The International Classification of Retinopathy of Prematurity (ICROP) first came to light in 1984 due to the need for a consensus on the classification and staging of retinopathy of prematurity (ROP).1 This consensus statement enhanced the understanding of the disease and formed the framework for future treatment trials. It was later expanded in 1987 to include retinal detachment and then revisited in 2005 to further refine the ICROP classification system.2 The latter introduced new terms, including aggressive posterior ROP and pre-plus disease, with better clarification of zone 1.2 Recent advances in diagnosis and management and the variability of the disease worldwide have prompted the formation of an international ROP committee that updated the ICROP to its third edition in 2021.3 This evidence-based expert consensus by Chiang et al reflects on what has not changed from prior consensus and highlights the changes implemented by the committee, as well as relevant topics in ROP in this era.3
ZONES OF VASCULARIZATION
Unchanged Guidelines
The 3 zones from the first classification have not been modified, with zone 1 being most posterior, centered at the disc, and with a radius twice the distance between the optic disc and the fovea. Zone 2 extends from the edge of zone 1 to the ora serrata nasally, forming a ring equidistant from the disc in the other 3 quadrants. Zone 3 extends from the edge of zone 2 to the ora serrata and forms the remaining crescent.
Updated Guidelines
Because ROP in zone 2 might have a variable outcome depending on its location within this zone, the committee defined a “posterior zone 2,” which extends 2 disc diameters anteriorly from the edge of zone 1, making it more posterior and possibly more concerning. Moreover, the term “notch” was also added to indicate the presence of a 1 to 2 clock hour extension of an ROP lesion into a more posterior zone. Given that ROP is determined by the most posterior zone involved, even with predominant involvement of more peripheral zones, the specified zone would be that with the incursion and the term “secondary to notch” would be subsequently added.
PLUS DISEASE
Unchanged Guidelines
The definitions of plus disease as retinal vascular dilation and tortuosity and pre-plus disease as vascular abnormalities less severe than the former still hold true.
Updated Guidelines
Classification of plus disease is based on the appearance of the vessels in zone 1 and is along a spectrum spanning from normal to pre-plus to plus disease.
STAGES OF ROP
Unchanged Guidelines
- Stage 1, demarcation line: flat white line at the edge of the vascularized and unvascularized retina.
- Stage 2, ridge: differentiated from stage 1 by having width and height, with or without small neovascular tufts (ie, popcorn neovascularization).
- Stage 3, neovascular proliferation: extraretinal neovascularization extending into the vitreous can be from a ridge or flat appearing without an obvious ridge.
- Stage 4, partial retinal detachment: 4A, sparing the fovea, 4B involving the fovea; can be exudative or tractional.
- Stage 5, total retinal detachment.
Updated Guidelines
Stage 5 is now subcategorized as follows:
- Stage 5A, visible optic nerve head, open funnel.
- Stage 5B, optic nerve head not visible, closed funnel or retrolental fibrosis.
- Stage 5C, same as 5B but with anterior-segment changes.
Moreover, to accommodate for the presence of aggressive ROP in larger preterm infants in underdeveloped areas of the world, and to stress the importance of the time rather than location of this disease, the committee opted to rename aggressive posterior ROP. Previously also known as rush disease, the new nomenclature is aggressive ROP (A-ROP), which shows nonconformity to the typical stages of ROP. Instead, A-ROP might show early vascular changes posterior to the edge of the vascular and avascular retina, with rapid progression of neovascularization and severe plus disease.
Another update pertains to optical coherence tomography (OCT) and staging. New guidelines state that peripheral OCT coupled with scleral depression might help better stage the disease, follow-up progression, and delineate the extension of traction and/or retinal detachment.4,5
The consensus group also addressed the topic of artificial intelligence (AI) and telemedicine in ROP. Advances in machine learning and AI have been employed in multiple areas of medicine, including for diabetic retinopathy screening. The use of AI in ROP might be beneficial for earlier detection of areas at risk, more accurate staging, and follow-up after treatment or regression.6 It would be also helpful in areas with scarcity of medical professionals with adequate experience in ROP, where telemedicine can be an option to attempt to decrease the disease burden in these areas.6,7
LATER CHANGES OF ROP
Updated Guidelines
The introduction of anti-VEGF agents, as well as the long-term follow-up of ROP patients, required the introduction of new terminology to identify these changes.
