Retinoblastoma (RB) is the most common intraocular cancer of childhood, accounting for approximately 11% of cancers occurring in the first year of life, with 95% diagnosed before 5 years of age.1 The global burden of RB is in the Asia-Pacific region and Africa, with the United States contributing less than 5% of all cases (approximately 250 cases per year).2
DIAGNOSIS
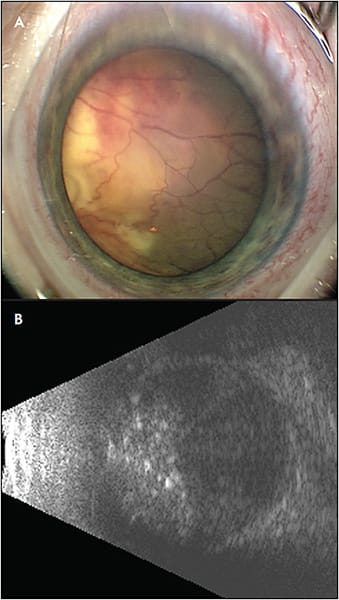
The diagnosis of RB is clinical based on a constellation of symptoms (leukocoria, absent pupil light reflex, and strabismus) and findings of whitish retinal mass with calcification and seeding observed during examination under anesthesia (EUA). Supported by ancillary studies such as ultrasound B-scan and fluorescein angiography, it is possible to differentiate RB from masquerade entities such as Coats disease, persistent fetal vasculature, retinal dysplasia, or astrocytic hamartoma.
STAGING
The key to globe salvation and vision preservation in RB depends on early diagnosis and appropriate treatment.3 Extraocular (orbital) and metastatic RB are rarely observed in the United States. Intraocular RB classification is an essential component of management because it guides the treatment, determines prognosis, and is essential for assessing treatment outcomes.4 The International Classification for Intraocular Retinoblastoma (ICRB) classifies tumors from A through E based on size (A; small tumors), location (B; macular or juxtapapillary location), extent of seeding (C; localized subretinal or vitreous seeding or D; diffuse), and complications (E; neovascular glaucoma, phthisis bulbi, aseptic orbital cellulitis, diffuse vitreous hemorrhage).
TREATMENT PRINCIPLES
Retinoblastoma management remains complex, requiring individualized treatment based on age at presentation, laterality, location, ICRB staging, compartmental involvement, vision potential, and available institutional resources (Table 1). Standardization of therapy remains controversial due to the evolving nature of treatment and lack of prospective studies or randomized trials. Even in the United States, enucleation remains the definitive treatment in cases of advanced unilateral intraocular retinoblastoma (group E) (Figure 1). Long-term burden of treatment such as need for multiple EUAs (32 or more), ocular toxicity, and unpredictable visual outcome should also be considered when discussing treatment options with the parents and the pediatric oncologist.
| ROUTE | INVOLVED COMPARTMENT | MAIN LIMITATION(S) | |||
| Retinal tumor | Choroidal extension | Vitreous seeding | Subretinal seeding | ||
| Intravenous chemotherapy | Effective | Effective | Minimally effective | Moderately effective | Systemic toxicity |
| Intra-arterial chemotherapy | Effective | Effective | Moderately effective | Effective | Technically challenging, affordability, local toxicity |
| Intravitreal chemotherapy | Minimally effective | Minimally effective | Highly effective | Minimally effective | Potential for extraocular seeding |
| Limited effectiveness of intra-arterial chemotherapy and intravenous chemotherapy on vitreous seeding can be overcome by combining them with intravitreal chemotherapy. | |||||
FOCAL THERAPY OPTIONS
Focal consolidation therapy performed along with intravenous chemotherapy (IVC) or intra-arterial chemotherapy (IAC) include cryotherapy, transpupillary thermotherapy, and plaque brachytherapy. Cryotherapy is effective for small equatorial and peripheral retinal tumors (group A). Triple freeze thaw cryotherapy is applied at 4-6 weeks intervals until complete tumor regression. Transpupillary thermotherapy is indicated for posteriorly located small tumors (group B). The therapy is delivered using an 810 nm diode laser with a longer treatment duration covering the entire extent of the tumor. Complete tumor regression can be achieved in more than 85% of tumors using 3 to 4 sessions of thermotherapy. The contributory effect of focal therapies applied prior to, during, or after completion of chemotherapy is an important confounding variable that is often overlooked when interpreting published data.5 External beam radiation therapy is avoided, if possible, given the associated side effects and risk of developing secondary cancers later in life. However, focal radiation such as plaque brachytherapy has been used successfully in children with RB.6
CHEMOTHERAPY OPTIONS
Globe salvaging treatment modalities include systemic chemotherapy delivered either intravenously or intra-arterially, along with local delivery of chemotherapy drug into the intravitreal cavity (iVitC). A simplified guide to choosing treatment options currently used at our center is provided (Table 2).
