Pediatric retinal detachment (PRD) is relatively uncommon in the United States, accounting for 3% to 13% of all retinal detachments (RDs) in the total population.1-3 It usually tends to occur in male patients age 9 to 12 years old, and its prevalence increases with age because older children have a higher risk of traumatic injury and high myopia.4,5 PRD is a unique entity because its etiologies, clinical presentations, and prognosis vary significantly from adult RD and need to be taken into consideration for optimal outcomes.6
ETIOLOGY AND RISK FACTORS
The etiologies of PRD consist of different inherited and acquired disorders, and their relative rates vary by geographic location.7,8 The common predisposing factors for PRD are trauma (44%), high myopia (15%), retinopathy of prematurity (ROP) (8%), aphakia (10%), and other etiologies (23%) such as Stickler syndrome, Knobloch syndrome, prior ocular surgery, and familial exudative vitreoretinopathy (FEVR).9-12 Pediatric RD can be classified based on its mechanisms: traumatic rhegmatogenous, tractional, and exudative. Traumatic PRD can be caused by open or closed globe injuries. Rhegmatogenous RD may occur secondary to myopia, inherited retinal disease such as Stickler syndrome, and X-linked juvenile retinoschisis (XLRS). Tractional RD (TRD) can be caused by ROP, FEVR persistent fetal vasculature (PFV), toxocariasis, and Norrie disease. Exudative PRD can be caused most typically by Coats disease and retinoblastoma.1,13
Traumatic PRD represents the most common cause of RD and has an incidence of 2.5 to 2.9 per 100,000 children annually. Traumatic PRD can be nonaccidental (eg, abuse, self-injurious behavior, eye rubbing) which portends an especially guarded prognosis, while accidental causes include projectile injury, sports-related injury, and toy gun injuries.14,15
CLINICAL PRESENTATIONS AND PROFILES
Pediatric RD is often detected later than RD in adults. Typically, presenting visual acuity is poor, and the duration of RD is difficult to attain. Many cases appear chronic at initial presentation.6,16 Pediatric RD can occasionally be missed on initial evaluation due to poor fundus visualization secondary to cooperation, media opacity, or incomplete mydriasis.17-19 Also, children tend to mask their visual deficits, which leads to delayed diagnosis.20-22 Pediatric RD usually presents bilateral with a macula-off or total RD and with concomitant proliferative vitreoretinopathy (PVR).23 Nystagmus, strabismus, esotropia, exotropia, cataract, hypotony, uveitis, and leukocoria are poor prognostic factors and indicators of chronicity.24-27
DIAGNOSTIC APPROACH
A detailed history must be taken for all children who present with PRD to identify underlying predisposing factors.11 Patients should undergo bilateral funduscopic examinations often under anesthesia if a complete comprehensive examination in clinic is not feasible.15 General anesthesia is typically used in uncooperative children when blinding disease is suspected and may include multimodal imaging such as optical coherence tomography (OCT), OCT-angiography, B-scan, anterior-segment ultrasonography, fluorescein angiography, and fundus photography. The presence of peripheral degenerations and clinical syndromes should be identified to assess the risk of detachment in the fellow eye.28
Total evaluation of the patient’s appearance, face, trunk, height, and joint mobility is highly important, and the presence of extensible skin, hypermobile digits, hearing loss, or cognitive deficits may point to a specific inherited syndrome.29,30 Depending on the suspected condition, genetic testing and screening of family members may also be advised, especially in the case of a hereditary vitreoretinopathy such as Stickler syndrome, Knobloch syndrome, Wagner disease, and Marfan syndrome.31-33 The modalities described below can be helpful in diagnosing and monitoring PRD.