- Regression: Whether following anti-VEGF intravitreal injections (fastest), laser therapy, or spontaneous. Among the many signs of regression is the decrease in plus disease, involution of neovascularization, and revascularization of the peripheral retina, whether partial or complete. The rate of spontaneous regression is stage dependent,8 and treatment with ablation of ischemic retina has been recommended for disease with higher risk of progression to retinal detachment. The Multicenter Trial of Cryotherapy for Retinopathy of Prematurity Study (CRYO-ROP) first recommended treatment in threshold disease, defined as at least 5 contiguous or 8 cumulative clock hours of stage 3 ROP with plus disease in zones 1 or 2.9 The Early Treatment for Retinopathy of Prematurity Study (ETROP) later recommended laser treatment in high-risk prethreshold ROP, known as type 1, including patients with plus disease in zone 1 (any stage); or stage 3 in zone 1 without plus disease; or stage 2 or 3 in zone 2 with plus disease.10 Treatment with anti-VEGF was later considered due to the potential for office-based treatment instead of general anesthesia, and the Bevacizumab Eliminates the Angiogenic Threat of Retinopathy of Prematurity (BEAT-ROP) trial showed benefit of bevacizumab over laser in zone 1, stage 3+ disease.11 However, recent studies have shown that sole use of anti-VEGF was associated with later onset recurrences and persistent vascular changes.12-16
- Persistent avascular retina (PAR): This term is designated for cases of incomplete revascularization. It tends to occur more frequently and over a greater extent after regression due to treatment, most notably with anti-VEGF,16-18 rather than spontaneous regression. Blair et al previously specified that in children younger than 13 years of age, ≥2 disc diameters of nonperfusion posterior to the ora is likely abnormal.19
- Reactivation: The risk of reactivation varies depending on whether regression was due to anti-VEGF treatment (highest incidence), was spontaneous, or occurred following laser treatment (lowest incidence). The timeline and clinical features or stages of reactivation also vary among patients. It’s worth noting that with reactivation, the disease might not follow the classic aforementioned stage sequence. The committee recommends documenting “reactivated” ahead of the stage when appropriate.
A CASE OF PERIPHERAL AVASCULAR RETINA
A 15-year-old male with a history of premature birth at 25 weeks gestation, ROP screening but no treatment, myopia, and anisometropic amblyopia of the left eye presented for routine optometric exam. His corrected visual acuity was 20/25 in the right eye (OD) and 20/200 in the left eye (OS) with a refraction of -6 sphere OD and -13 sphere OS. Exam revealed mild tortuosity of posterior retinal vessels as well as a temporal ridge with PAR in both eyes (Figure 1 A and B). Two years later, on routine follow-up, the patient’s visual acuity had worsened to 20/150 OD and counting fingers OS. He was noted to have bilateral subtotal macula-involving rhegmatogenous retinal detachments (Figure 1 C and D). Bilateral scleral buckling procedures with cryotherapy and external drainage were performed. Two months after his surgeries, the retinal detachments had resolved (Figure 1 E and F), and the visual acuity improved to 20/40 OD and 20/100 OS.