| GROUP | TREATMENT METHOD | COMMENTS | |||
| Focal therapy | IVC | IAC | IvitC | ||
| A | Yes | No | No | No | Cryotherapy and TTT based on location |
| B | Yes | Maybe | No | No | May benefit from chemoreduction |
| C | Yes | Preferred | Alternative | Yes | IVC and IAC are equally effective |
| D | Yes | Alternative | Preferred | Yes | IAC is more effective than IVC* |
| E | Yes | Alternative | Preferred | Yes | IAC is more effective than IVC |
| IAC, intra-arterial chemotherapy; IVC, intravitreal chemotherapy; IvitC, intravitreal chemotherapy; TTT, transpupillary thermotherapy.Focal therapy is used in all groups of RB. Group A: Can be managed by focal therapy alone. Groups D, E: if no potential for vision, consider enucleation. *The Children’s Oncology Group is currently conducting a prospective study to evaluate IVC plus iVitC for group D eyes. |
|||||
Intravenous Chemotherapy
Intravenous chemotherapy involves delivering 6 cycles of chemotherapy (carboplatin, vincristine, and etoposide) through a systemic route to shrink or reduce the tumor size (chemoreduction) followed by focal consolidative therapy. Intravenous chemotherapy is one of the main globe-salvaging options for RB groups B and C, with excellent outcomes in salvaging group B and C eyes (100%).7 However, the globe salvage for group D and group E eyes is modest (24% to 59%).7,8 Systemic side effects include myelosuppression, immunosuppression, risk of serious bacterial infection, and nonspecific gastrointestinal toxicity. Carboplatin is associated with risk of ototoxicity and nephrotoxicity; however, these are quite rare and studies show they are dose dependent.9 Etoposide can increase secondary malignancy risk to 4% in patients with germline Rb1 alteration,10 and it can alter bone metabolism.11 Although acute toxicities can occur, systemic IVC is given in the outpatient clinic and is generally well tolerated with minimal risk of late effects.
Intra-arterial Chemotherapy
With the aim to avoid systemic toxicity with IVC and to achieve higher globe salvage rates, there has been a shift toward use of IAC.12 The drug delivered is targeted to the globe by passing the catheter into the ostium of the ophthalmic artery via femoral arterial catheterization. The most commonly used agents include melphalan, topotecan, and carboplatin. The standard regimen includes delivery of 1 or a combination of 2 drugs, given once monthly for 3 cycles. In a systematic review of published studies, the overall globe salvage rate was 74% with IAC as a first-line treatment modality.13 Specifically, for group D (36% to 100%) and group E (17% to 87%), the results with IAC are more favorable compared with IVC.14-16 The Children’s Oncology Group is currently conducting a prospective study to evaluate IVC plus iVitC for group D eyes. Systemic toxicity of IVC is substituted by IAC procedure-related ocular complications, such as bradycardia and/or hypotension, ophthalmic artery stenosis and occlusion, retinal artery or vein occlusion, and intraocular hemorrhage.
Intravitreal Chemotherapy
Tumor seeding is one of the major predictive factors for failure of both IVC and IAC.17,18 Intravitreal chemotherapy (iVitC) is a targeted approach that delivers the highest concentration of drug into the vitreous cavity without systemic toxicity.19 By definition, group C, D, and E eyes are associated with vitreous seeding, and in such eyes, complete regression of vitreous seeds can be achieved in 82% to 100% of eyes (iVitC, melphalan).20 The most used drugs are melphalan and topotecan given once monthly until complete resolution or calcification of vitreous seeds is noted. The most common and expected toxicity is a localized salt-and-pepper retinopathy, particularly due to melphalan toxicity due to its high binding with retinal pigment epithelium (RPE).21 This is more commonly seen in children with brown eyes due to increased pigmentation within the iris as well as in RPE. Topotecan is an effective alternative.22 Extensive data since 2012 has dissipated the fear of extraocular extension or needle tract seeding, provided that certain safety rules for injections are followed.20