B-scan
An ultrasound can be considered to rule out ocular masses, such as retinoblastoma, or in patients with a poor view of the retina due to cataract, ectopia lentis, or poorly dilating pupil. B-scan can also help differentiate TRD from exudative RD and areas of schisis and detachment in combined schisis/rhegmatogenous RD (RRD).20
Spectral-domain Optical Coherence Tomography
Spectral-domain OCT can easily be performed even on small children and can be especially helpful in the diagnosis of juvenile X-linked retinoschisis. For those patients too young to sit reliably for an in-clinic OCT, a flexible OCT may be used to obtain images during exams under anesthesia.34-36
Fluorescein Angiogram
Fluorescein angiogram is a reliable method for the evaluation of nontraumatic causes of RD, especially those with signs of exudation, uveitis, or clinical features suggestive of vascular anomalies or nonperfusion such as those observed in retinopathy of prematurity, FEVR, and Coats disease.15 Close attention should be paid for peripheral avascularity, leakage, or other vascular abnormalities, as these findings may confirm the diagnosis as well as guide the treatment of the fellow eye. The use of ultrawidefield angiography may be especially helpful for evaluation of peripheral disease.
Swept-source Widefield OCT Angiography
Swept-source widefield OCT angiography is noninvasive and may be helpful in identifying both central and peripheral vascular anomalies that can help confirm the diagnosis, but it may be difficult to perform in an uncooperative child.37
SURGICAL MANAGEMENT AND OUTCOMES
Pediatric RD has a worse prognosis than adult RD due to a higher incidence of delayed presentation and macular involvement.34 Proliferative vitreoretinopathy is more common at initial presentation and postoperatively in children, and it tends to develop subretinally, in contrast to preretinal PVR in adults.38-40
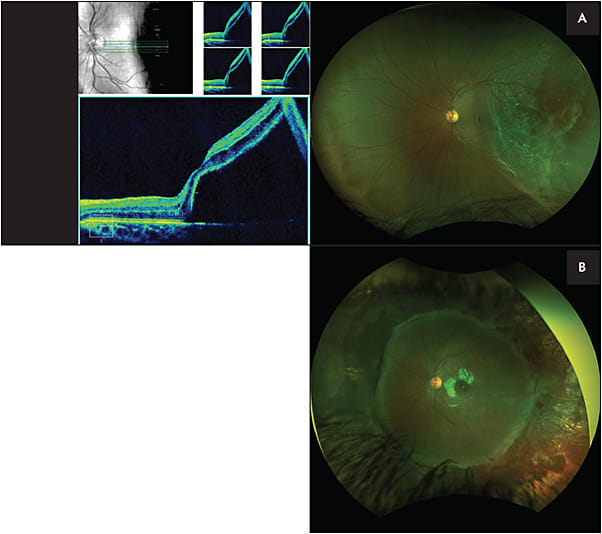
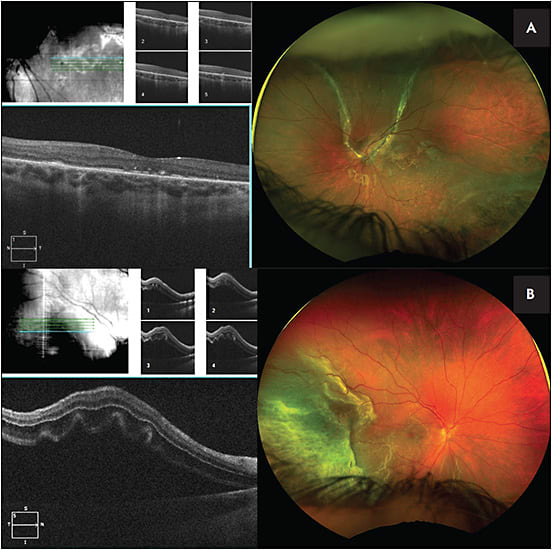
Initial treatment modalities include laser retinopexy, primary scleral buckle (SB), primary pars plana vitrectomy (PPV), and combined SB/PPV with or without lensectomy (Figures 1 and 2).41 The single-surgery success rate for all procedures in PRD repair has been estimated to be 73.3%. Reattachment rates generally are higher for traumatic etiologies and lower for congenital or developmental retinal anomalies.4,5,25 Among all forms of PRD, traumatic RD and RRD have a better anatomical success rate (78%) than TRD (39%). Despite a wide range of surgical approaches, PRD has a low surgical success rate of reattachment compared to adult RD.1,15 Even with successful anatomic reattachment, eyes are often at risk of amblyopia. Comanagement with a visual development specialist or pediatric ophthalmologist is essential to maximizing functional outcomes in the PRD patient.42
Scleral Buckling
