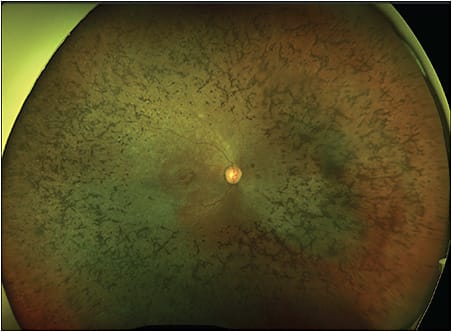
Following the success of voretigene neparvovec-rzyl (Luxturna; Spark Therapeutics) for biallelic RPE65 mutation-associated retinal dystrophy, patients struggling with inherited retinal disease (IRD) such as Usher syndrome (Figure 1) now approach their retinal physicians with hopeful optimism. For the first time, an FDA-approved gene therapy has demonstrated measurable benefit for patients.1 Naturally, this has spurred considerable interest in gene therapy for a multitude of IRDs and — creatively — other VEGF-driven pathology such as exudative macular degeneration. These advances are more thoroughly reviewed in other recent publications in longer format beyond the scope of this article.2,3
Increasingly, patients suffering from IRDs and their families inquire about ongoing and future gene therapy trials. How should an informed retinal physician consider the ongoing clinical trial results and share that news with patients? A useful lens through which to view each gene therapy clinical trial asks 2 key questions:
- Does the novel gene therapy impact the natural pathophysiology of the disease in a measurable and durable way? and
- What is the inflammatory response to the therapy?
Although there are other adverse events to consider, increasingly, the degree and longevity of intraocular inflammation after viral delivery of often exogenous gene products feature prominently in the dosing and defined therapeutic window of intraocular gene therapy.
GENE THERAPY APPROACHES
When discussing the mechanics of “gene therapy” with inquiring patients, the retinal physician might explain the approaches of either gene augmentation or gene editing, with the former comprising most of the existing therapies to date. Adeno-associated viral (AAV) vectors, by far the most widely used, provide target cells a working copy of the missing gene in a process called transduction. Critically, this genetic material is not integrated into the host genome but rather kept in the nucleus as episomal DNA. Because the entire field of intraocular gene therapy is still young, real questions remain about long-term durable treatment effect of episomal DNA in gene augmentation approaches, especially as they are applied to young children.
Gene editing, on the other hand, uses “molecular scissors” of the CRISPR-Cas9 technology to excise and replace faulty genes. There are additional technical hurdles involved in editing the host chromatin, and questions remain regarding safety of off-target interaction with the genome.
Excluding clinical trials that focus on VEGF-driven disease, there are currently 10 active and enrolling gene therapy clinical trials listed on clinicaltrials.gov for IRDs. Others are planned but not yet enrolling and still other trials have completed enrollment and are now ongoing. At present, the enrolling clinical trials target X-linked retinitis pigmentosa, PDE6A-related retinitis pigmentosa, RPGR-related retinitis pigmentosa, nonsyndromic retinitis pigmentosa, Bietti crystalline dystrophy, and CEP290-associated Leber congenital amaurosis. Additionally, there have been encouraging results with Gucy2d-associated Leber congenital amaurosis.4
GENE THERAPY TREATMENT EFFECT
Recently, an instructive paper was published detailing the 12-month results from intravitreal injections of AAV (rAAV2tYF-CB-hRS1) for patients with X-linked retinoschisis.5 Therein, the authors highlight that their gene augmentation strategy did not demonstrate a measurable improvement for patients as investigated with visual acuity, visual field, full field ERG, or OCT.
Considering the above first key question, these 12-month data do not yet yield a measurable and durable improvement of the pathophysiology of the disease. The trial is set to follow patients for 5 years, and forthcoming results may well be more positive, especially considering the natural course of X-linked retinoschisis. If successful, the retinas of treated eyes may well stabilize the macula and experience less macular atrophy, perhaps revealing that finding over time.