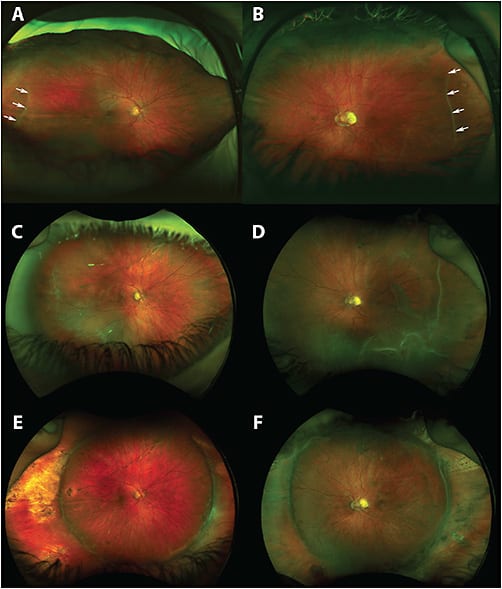
This patient developed bilateral rhegmatogenous retinal detachments in the setting of avascular retina and evidence of a regressed ridge in both eyes. This case reinforces the importance of recognizing the potential prognostic implications of such findings, especially as ultrawidefield fundus photography is performed frequently in optometric practices. It is not known whether prophylactic laser to areas of avascular retina would have decreased the risk of retinal detachment in this setting, and there is no consensus yet regarding the role for prophylactic laser in the acute setting of regressed ROP. This case exemplifies the risk of leaving avascular retina untreated (to be balanced against the risk of treating an unknown number of babies with laser who would never detach). In the absence of a clinical trial, frequent follow-up with patient education and/or prophylactic laser retinopexy would seem to be reasonable options in this high-risk population,20,21 especially considering the fact that with increasing rates of survival in extreme prematurity, the incidence of late-onset complications may also increase.15,22
LONG-TERM SEQUALAE
A history of preterm birth, with or without ROP, predisposes patients to long-term changes in the retina or retinal vasculature, including later-onset retinal detachments, retinoschisis, macular changes, PAR, straightening of the arcades, abnormal vascular branching, and glaucoma. Therefore, prolonged monitoring is important in this disease.
CONCLUSION
The recent updates by the ICROP experts serve to better stage the disease and understand its prognosis (posterior zone 2, notch, continuum of vascular abnormalities), detect aggressive features (aggressive ROP), plan treatment (subclassification of stage 5), and monitor disease response and long-term complications with emerging treatments (regression, reactivation, PAR). These changes provide enhanced understanding and diagnosis of ROP, which decreases ROP burden worldwide. RP
REFERENCES
- The Committee for the Classification of Retinopathy of Prematurity. An international classification of retinopathy of prematurity. Arch Ophthalmol. 1984;102(8):1130-1134. doi:10.1001/archopht.1984.01040030908011
- International Committee for the Classification of Retinopathy of Prematurity. The International Classification of Retinopathy of Prematurity revisited. Arch Ophthalmol. 2005;123(7):991-999. doi:10.1001/archopht.123.7.991
- Chiang MF, Quinn GE, Fielder AR, et al. International Classification of Retinopathy of Prematurity, Third Edition. Ophthalmol. 2021;128(10):e51-e68. doi:10.1016/j.ophtha.2021.05.031
- Scruggs BA, Ni S, Nguyen TP, et al. Peripheral OCT assisted by scleral depression in retinopathy of prematurity. Ophthalmol Sci. 2022;2(1):100094. doi:10.1016/j.xops.2021.100094
- Chen X, Mangalesh S, Dandridge A, et al. Spectral-domain OCT findings of retinal vascular-avascular junction in infants with retinopathy of prematurity. Ophthalmol Retina. 2018;2(9):963-971. doi:10.1016/j.oret.2018.02.001
- Scruggs BA, Chan RVP, Kalpathy-Cramer J, Chiang MF, Campbell JP. Artificial intelligence in retinopathy of prematurity diagnosis. Transl Vis Sci Technol. 2020;9(2):5. doi:10.1167/tvst.9.2.5
- Brady CJ, D’Amico S, Campbell JP. Telemedicine for retinopathy of prematurity. Telemed J E Health. 2020;26(4):556-564. doi:10.1089/tmj.2020.0010
- Ju RH, Zhang JQ, Ke XY, Lu XH, Liang LF, Wang WJ. Spontaneous regression of retinopathy of prematurity: incidence and predictive factors. Int J Ophthalmol. 2013;6(4):475-480. doi:10.3980/j.issn.2222-3959.2013.04.13
- Palmer EA. Results of U.S. randomized clinical trial of cryotherapy for ROP (CRYO-ROP). Doc Ophthalmol. 1990;74(3):245-251. doi:10.1007/BF02482615
- Good WV; Early Treatment for Retinopathy of Prematurity Cooperative Group. Final results of the Early Treatment for Retinopathy of Prematurity (ETROP) randomized trial. Trans Am Ophthalmol Soc. 2004;102:233-250.