Primary SB is considered a highly useful technique in treatment of PRD. Primary SB provides a higher surgical success rate (79%) compared with PPV alone (64.5%) and even combined SB/PPV (67.2%) in PRD. In contrast, for adult RRD, a similar success rate of reattachment is reported between SB/PPV and SB alone. Primary SB in PRD also has a lower risk of complications and subsequent need for secondary surgeries.4,43-45 Primary SB is especially useful in treatment of dialysis-related RD and detachments in high myopes caused by lattice and holes.34 Mild PVR in PRD can be managed with standalone SB (larger buckle elements such as 42 bands and 287 tires), but in complicated RD, SB alone may be insufficient, and combined SB/PPV may be considered.23,41 In traumatic PRD with open-globe injury, SB should be placed at the time of closing the globe or within 1 to 2 weeks after that to minimize the risk of conjunctival or Tenon scarring and permanent vision loss.15 Patients under 2 years old may need band division to avoid amblyopia 3 to 6 months after surgery if eye growth is restricted.42
Pars Plana Vitrectomy
The success rate in primary PPV is significantly lower than primary SB or even a combined SB/PPV, therefore recent studies emphasize the need for adding SB in most PRD cases.18,34
Pediatric PPV requires an aged-based method for sclerotomy placement to avoid iatrogenic damage to the crystalline lens and peripheral retina. The changes of ciliary body dimensions during ocular development are especially dramatic in the first 2 years of life, with a second growth spurt occurring around puberty.46,47 Pediatric sclera also has different structural characteristics with lower rigidity and its wounds are generally more likely to leak. Therefore, suturing sclerotomies at the conclusion of the vitrectomy is recommended in children as they may be more prone to rubbing, insufficient hygiene, and incomplete positioning.42
The pediatric vitreous is often more formed than the adult vitreous, so it can help to create tamponade during SB by bringing the retinal pigment epithelium closer to the retinal break. Furthermore, the retinal pigment epithelium tends to be healthier and is better able to pump subretinal fluid postoperatively.4,48 Also, the firm adherence of the pediatric cortical vitreous makes PPV more challenging in children than adults, leading to the potential for iatrogenic retinal breaks during induction of posterior vitreous detachment (PVD), incomplete PVD induction with subsequent contraction, and recurrent detachment.49 In these cases, PVD induction can be assisted by dilute triamcinolone staining and flexible loop scraping. Segmentation can be an alternative to delamination for preretinal fibrous tissue removal.15,49
Considering the positioning requirements and travel restrictions with gas tamponade, silicone oil is often the preferred tamponade in vitrectomy for PRD. However, it can emulsify and be associated with complications such as elevated intraocular pressure, cataract formation, and band keratopathy (especially in cases of aphakic oil).27,50
Pars plana vitrectomy carries a higher risk of complications than SB in PRD; however, it is an unavoidable choice for complicated cases such as RD with severe PVR (grade C or worse), vitreous hemorrhage or haze, coexistence of cataract or lens subluxation, giant or multiple posterior or radial tears, coloboma, or recurrent RRD.5,51