INFLAMMATORY RESPONSE
When the second above key question is posed, the authors do provide considerable detail regarding intraocular inflammation. While intravitreal injection was generally well tolerated, 11 patients (40.7%) developed keratic precipitates, with 7 patients (53.8%) in the high-dose (6x1011 vg/eye) arm doing so. Of these, 3 high-dose patients (23.1%) went on to develop chronic uveitis despite immunosuppressive therapy. Two patients developed retinal detachments, perhaps attributable to underlying disease. In their thoughtful discussion, the authors suggested that inflammation resulted from administration, rather than in response to foreign protein transduction and expression, because antibodies to the transcribed retinoschisin protein remained low. They postulate that combined with other factors, “the observed inflammatory response, may explain, at least in part, the lack of overall efficacy observed.” Additionally, the authors suggest that future clinical protocols use a prophylactic anti-inflammatory regimen, citing that none of their patients with sub-Tenon triamcinolone developed chronic uveitis.
These inflammatory challenges are not unique to this trial for X-linked retinoschisis, but rather shared virtually amongst all virally administered retinal gene therapies. More generally, virally delivered gene augmentation strategies face challenges at both ends of the therapeutic window, as was demonstrated during the INFINITY trial evaluating ADVM-022 for treatment of diabetic macular edema.6 Questions remain regarding long-term durability of treatment effect with Luxturna, citing macular atrophy with postulated insult from viral toxicity, mechanics of subretinal delivery, or inflammation — although only 11% of eyes were found to have signs of inflammation.7
EXPANDING THE THERAPEUTIC WINDOW
When applying the 2 key questions above, the first question of measurable and durable impact on disease speaks to the floor of the therapeutic window, below which there is no treatment effect. Often, the measurable change is hard to discern in IRD disease states over time. Patients may be young and have other syndromic findings, making subjective and visual field testing difficult. Sometimes, it is unclear what subjective improvements have been made over time. The second key question regarding inflammation is a critical driver of the height of the ceiling of the therapeutic window, above which toxicity limits efficacy and safety. As detailed in the above report and others, there is often a dose-related inflammation from intravitreal AAV administration. Both considerations coalesce to produce a narrow therapeutic window, which is a challenge for clinical trial design and ultimate approval of new therapy.
To expand the therapeutic window, consideration is now given to both the floor and ceiling in pending clinical trials.8 For efficacy at the floor, some suggest validated measures in line with National Institutes of Health and Food and Drug Administration guidelines, which can find therapeutic effect even when more subjective measures fall short. Considerable effort was invested toward these goals to bring Luxturna to approval, including development and validation of multiluminance mobility testing,9 full-field light sensitivity threshold testing,10 and pupillometry, which is useful in young children.11 These additional measures are vital because traditional electroretinography may not show robust improvement whereas other measures do, as was the case with Luxturna.8 More comprehensively, natural history studies inform clinical trial design for disease-specific factors that show the sharpest decline over time and offer the largest signal to capture for treatment effect.
MITIGATING TOXICITY AND INFLAMMATION
To address the ceiling of toxicity and inflammation in particular, robust steroid treatment and need for immunomodulatory therapy should be included in study design. Gene therapy–associated uveitis denotes, “intraocular inflammation that is recurrent, chronic, and/or more severe or greater in duration than expected for the surgical procedure alone.”5,12 Furthermore, multiple reports suggest administration outside of the vitreous produces a more limited inflammatory response.13 Subretinal delivery, as is the case in Luxturna and others, avoids exposing the ciliary body, iris, and lens to the viral vector while maintaining it relatively encapsulated within the immune-privileged subretinal space. Although rare, mild to moderate inflammatory responses have occurred with subretinal delivery, as was the case with CNGA3-associated and CNGB3-associated achromatopsia.14 The subretinal space can be accessed via a 41-gauge canula after vitrectomy or through a limited anterior sclerotomy into the subretinal space.15 Alternatively, the suprachoroidal space can now be accessed reliably through the sclera, with retina-wide expression following AAV8 administration.16 Some inflammation will be tolerated, given there are no proven alternative therapies for IRDs or a library of biosimilar options. However, recent results behoove scientists, clinical trial consultants, and the treating retinal physician to consider inflammation seriously.
