Infectious retinitis is a diagnosis with the potential to cause profound vision loss. While it may occur in both pediatric and adult populations, the scope of this article will focus on the role of multimodal imaging in the characterization and diagnosis of infectious retinitis in adults. Infectious retinitis can indicate an immunocompromised state or insidious systemic disease, prompting further evaluation, but can also occur in immunocompetent patients. It is important to properly diagnose this entity to avoid treatment delay, because patients usually require aggressive intervention once the pathogen is identified.
The most common causative viruses are cytomegalovirus (CMV), herpes simplex virus (HSV) type 1 and type 2, and varicella-zoster virus (VZV). The parasitic infection toxoplasmosis can cause both focal and widespread retinitis depending on the immune status of the host. Other infections include syphilis, endogenous bacterial or fungal infections, West Nile virus, tuberculosis, and other less common infections. This article will highlight the pathogens that cause characteristic findings on multimodal imaging that can be used to distinguish one etiology from another.
CYTOMEGALOVIRUS RETINITIS
Cytomegalovirus retinitis often indicates a systemic infection secondary to an immunocompromised state. The diagnosis is clinical, although polymerase chain reaction (PCR) testing of either the aqueous or the vitreous can be confirmatory. Although fulminant CMV retinitis is characterized by a classic “pizza-pie” appearance due to hemorrhagic necrosis, the more diagnostically challenging manifestation is the indolent form that presents with minimal hemorrhage and granular lesions in the peripheral retina.
Ultrawidefield imaging is helpful in highlighting subtle peripheral findings, as seen in Figure 1A. This patient was immunocompromised and presented with granular lesions that were difficult to visualize on exam, but are highlighted by the Optos ultrawidefield fundus camera. The Optos camera utilizes pseudocolor green (532 nm) and red (633 nm) filters that preferentially capture retinal and choroidal pathology, respectively. As this patient was treated with antivirals, the lesions pigmented over time and were effectively monitored using serial ultrawidefield retinal photos (Figures 1B and 1C).
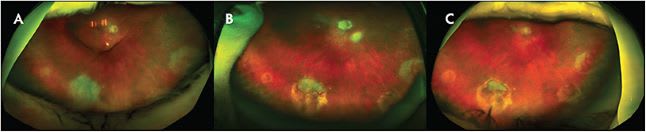
Optical coherence tomography (OCT) in CMV demonstrates disruption of the inner segment/outer segment junction, along with retinal thickening and midretinal hyperreflectivity.1 Management involves the use of oral or intravitreal antiviral medications and sometimes requires intravenous antiviral medications. A large percentage of patients develop a rhegmatogenous retinal detachment, cystoid macular edema, or an epiretinal membrane, all of which can be visually significant complications.2 Serial multimodal imaging can be helpful in monitoring these complications.
VARICELLA-ZOSER VIRUS AND HERPES SIMPLEX VIRUS TYPE 1 AND 2
Acute retinal necrosis (ARN) and progressive outer retinal necrosis (PORN) are caused by VZV and HSV types 1 and 2. Acute retinal necrosis is the term typically assigned to herpetic retinitis in immunocompetent patients, while PORN describes the subtle manifestations of herpetic retinitis in immunocompromised patients. The manifestations of both entities include retinal vasculitis with hemorrhages, white-yellow lesions, and retinal necrosis, with retinitis starting peripherally and extending into the posterior pole. The full-thickness retinal lesions rapidly coalesce and lead to widespread retinal necrosis.3 Patients present with decreased vision, floaters, and flashes, usually unilaterally.
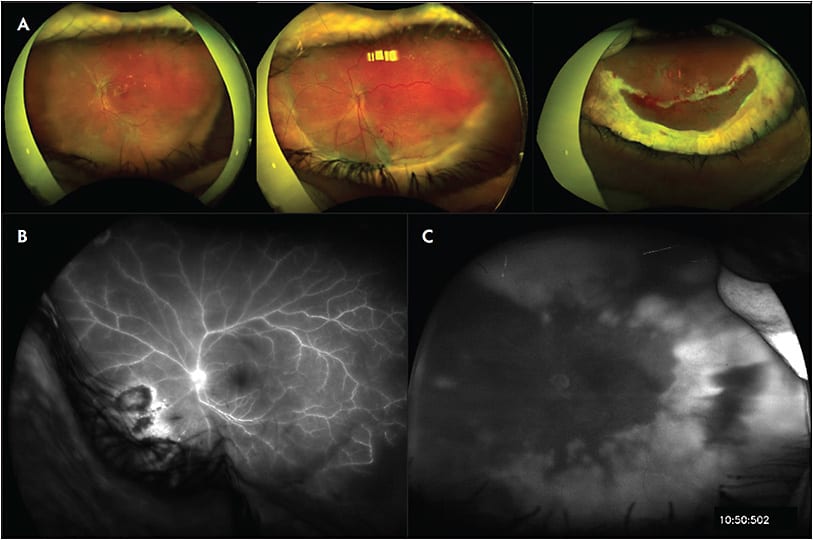
In immunocompetent individuals, the viral particles will cause a robust immune response leading to cicatricial structural changes in the retina and vitreous. Figure 2A demonstrates an example of retinitis secondary to VZV in an immunocompetent patient who ultimately developed cicatrizing disease and rhegmatogenous retinal detachment requiring extensive retinectomy, scleral buckling, and vitrectomy for repair.