A lens-sparing vitrectomy is ideal for PRD for the prevention of amblyopia and glaucoma; however, cases with choroidal detachment or funnel RDs may need a limbal approach with lensectomy.15,49,52 Phacoemulsification can be employed in select cases if a lens opacity prohibits adequate visualization. If planning for lensectomy in PRD, it is recommended to remove the entire capsular bag to decrease the scaffold for subsequent PVR. Intraocular lens placement is usually not advisable at the time of lensectomy. Secondary lenses or contact lenses may be used once the eye is stable for the management of aphakia.15
Scleral Buckling and Pars Plana Vitrectomy
Children with complex RDs who are candidates for vitrectomy tend to have better long-term anatomic and functional results with SB and PPV compared to primary PPV.53,54 A recent IRIS Registry (Intelligent Research in Sight) analysis showed that children with complex RD most commonly require a mean of 1.68 procedures to achieve retinal reattachment.41 Combined SB and PPV in PRD can support the vitreous base, decreases retinectomy needs, manage incomplete vitreous removal, and preserve crystalline lens, which causes a lower risk of postoperative inflammation, amblyopia, and aphakic glaucoma.18,55
CLINICAL TIPS AND OTHER SURGICAL CONSIDERATIONS
Bilateral PRD is not uncommon, so many surgeons may consider prophylactic 360° laser retinopexy for fellow eyes with a high risk for detachment.56 In cases of bilateral simultaneous RD, same-day bilateral surgery may be considered in some cases with anesthesia risk or significant systemic comorbidities.57,58
Preoperative laser panretinal photocoagulation and intravitreal anti-VEGF injection may play a role in managing PRD, especially in ROP, FEVR, and other vascular conditions.12,59-64 Self-inflicted RD creates unique considerations due to bilateral injury, continuous traumatic behavior, and recurrent RD. In cases of unilateral RD, repetitive self-injurious behavior may warrant a prophylactic SB with laser in the fellow eye. In addition, behavioral therapy, psychiatric medications, and protective devices such as protective eyewear help mitigate traumatic injury.65
CONCLUSION
Retinal detachments in the pediatric population are uncommon but portend significant challenges in management. Primary SB should be considered as an initial treatment in many PRDs, although other surgical modalities such as combined SB and PPV may be needed to tailor the treatment to the situation. A thorough and thoughtful preoperative assessment with early intervention can engender higher success of reattachments. Additional complications such as amblyopia need to be actively managed along with the retinal disease for the most favorable visual outcomes in this population. Protective eyewear should be considered especially in monocular patients and self-induced traumatic PRD. RP
REFERENCES
- Read SP, Aziz HA, Kuriyan A, et al. Retinal detachment surgery in a pediatric population: visual and anatomic outcomes. Retina. 2018;38(7):1393-1402. doi:10.1097/IAE.0000000000001725
- Van de Put MAJ, Hooymans JMM, Los LI; Dutch Rhegmatogenous Retinal Detachment Study Group. The incidence of rhegmatogenous retinal detachment in The Netherlands [published correction appears in Ophthalmology. 2018 Jul;125(7):1127]. Ophthalmology. 2013;120(3):616-622. doi:10.1016/j.ophtha.2012.09.001
- Meier P. [Retinal detachment in children: differential diagnosis and current therapy]. Klin Monbl Augenheilkd. 2008;225(9):779-790. doi:10.1055/s-2008-1027515