- Mintz-Hittner HA, Kennedy KA, Chuang AZ; BEAT-ROP Cooperative Group. Efficacy of intravitreal bevacizumab for stage 3+ retinopathy of prematurity. N Engl J Med. 2011;364(7):603-615. doi:10.1056/NEJMoa1007374
- Patel RD, Blair MP, Shapiro MJ, Lichtenstein SJ. Significant treatment failure with intravitreous bevacizumab for retinopathy of prematurity. Arch Ophthalmol. 2012;130(6):801-802. doi:10.1001/archophthalmol.2011.1802
- Ittiara S, Blair MP, Shapiro MJ, Lichtenstein SJ. Exudative retinopathy and detachment: a late reactivation of retinopathy of prematurity after intravitreal bevacizumab. J AAPOS. 2013;17(3):323-325. doi:10.1016/j.jaapos.2013.01.004
- Snyder LL, Garcia-Gonzalez JM, Shapiro MJ, Blair MP. Very late reactivation of retinopathy of prematurity after monotherapy with intravitreal bevacizumab. Ophthalmic Surg Lasers Imaging Retina. 2016;47(3):280-283. doi:10.3928/23258160-20160229-12
- Al Rasheed R, Adhi MI, Alowedi SA, Albdah B, Aldebasi T, Hazzazi MA. Long-term peripheral retinal vascular behavior in retinopathy of prematurity patients treated with ranibizumab intravitreal injection as monotherapy using fluorescein angiography. Int J Retina Vitreous. 2022;8(1):53. doi:10.1186/s40942-022-00402-3
- Lepore D, Quinn GE, Molle F, et al. Follow-up to age 4 years of treatment of type 1 retinopathy of prematurity intravitreal bevacizumab injection versus laser: fluorescein angiographic findings. Ophthalmology. 2018;125(2):218-226. doi:10.1016/j.ophtha.2017.08.005
- Cheng Y, Liu TG, Li WY, Zhao MW, Liang JH. Fluorescein angiography of retinal vascular involution after intravitreal injection of ranibizumab for retinopathy of prematurity. Int J Ophthalmol. 2019;12(1):79-82. doi:10.18240/ijo.2019.01.12
- Meng QY, Cheng Y, Zhao MW, Liang JH. The process of retinal vascularization in retinopathy of prematurity after ranibizumab treatment in China. Int J Ophthalmol. 2019;12(7):1146-1150. doi:10.18240/ijo.2019.07.15
- Blair MP, Shapiro MJ, Hartnett ME. Fluorescein angiography to estimate normal peripheral retinal nonperfusion in children. J AAPOS. 2012;16(3):234-237. doi:10.1016/j.jaapos.2011.12.157
- Kaiser RS, Trese MT, Williams GA, Cox MS Jr. Adult retinopathy of prematurity: outcomes of rhegmatogenous retinal detachments and retinal tears. Ophthalmology. 2001;108(9):1647-1653. doi:10.1016/s0161-6420(01)00660-1
- Ho LY, Ho V, Aggarwal H, et al. Management of avascular peripheral retina in older prematurely born infants. Retina. 2011;31(7):1248-1254. doi:10.1097/IAE.0b013e31820d3f70
- Hanif AM, Gensure RH, Scruggs BA, Anderson J, Chiang MF, Campbell JP. Prevalence of persistent avascular retina in untreated children with a history of retinopathy of prematurity screening. J AAPOS. 2022;26(1):29-31. doi:10.1016/j.jaapos.2021.09.004