EMERGING TREATMENT OPTIONS
Intracameral Chemotherapy
Encouraged by results following (iVitC), intracameral chemotherapy for aqueous seeding has been developed for a rare case of recurrent RB that presents as white fluffy seeds in the anterior chamber usually secondary to tumor extension into the ciliary body. Early results from a single center have been promising, with eye preservation achieved in 85% (mean follow-up of 45 months).23
Oncolytic Adenovirus (VCN-01)
A novel oncolytic adenovirus is designed to replicate selectively in tumor cells with high abundance of free E2F1, a consequence of a dysfunctional RB1 pathway. In mice with RB xenografts, intravitreal administration of VCN-01 induced tumor necrosis, improved ocular survival, and prevented micrometastatic dissemination into the brain, despite considerable intraocular inflammation.24 The first clinical trial currently ongoing at SJD Barcelona Children’s Hospital in Spain aims to study the safety and efficacy of the treatment, particularly in chemoresistant RB cases. The preliminary results of the study were promising in terms of tumor regression and globe salvage.25
Chemoplaque
A phase 1 study is currently under way to evaluate a novel sustained-release episcleral plaque loaded with topotecan, called chemoplaque, in patients with active residual or recurrent intraocular retinoblastoma in at least 1 eye following completion of first-line therapy.26
Belinostat
Advances in the understanding of the molecular drivers of RB pathway have provided opportunities to explore novel drugs with targeted effects, improved bioavailability, and reduced chemotoxicity. In preclinical studies, molecularly targeted inhibition of HDACs with intravitreal belinostat seems to be effective but without retinal toxicity.27
CONCLUSION
Considering global burden of retinoblastoma with predominance in lower-income and middle-income countries, innovative approaches in drug delivery and alternatives to chemotherapy that are inexpensive and accessible are needed. RP
REFERENCES
- Murphree AL, Benedict WF. Retinoblastoma: clues to human oncogenesis. Science. 1984;223(4640):1028-1033. doi:10.1126/science.6320372
- Usmanov RH, Kivelä T. Predicted trends in the incidence of retinoblastoma in the Asia-Pacific region [published correction appears in Asia Pac J Ophthalmol (Phila). 2014 Nov-Dec;3(6):397]. Asia Pac J Ophthalmol (Phila). 2014;3(3):151-157. doi:10.1097/APO.0000000000000060
- Abramson DH, Beaverson K, Sangani P, et al. Screening for retinoblastoma: presenting signs as prognosticators of patient and ocular survival. Pediatrics. 2003;112(6 Pt 1):1248-1255. doi:10.1542/peds.112.6.1248
- Shields CL, Mashayekhi A, Au AK, et al. The International Classification of Retinoblastoma predicts chemoreduction success. Ophthalmology. 2006;113(12):2276-2280. doi:10.1016/j.ophtha.2006.06.018
- Raval V, Bowen RC, Soto H, Singh A. Chemotherapy for retinoblastoma: impact of intravitreal chemotherapy. Asia Pac J Ophthalmol (Phila). 2020;10(2):200-202. Published 2020 Sep 9. doi:10.1097/APO.0000000000000322
- Echegaray JJ, Al-Zahrani YA, Singh A. Episcleral brachytherapy for retinoblastoma. Br J Ophthalmol. 2020;104(2):208-213. doi:10.1136/bjophthalmol-2019-313985
- Chung CY, Medina CA, Aziz HA, Singh AD. Retinoblastoma: evidence for stage-based chemotherapy. Int Ophthalmol Clin. 2015;55(1):63-75. doi:10.1097/IIO.0000000000000054
- Raval V, Bowen RC, Soto H, Singh A. Intravenous chemotherapy for retinoblastoma in the era of intravitreal chemotherapy: a systematic review. Ocul Oncol Pathol. 2021;7(2):142-148. doi:10.1159/000510506
- Lambert MP, Shields C, Meadows AT. A retrospective review of hearing in children with retinoblastoma treated with carboplatin-based chemotherapy. Pediatr Blood Cancer. 2008;50(2):223-226. doi:10.1002/pbc.21155
- Turaka K, Shields CL, Meadows AT, Leahey A. Second malignant neoplasms following chemoreduction with carboplatin, etoposide, and vincristine in 245 patients with intraocular retinoblastoma. Pediatr Blood Cancer. 2012;59(1):121-125. doi:10.1002/pbc.23278