- Starr MR, Boucher N, Sharma C, et al. The state of pediatric retinal detachment surgery in the United States: a nationwide aggregated health record analysis. Retina. 2023;43(5):717-722. doi:10.1097/IAE.0000000000003735
- Nuzzi R, Lavia C, Spinetta R. Paediatric retinal detachment: a review. Int J Ophthalmol. 2017;10(10):1592-1603. doi:10.18240/ijo.2017.10.18
- Archambault C, Azad AD, Al-Moujahed A, Vail D, Wood E, Koo EB. Time to treatment of pediatric retinal detachments: a US claims-based analysis. Ophthalmol Retina. 2023;7(3):221-226. doi:10.1016/j.oret.2022.08.017
- Gan NY, Lam WC. Retinal detachments in the pediatric population. Taiwan J Ophthalmol. 2018;8(4):222-236. doi:10.4103/tjo.tjo_104_18
- Tsai ASH, Wong CW, Lim L, et al. Pediatric retinal detachment in an Asian population with high prevalence of myopia: clinical characteristics, surgical outcomes, and prognostic factors. Retina. 2019;39(9):1751-1760. doi:10.1097/IAE.0000000000002238
- Reddy DN, Yonekawa Y, Thomas BJ, Nudleman ED, Williams GA. Long-term surgical outcomes of retinal detachment in patients with Stickler syndrome. Clin Ophthalmol. 2016;10:1531-1534. doi:10.2147/OPTH.S111526
- Soliman MM, Macky TA. Pediatric rhegmatogenous retinal detachment. Int Ophthalmol Clin. 2011;51(1):147-171. doi:10.1097/IIO.0b013e31820099c5
- Agrawal V, Kalia S. Management and surgical outcomes of pediatric retinal detachment associated with familial exudative vitreoretinopathy - our experience at a tertiary care ophthalmic center in North India. Indian J Ophthalmol. 2022;70(7):2490-2496. doi:10.4103/ijo.IJO_2292_21
- Peng J, Liang T, Chen C, et al. Subretinal injection of ranibizumab in advanced pediatric vasoproliferative disorders with total retinal detachments. Graefes Arch Clin Exp Ophthalmol. 2020;258(5):1005-1012. doi:10.1007/s00417-020-04600-3
- Naravane AV, Belin PJ, Pierce B, Quiram PA. Risk and prevention of retinal detachments in patients with Stickler syndrome. Ophthalmic Surg Lasers Imaging Retina. 2022;53(1):7-11. doi:10.3928/23258160-20211213-02
- Gonzales CR, Singh S, Yu F, Kreiger AE, Gupta A, Schwartz SD. Pediatric rhegmatogenous retinal detachment: clinical features and surgical outcomes. Retina. 2008;28(6):847-852. doi:10.1097/IAE.0b013e3181679f79
- Hoyek S, Baldwin G, Patel N. Pediatric traumatic retinal detachments. In: Özdek Ş, Berrocal A, Spandau U, eds. Pediatric Vitreoretinal Surgery. Springer; 2023:493-503. doi:10.1007/978-3-031-14506-3_34
- Portney DS, Jacobson A, Liles N, Bohnsack BL, Besirli CG. Characteristics of retinal detachment after pediatric open-globe injuries. Ophthalmol Retina. 2021;5(11):1175-1177. doi:10.1016/j.oret.2021.04.011
- Felfeli T, Mireskandari K, Ali A. Long-term outcomes of pediatric traumatic cataracts and retinal detachments due to self-inflicted injuries. Eur J Ophthalmol. 2021;31(1):271-276. doi:10.1177/1120672120926452
- Ghoraba HH, Mansour HO, Abdelhafez MA, et al. Comparison between pars plana vitrectomy with and without encircling band in the treatment of pediatric traumatic rhegmatogenous retinal detachment. Clin Ophthalmol. 2020;14:3271-3277. doi:10.2147/OPTH.S275778
- Rahimi M, Bagheri M, Nowroozzadeh MH. Characteristics and outcomes of pediatric retinal detachment surgery at a tertiary referral center. J Ophthalmic Vis Res. 2014;9(2):210-214.