TOXOPLASMOSIS
Ocular toxoplasmosis is caused by Toxoplasma gondii, an intracellular parasite, and is the most common cause of infectious retinitis.4 Clinical exam reveals the classic “headlight in fog” with a focal area of retinitis and overlying vitreous inflammation. A nearby chorioretinal scar represents a prior healed infection, and recurrences often occur at the margin of an old scar. Ocular toxoplasmosis is mostly a clinical diagnosis; however, PCR can be used for atypical causes. Optical coherence tomography can highlight the active phase of toxoplasmosis, including disruption of inner/outer retina, dense vitreous inflammation, choroidal neovascular membrane formation, and choroidal thickening posterior to retinitis.
Fluorescein angiography can demonstrate distinguishing characteristics in infectious retinitis. For example, Figures 2B and 2C compare images of fluorescein angiograms in toxoplasma chorioretinitis and herpetic retinitis. The most notable distinction is the hyperfluorescence of the retinal vasculature in toxoplasmosis as compared to herpetic retinitis. In immunocompromised patients, toxoplasmosis can appear flat and broad, and it can be difficult to distinguish clinically from herpetic retinitis, making fluorescein angiogram a useful adjunct for diagnosis.
OTHER INFECTIOUS RETINITIS
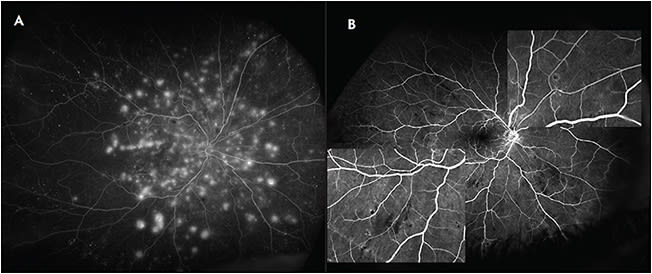
Other rarer forms of infectious retinitis, such as West Nile virus, can demonstrate characteristic findings on multimodal imaging to distinguish acute versus chronic disease. Figure 3 demonstrates acute-phase West Nile virus (Figure 3A), which is characterized by multifocal pinpoint areas of hyperfluorescence, as well as late-phase West Nile virus in a distinct patient (Figure 3B) which shows staining linear and target-like lesions on fluorescein angiography.5
CONCLUSION
Multimodal imaging is a useful adjunct to both the diagnosis and treatment of infectious retinitis. Initial presentation of infectious retinitis can be challenging due to subtle findings or overlap of presentation between etiologies depending on the immune status of the patient. Fundus photography, OCT, fluorescein angiography, and other angiographic imaging modalities can provide ancillary information to better inform the diagnosis, especially if PCR-based diagnosis of the intraocular fluid is delayed or unavailable.
Monitoring of infectious retinitis for improvement and resolution is crucial during treatment, and multimodal imaging can also prove useful for disease monitoring over time. This is especially true of ultrawidefield fundus photography using a nonmydriatic camera, which is able to circumvent media opacity and synechiae to reveal pathology in the periphery where the earliest and most subtle signs of infectious retinitis often occur. The use of imaging in addition to the clinical exam and aqueous or vitreous fluid testing can help guide management quickly, which is crucial given the vision-threatening nature of infectious retinitis. RP
REFERENCES
- Mahendradas P, Sridharan A, Kawali A, Sanjay S, Venkatesh R. Role of ocular imaging in diagnosis and determining response to therapeutic interventions in posterior and panuveitis. Asia Pac J Ophthalmol (Phila). 2021;10(1):74-86. doi:10.1097/APO.0000000000000354
- Banker AS. Posterior segment manifestations of human immunodeficiency virus/acquired immune deficiency syndrome. Indian J Ophthalmol. 2008;56(5):377-383. doi:10.4103/0301-4738.42413
- Holland GN. The progressive outer retinal necrosis syndrome. Int Ophthalmol. 1994;18(3):163-165. doi:10.1007/BF00915966
- Kim SJ, Scott IU, Brown GC, et al. Interventions for toxoplasma retinochoroiditis: a report by the American Academy of Ophthalmology. Ophthalmology. 2013;120(2):371-378. doi:10.1016/j.ophtha.2012.07.061
- Golshani C, Venkat A, Srivastava SK. Multimodal imaging findings in acute West Nile virus chorioretinitis [published online ahead of print, 2021 May 12]. Retin Cases Brief Rep. 2021;10.1097/ICB.0000000000001162. doi:10.1097/ICB.0000000000001162