CONCLUSION
While much work remains from bench to bedside, the practicing retinal physician today can evaluate and inform patients of IRD gene therapy clinical trials with the following 2 key questions in mind. First, does the novel gene therapy impact the natural pathophysiology of the disease in a measurable and durable way? Second, what is the inflammatory response to the therapy? Answers to these questions are central to the ultimate success of each therapy and are driving innovation in the expanding and exciting field of retina gene therapy. RP
REFERENCES
- Russell S, Bennett J, Wellman JA, et al. Efficacy and safety of voretigene neparvovec (AAV2-hRPE65v2) in patients with RPE65-mediated inherited retinal dystrophy: a randomised, controlled, open-label, phase 3 trial [published correction appears in Lancet. 2017 Aug 26;390(10097):848]. Lancet. 2017;390(10097):849-860. doi:10.1016/S0140-6736(17)31868-8
- Khanani AM, Thomas MJ, Aziz AA, et al. Review of gene therapies for age-related macular degeneration. Eye (Lond). 2022;36(2):303-311. doi:10.1038/s41433-021-01842-1
- Nuzbrokh Y, Ragi SD, Tsang SH. Gene therapy for inherited retinal diseases. Ann Transl Med. 2021;9(15):1278. doi:10.21037/atm-20-4726
- Boye SL, O’Riordan C, Morris J, et al. Preclinical studies in support of phase I/II clinical trials to treat GUCY2D-associated Leber congenital amaurosis. Mol Ther Methods Clin Dev. 2022;28:129-145. doi:10.1016/j.omtm.2022.12.007
- Pennesi ME, Yang P, Birch DG, et al. Intravitreal delivery of rAAV2tYF-CB-hRS1 vector for gene augmentation therapy in patients with X-linked retinoschisis: 1-year clinical results. Ophthalmol Retina. 2022;6(12):1130-1144. doi:10.1016/j.oret.2022.06.013
- Adverum. Adverum reports first quarter 2021 results. News release. May 6, 2021. Accessed February 6, 2023. https://investors.adverum.com/news/news-details/2021/Adverum-Reports-First-Quarter-2021-Results-2021-5-6-2021-5-6/default.aspx
- Gange WS, Sisk RA, Besirli CG, et al. Perifoveal chorioretinal atrophy after subretinal voretigene neparvovec-rzyl for RPE65-mediated Leber congenital amaurosis. Ophthalmol Retina. 2022;6(1):58-64. doi:10.1016/j.oret.2021.03.016
- Sofia F, Cerolini S, Durham T. Report from a workshop on accelerating the development of treatments for inherited retinal dystrophies associated with mutations in the RDH12 gene. Transl Vis Sci Technol. 2020;9(8):30. doi:10.1167/tvst.9.8.30
- Chung DC, McCague S, Yu ZF, et al. Novel mobility test to assess functional vision in patients with inherited retinal dystrophies. Clin Exp Ophthalmol. 2018;46(3):247-259. doi:10.1111/ceo.13022
- Messias K, Jagle H, Saran R, et al. Psychophysically determined full-field stimulus thresholds (FST) in retinitis pigmentosa: relationships with electroretinography and visual field outcomes. Doc Ophthalmol. 2013;127(2):123-129.
- Melillo P, Pecchia L, Testa F, Rossi S, Bennett J, Simonelli F. Pupillometric analysis for assessment of gene therapy in Leber congenital amaurosis patients. Biomed Eng Online. 2012;11:40. Published 2012 Jul 19. doi:10.1186/1475-925X-11-40
- Pennesi ME, Gregory-Evans K, Yang P. Retinitis pigmentosa and allied disorders. In SR Sadda, ed. Ryan’s Retina. Elsevier; 2022.
- Bucher K, Rodríguez-Bocanegra E, Dauletbekov D, Fischer MD. Immune responses to retinal gene therapy using adeno-associated viral vectors - Implications for treatment success and safety. Prog Retin Eye Res. 2021;83:100915. doi:10.1016/j.preteyeres.2020.100915
- AGTC. Twelve-month findings from two phase 1/2 clinical trials of subretinal gene therapy for achromatopsia. News release. September 29, 2021. Accessed February 6, 2023. https://agtc.com/wp-content/uploads/2021/12/Huckfeldt-final-RD2021-slides-9-28-21_press-release.pdf
- de Smet MD, Lynch JL, Dejneka NS, Keane M, Khan IJ. A subretinal cell delivery method via suprachoroidal access in minipigs: safety and surgical outcomes. Invest Ophthalmol Vis Sci. 2018;59(1):311-320. doi:10.1167/iovs.17-22233
- Ding K, Shen J, Hafiz Z, et al. AAV8-vectored suprachoroidal gene transfer produces widespread ocular transgene expression. J Clin Invest. 2019;129(11):4901-4911. doi:10.1172/JCI129085