- Wenick AS, Barañano DE. Evaluation and management of pediatric rhegmatogenous retinal detachment. Saudi J Ophthalmol. 2012;26(3):255-263. doi:10.1016/j.sjopt.2012.04.005
- Abdi F, Aghajani A, Hemmati S, et al. Pediatric rhegmatogenous retinal detachment: A meta-analysis of clinical features, surgical success rate, and prognostic factors. Indian J Ophthalmol. 2023;71(3):717-728. doi:10.4103/ijo.IJO_643_22
- Rejdak R, Nowakowska D, Wrona K, Maciejewski R, Junemann AG, Nowomiejska K. Outcomes of vitrectomy in pediatric retinal detachment with proliferative vitreoretinopathy. J Ophthalmol. 2017;2017:8109390. doi:10.1155/2017/8109390
- Sparks ME, Davila PJ, He YG, Wang AL. Pediatric rhegmatogenous retinal detachments: etiologies, clinical course, and surgical outcomes. J Vitreoretin Dis. 2023;7(2):139-143. doi:10.1177/24741264221150595
- Brown AC, Nwanyanwu K. Retinopathy of prematurity. StatPearls. 2023.
- Gurler B, Coskun E, Öner V, Comez A, Erbagci I. Clinical characteristics and surgical outcomes of pediatric rhegmatogenous retinal detachment. Int Ophthalmol. 2016;36(4):521-525. doi:10.1007/s10792-015-0158-3
- Eibenberger K, Sacu S, Rezar-Dreindl S, Schmidt-Erfurth U, Stifter E, Georgopoulos M. Clinical characteristics and surgical outcome of pediatric and early adulthood retinal detachment. Eur J Ophthalmol. 2021;31(3):1367-1374. doi:10.1177/1120672120913030
- Wadhwa N, Venkatesh P, Sampangi R, Garg S. Rhegmatogenous retinal detachments in children in India: clinical characteristics, risk factors, and surgical outcomes. J AAPOS. 2008;12(6):551-554. doi:10.1016/j.jaapos.2008.05.002
- Wu H, Xie Z, Wang P, et al. Differences in retinal and choroidal vasculature and perfusion related to axial length in pediatric anisomyopes. Invest Ophthalmol Vis Sci. 2021;62(9):40. doi:10.1167/iovs.62.9.40
- Coussa RG, Sears J, Traboulsi EI. Stickler syndrome: exploring prophylaxis for retinal detachment. Curr Opin Ophthalmol. 2019;30(5):306-313. doi:10.1097/ICU.0000000000000599
- Lee AC, Greaves GH, Rosenblatt BJ, et al. Long-term follow-up of retinal detachment repair in patients with Stickler syndrome. Ophthalmic Surg Lasers Imaging Retina. 2020;51(11):612-616. doi:10.3928/23258160-20201104-02
- Morris RE, Kuhn F. Retinal detachments in stickler syndrome. Ophthalmic Surg Lasers Imaging Retina. 2022;53(9):522-523. doi:10.3928/23258160-20220815-03
- Soh Z, Richards AJ, McNinch A, Alexander P, Martin H, Snead MP. Dominant Stickler syndrome. Genes (Basel). 2022;13(6):1089. doi:10.3390/genes13061089
- Parra MM, Spoth E, Ronquillo CC, Henderson R, Hartnett ME. Multimodal retinal imaging findings in two cousins with VCAN-related vitreoretinopathy or Wagner disease. Ophthalmic Surg Lasers Imaging Retina. 2022;53(11):639-643. doi:10.3928/23258160-20221026-01
- Drenser K. Pearls for managing pediatric retinal detachments. Ophthalmology. 2019;126(9):1271-1272. doi:10.1016/j.ophtha.2019.03.022
- Sin HPY, Yip WWK, Chan VCK, Young AL. Etiologies and surgical outcomes of pediatric retinal detachment in Hong Kong. Int Ophthalmol. 2017;37(4):875-883. doi:10.1007/s10792-016-0287-3
- McElnea E, Stephenson K, Gilmore S, O’Keefe M, Keegan D. Paediatric retinal detachment: aetiology, characteristics and outcomes. Int J Ophthalmol. 2018;11(2):262-266. Published 2018 Feb 18. doi:10.18240/ijo.2018.02.14