- Schündeln MM, Hauffa PK, Bauer JJ, et al. Pediatric survivors of retinoblastoma are at risk for altered bone metabolism after chemotherapy treatment early in life. Pediatr Hematol Oncol. 2015;32(7):455-466. doi:10.3109/08880018.2015.1048912
- Abramson DH, Dunkel IJ, Brodie SE, Kim JW, Gobin YP. A phase I/II study of direct intraarterial (ophthalmic artery) chemotherapy with melphalan for intraocular retinoblastoma initial results. Ophthalmology. 2008;115(8):1398-1404.e1. doi:10.1016/j.ophtha.2007.12.014
- Yousef YA, Soliman SE, Astudillo PPP, et al. Intra-arterial chemotherapy for retinoblastoma: a systematic review. JAMA Ophthalmol. 2016;134(5):584-591. doi:10.1001/jamaophthalmol.2016.0244
- Suzuki S, Yamane T, Mohri M, Kaneko A. Selective ophthalmic arterial injection therapy for intraocular retinoblastoma: the long-term prognosis. Ophthalmology. 2011;118(10):2081-2087. doi:10.1016/j.ophtha.2011.03.013
- Abramson DH, Marr BP, Brodie SE, Dunkel I, Palioura S, Gobin YP. Ophthalmic artery chemosurgery for less advanced intraocular retinoblastoma: five year review. PLoS One. 2012;7(4):e34120. doi:10.1371/journal.pone.0034120
- Manjandavida FP, Stathopoulos C, Zhang J, Honavar SG, Shields CL. Intra-arterial chemotherapy in retinoblastoma - a paradigm change [published correction appears in Indian J Ophthalmol. 2019 Aug;67(8):1385]. Indian J Ophthalmol. 2019;67(6):740-754. doi:10.4103/ijo.IJO_866_19
- Shields CL, Honavar SG, Meadows AT, et al. Chemoreduction plus focal therapy for retinoblastoma: factors predictive of need for treatment with external beam radiotherapy or enucleation. Am J Ophthalmol. 2002;133(5):657-664. doi:10.1016/s0002-9394(02)01348-x
- Francis JH, Iyer S, Gobin YP, Brodie SE, Abramson DH. Retinoblastoma vitreous seed clouds (class 3): a comparison of treatment with ophthalmic artery chemosurgery with or without intravitreous and periocular chemotherapy. Ophthalmology. 2017;124(10):1548-1555. doi:10.1016/j.ophtha.2017.04.010
- Munier FL, Soliman S, Moulin AP, Gaillard MC, Balmer A, Beck-Popovic M. Profiling safety of intravitreal injections for retinoblastoma using an anti-reflux procedure and sterilisation of the needle track. Br J Ophthalmol. 2012;96(8):1084-1087. doi:10.1136/bjophthalmol-2011-301016
- Munier FL, Gaillard MC, Balmer A, et al. Intravitreal chemotherapy for vitreous disease in retinoblastoma revisited: from prohibition to conditional indications. Br J Ophthalmol. 2012;96(8):1078-1083. doi:10.1136/bjophthalmol-2011-301450
- Francis JH, Schaiquevich P, Buitrago E, et al. Local and systemic toxicity of intravitreal melphalan for vitreous seeding in retinoblastoma: a preclinical and clinical study. Ophthalmology. 2014;121(9):1810-1817. doi:10.1016/j.ophtha.2014.03.028
- Buitrago E, Höcht C, Chantada G, et al. Pharmacokinetic analysis of topotecan after intra-vitreal injection. Implications for retinoblastoma treatment. Exp Eye Res. 2010;91(1):9-14. doi:10.1016/j.exer.2010.03.009
- Stathopoulos C, Beck-Popovic M, Moulin AP, Munier FL. Ten-year experience with intracameral chemotherapy for aqueous seeding in retinoblastoma: long-term efficacy, safety and toxicity. Br J Ophthalmol. 2022;bjo-2022-322492. doi:10.1136/bjo-2022-322492
- Pascual-Pasto G, Bazan-Peregrino M, Olaciregui NG, et al. Therapeutic targeting of the RB1 pathway in retinoblastoma with the oncolytic adenovirus VCN-01. Sci Transl Med. 2019;11(476):eaat9321. doi:10.1126/scitranslmed.aat9321
- “Thanks to this clinical trial to combat retinoblastoma, Félix is able to carry on enjoying life.” Hospital Sant Joan de Déu Barcelona. November 27, 2020. Accessed May 10, 2023. https://www.sjdhospitalbarcelona.org/en/thanks-clinical-trial-combat-retinoblastoma-felix-able-carry-enjoying-life
- Topotecan episcleral plaque for treatment of retinoblastoma (STEP-RB). Clinicaltrials.gov identifier: NCT04428879. Updated May 20, 2021. Accessed May 10, 2023. https://clinicaltrials.gov/ct2/show/NCT04428879
- Kaczmarek JV, Bogan CM, Pierce JM, et al. Intravitreal HDAC inhibitor belinostat effectively eradicates vitreous seeds without retinal toxicity in vivo in a rabbit retinoblastoma model. Invest Ophthalmol Vis Sci. 2021;62(14):8. doi:10.1167/iovs.62.14.8








