macular volume scans can generate macular thickness maps that provide a preliminary analysis of retinal vasculitis for patients with uveitis. In tandem with FA, retinal physicians can employ multimodal imaging to assess uveitic vascular leakage. RP
References
Suttorp-Schulten MS, Rothova A. The possible impact of uveitis in blindness: a literature survey. Br J Ophthalmol. 1996;80(9):844-848. doi: 10.1136/bjo.80.9.844.
Chen X, Zhu W, Li X. OCT macular volume as a predictor of vascular leakage in uveitis. Ophthalmol Ther. 2022;11(5):1913-1924. doi: 10.1007/s40123-022-00558-z.
Zarei M, Pesarakli H, Yaseri M, Etesali H, Ebrahimiadib N. Peripapillary optical coherence tomography as an alternative to fluorescein angiography for monitoring Behcet’s retinal vasculitis. Sci Rep. 2021;11(1):20037. doi: 10.1038/s41598-021-99485-5.
Ebrahimiadib N, Kianzad Z, Zarei et al. Non-cystic macular thickening on optical coherence tomography as an alternative to fluorescein angiography for predicting retinal vascular leakage in early stages of uveitis. Sci Rep. 2022;12(1):13473. doi: 10.1038/s41598-022-17701-2.
Knickelbein JE, Tucker W, Kodati S, Akanda M, Nida Sen H. Non-invasive method of monitoring retinal vasculitis in patients with birdshot chorioretinopathy using optical coherence tomography. Br J Ophthalmol. 2018;102(6):815-820. doi: 10.1136/bjophthalmol-2016-309837.
Tian M, Tappeiner C, Zinkernagel MS, et al. Evaluation of vascular changes in intermediate uveitis and retinal vasculitis using swept-source wide-field optical coherence tomography angiography. Br J Ophthalmol. 2019 Sep;103(9):1289-1295. doi: 10.1136/bjophthalmol-2018-313078.
Palmer HE, Stanford MR, Sanders MD, Graham EM. Visual outcome of patients with idiopathic ischaemic and non-ischaemic retinal vasculitis. Eye (Lond). 1996;10(Pt 3):343-348. doi: 10.1038/eye.1996.71.
Bentley CR, Stanford MR, Shilling JS, Sanders MD, Graham EM. Macular ischaemia in posterior uveitis. Eye (Lond). 1993;7(Pt 3):411-414. doi: 10.1038/eye.1993.81.
Ostrovsky M, Ramon D, Iriqat S, et al. Retinal vascular occlusions in ocular Behçet dis ease - a comparative analysis. Acta Ophthalmol. 2023;101(6):619-626. doi: 10.1111/aos.15645.