- Nguyen TP, Ni S, Liang G, et al. Widefield optical coherence tomography in pediatric retina: a case series of intraoperative applications using a prototype handheld device. Front Med (Lausanne). 2022;9:860371. doi:10.3389/fmed.2022.860371
- Puodžiuvienė E, Jokūbauskienė G, Vieversytė M, Asselineau K. A five-year retrospective study of the epidemiological characteristics and visual outcomes of pediatric ocular trauma. BMC Ophthalmol. 2018;18(1):10. doi:10.1186/s12886-018-0676-7
- Mandviwala MM, Sassani PP. Traumatic retinal detachment caused by Nerf gun shot in a pediatric patient. Retin Cases Brief Rep. 2021;15(5):568-570. doi:10.1097/ICB.0000000000000853
- Al-Moujahed A, Saleh S, Ghoraba H, Nguyen QD, Wood E. Systemic and intraocular methotrexate for the prevention and treatment of proliferative vitreoretinopathy in children with rhegmatogenous retinal detachment and underlying inflammatory disease. J Vitreoretin Dis. 2022;6(5):399-404. doi:10.1177/24741264221076357
- Belin PJ, Naravane AV, Lu S, Li C, Lum F, Quiram PA. Vitreoretinopathy-associated pediatric retinal detachment treatment outcomes: IRIS Registry (Intelligent Research in Sight) analysis. Ophthalmol Sci. 2023;3(3):100273. doi:10.1016/j.xops.2023.100273
- Gan NY, Lam WC. Special considerations for pediatric vitreoretinal surgery. Taiwan J Ophthalmol. 2018;8(4):237-242. doi:10.4103/tjo.tjo_83_18
- Errera MH, Liyanage SE, Moya R, Wong SC, Ezra E. Primary scleral buckling for pediatric rhegmatogenous retinal detachment. Retina. 2015;35(7):1441-1449. doi:10.1097/IAE.0000000000000480
- Nichani PAH, Dhoot AS, Popovic MM, et al. Scleral buckling alone or in combination with pars plana vitrectomy for rhegmatogenous retinal detachment repair: a meta-analysis of 7,212 eyes. Ophthalmologica. 2022;245(4):296-314. doi:10.1159/000524888
- Papageorgiou E, Riri K, Kardaras D, et al. Scleral buckling surgery for stage 4A and 4B retinopathy of prematurity in critically ill neonates. Int Ophthalmol. 2022;42(4):1093-1100. doi:10.1007/s10792-021-02095-3
- Lemley CA, Han DP. An age-based method for planning sclerotomy placement during pediatric vitrectomy: a 12-year experience. Trans Am Ophthalmol Soc. 2007;105:86-91.
- Wright LM, Harper CA 3rd, Chang EY. Management of infantile and childhood retinopathies: optimized pediatric pars plana vitrectomy sclerotomy nomogram. Ophthalmol Retina. 2018;2(12):1227-1234. doi:10.1016/j.oret.2018.06.008
- Yonekawa Y, Fine HF. Practical pearls in pediatric vitreoretinal surgery. Ophthalmic Surg Lasers Imaging Retina. 2018;49(8):561-565. doi:10.3928/23258160-20180803-02
- Patel NA, Berrocal AM. Induction of posterior vitreous detachment in pediatric patients by radial perifoveal stripping. Retin Cases Brief Rep. 2022;16(4):470-472. doi:10.1097/ICB.0000000000001010
- Mishra S, Wadhwani M, Kumar A, Chauhan R. Outcome of pediatric retinal detachment using high-density silicone oil. Int Ophthalmol. 2021;41(2):575-580. doi:10.1007/s10792-020-01611-1
- Al Abdulsalm O, Al Habboubi H, Mura M, Al-Abdullah A. Re-vitrectomy versus combined re-vitrectomy with scleral buckling for pediatric recurrent retinal detachment. Clin Ophthalmol. 2022;16:877-884. doi:10.2147/OPTH.S356993
- Turgut B, Demir T, Çatak O. The recommendations for pediatric vitreoretinal surgery. Adv Ophthalmol Vis Syst. 2019;9(6):142-145. DOI:10.15406/aovs.2019.09.00366
- Ong SS, Ahmed I, Gonzales A, et al. Vitrectomy versus vitrectomy with scleral buckling in the treatment of giant retinal tear related retinal detachments: an international multicenter study. Ophthalmol Retina. 2022;6(7):595-606. doi:10.1016/j.oret.2022.03.004
- Carranza-Casas M, Quiroz-González E, Hernández-Reyes A, Matsui-Serrano R, Ariza-Camacho E, Graue-Wiechers F. Pediatric rhegmatogenous retinal detachment: predictors of anatomic and functional success. Int Ophthalmol. 2021;41(8):2777-2788. doi:10.1007/s10792-021-01834-w
- Ghoraba HH, El Gouhary SM, Ghali AAA, et al. Pars plana vitrectomy with/without encircling scleral band for treatment of retinal detachment associated with buphthalmos. Int J Retina Vitreous. 2021;7(1):39. doi:10.1186/s40942-021-00310-y
- Cadis C, Wang A, Julakanti M, Juergens A. Bilateral retinal detachment in a pediatric patient. J Emerg Med. 2019;56(4):e55-e57. doi:10.1016/j.jemermed.2018.12.031
- Ang GS, Townend J, Lois N. Interventions for prevention of giant retinal tear in the fellow eye. Cochrane Database Syst Rev. 2012;2012(2):CD006909. doi:10.1002/14651858.CD006909.pub3
- Sindal MD, Gondhale HP, Srivastav K. Clinical profile and outcomes of rhegmatogenous retinal detachment related to trauma in pediatric population. Can J Ophthalmol. 2021;56(4):231-236. doi:10.1016/j.jcjo.2020.12.001
- Fei P, Yang W, Zhang Q, Jin H, Li J, Zhao P. Surgical management of advanced familial exudative vitreoretinopathy with complications. Retina. 2016;36(8):1480-1485. doi:10.1097/IAE.0000000000000961
- Yamane T, Yokoi T, Nakayama Y, Nishina S, Azuma N. Surgical outcomes of progressive tractional retinal detachment associated with familial exudative vitreoretinopathy. Am J Ophthalmol. 2014;158(5):1049-1055. doi:10.1016/j.ajo.2014.08.009
- VanderVeen DK, Melia M, Yang MB, Hutchinson AK, Wilson LB, Lambert SR. Anti-vascular endothelial growth factor therapy for primary treatment of type 1 retinopathy of prematurity: a report by the American Academy of Ophthalmology. Ophthalmology. 2017;124(5):619-633. doi:10.1016/j.ophtha.2016.12.025
- Todorich B, Thanos A, Yonekawa Y, Capone A Jr. Repair of total tractional retinal detachment in norrie disease: report of technique and successful surgical outcome. Ophthalmic Surg Lasers Imaging Retina. 2017;48(3):260-262. doi:10.3928/23258160-20170301-11
- Danford ID, Scruggs BA, Capone A Jr, et al. The prevalence of retinal disease and associated cns disease in young patients with incontinentia pigmenti. Ophthalmol Retina. 2022;6(12):1113-1121. doi:10.1016/j.oret.2022.05.032
- Qiang Kwong T, Shunmugam M, Williamson TH. Characteristics of rhegmatogenous retinal detachments secondary to retinal dialyses. Can J Ophthalmol. 2014;49(2):196-199. doi:10.1016/j.jcjo.2013.12.013
- Rossin EJ, Tsui I, Wong SC, et al. Traumatic retinal detachment in patients with self-injurious behavior: an international multicenter study. Ophthalmol Retina. 2021;5(8):805-814. doi:10.1016/j.oret.2020.11.012








