Over the last 15 years, the incidence of severe vision loss from neovascular age-related macular degeneration (nAMD) has fallen markedly, owing to the introduction of treatment with intravitreal anti-VEGF therapy. However, the real-world outcomes of treatment consistently fail to produce the gains in function achieved by the landmark studies. In the real world, the tight controls of clinical studies are often not followed, and capacity constraints may lead to less-than-optimal treatment protocols. In the context of suboptimal management, there is considerable potential for reactivation of the neovascular lesion, resulting in fluctuations in retinal thickness, which is a key biomarker of loss of control of fluid. This clearly begs the question of the effect of such fluctuations on functional and morphologic outcomes during anti-VEGF therapy.
DOSING PROTOCOLS
The pivotal trials that heralded the age of anti-VEGF therapy followed a dosing protocol that was developed based on prior knowledge of drug durability and treatment efficacy where treatments were given at prespecified fixed intervals. The trials that used this treatment posology have to date yielded the best possible visual outcomes. Nonetheless, for several reasons, such as constraints of capacity and funding issues, centers often follow a pro re nata (PRN) strategy, which involves retreatment only when retinal fluid is detected; this approach relies on the detection of morphological changes to trigger further treatment. Subsequently, a compromise protocol was developed that had elements of both the fixed dosing and PRN approaches, which was termed treat-and-extend. In this situation, a treatment is administered at every visit regardless of activity. If the retina is dry or the morphology remains stable, then the treatment interval is extended; if there is an increase in fluid or drop in visual acuity then the interval between treatments is reduced. Although this approach does allow optimization of the capacity of such clinics, it still allows for a certain level of fluctuation in retinal fluid.
Although it is established that persistent lesion activity is a poor prognostic marker for best-corrected visual acuity (BCVA), recent evidence also suggests that fluid location and the cycle of fluid fluctuations can impact outcomes. Continuous-release devices and other longer acting treatments may have the potential to stabilize the retina more effectively.
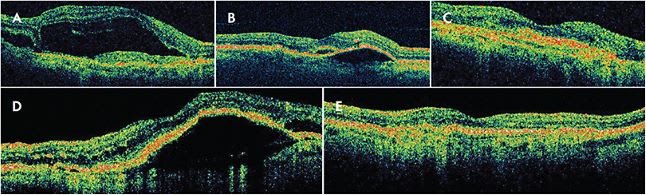
SUBRETINAL FLUID VS INTRARETINAL FLUID
Exploring the impact of retinal thickness fluctuations on outcomes begins with a definition of retinal fluid. There are 2 distinct compartments that have emerged as important in the management of nAMD: subretinal fluid (SRF) and intraretinal fluid (IRF). Over the last few years there have been myriad studies looking at the difference in outcomes dependent on fluid compartment. When analyzed, results from the Comparison of Age-Related Macular Degeneration Treatments Trials (CATT) had better BCVA outcomes in eyes that had SRF,1 and the Inhibition of VEGF in Age-Related Choroidal Neovascularization (IVAN) trial showed less geographic atrophy in eyes that displayed SRF.2 Furthermore, the FLUID study looked specifically at the impact of SRF on vision outcomes in patients being treated with ranibizumab (Lucentis; Genentech) and it was found that tolerating SRF of less than 200 µm had comparable BCVA outcomes but required fewer injections to achieve it.3
The first study to examine the impact of retinal thickness fluctuations on functional and morphologic outcomes was the pooled analysis from CATT and IVAN. Both of these trials, which were contemporaneous and used similar treatment regimens and drugs, reported the results from the 1,731 patients who were enrolled in these studies. Study eyes that exhibited the greatest fluctuations in fluid (measured as foveal center point thickness [FCPT]) had the lowest BCVA gains. This analysis also found that those with the greatest FCPT variations also showed a greater development of fibrosis.1 The FCPT measurements in these 2 trials were taken using time-domain optical coherence tomography; subsequently, other studies confirmed these findings based on measurements made using spectral-domain instruments.
The HARBOR trial investigated fixed dosing (monthly) vs PRN treatment of ranibizumab (0.5 mg or 2 mg) in 1,097 subjects with nAMD and was also subjected to secondary analysis. The results showed that the PRN regime was not inferior to fixed dosing. Using this data set, Sheth et al4 carried out an in-depth post hoc analysis looking at the impact on outcomes that fluid fluctuations had across the groups. The 1,097 patients were pooled and redistributed into quartiles dependent on their fluid fluctuation score. The fluctuation score was calculated by cumulative change in the central foveal thickness (internal limiting membrane to the retinal pigment epithelium). Each time a central retinal thickness fluctuation of greater than 50 μm in either direction was measured, the numerical value was added to the fluctuation score. Moving across the quartiles (1 being the lowest fluctuation value and 4 being the highest) it was found that there was an inverse correlation with BCVA gains and fluctuation scores.
Further subanalysis of the HARBOR trial results considered SRF vs IRF fluid compartments. When the SRF compartment only was considered in the fluctuation score, there was no statistical significance in BCVA gains across the quartiles. However, IRF (measured from internal limiting membrane to photoreceptor outer segments) fluctuations again showed an inverse correlation in BCVA gains across the quartiles. When the treatment arms were compared, there was a greater number of patients in the PRN group compared to the monthly treatment arm in quartile 4 (179 vs 33); however, between these 2 groups in quartile 4 there was little difference in outcomes suggesting that the fluctuation in fluid was an influencing factor.4
Sadda et al5 also carried out a post hoc analysis on the HARBOR data set and fluid dynamics. This study did not look at fluctuations; instead, it examined the presence of IRF or SRF at baseline, 12 months, and 24 months, and determined whether the fluid was central or noncentral. Analysis showed a poorer visual outcome with residual IRF, regardless of severity or location. Residual SRF did not demonstrate a poorer outcome.
The HAWK and HARRIER trials, which examined the comparative effectiveness of brolucizumab (Beovu; Novartis) to aflibercept (Eylea; Regeneron) in the treatment of new-onset nAMD was also subjected to a post hoc analysis.6 Employing a treatment-agnostic approach, study eyes were assigned to 4 groups based on the severity of central subfield thickness (CST) fluctuations over the entire follow-up period in the 1,752 subjects. Analysis showed that those with the least fluctuations in CST demonstrated the greatest gains in BCVA. Furthermore, it was shown that greater CST fluctuations were associated with fluid persistence in the maintenance phase.6
In addition to post hoc analysis of clinical trials, a real-world study was carried out by Chakravarthy et al,7 who analyzed results from a single UK site constituting 403 eyes with complete data and a further 399 eyes with limited data. Artificial intelligence was used to obtain volume measurements of IRF, SRF, and pigment epithelium detachment. As in the landmark trials, there was a negative correlation with BCVA gains and retinal fluid fluctuations. When fluid compartmentalization was considered, IRF fluctuation had the greatest impact, PED medium impact, and SRF variability the least.
In an analysis of outcomes from the ARCHWAY study8 presented at the American Society of Retina Specialists Annual Meeting 2022, the Roche/Genentech Susvimo sustained-release implant was compared to monthly ranibizumab and showed that most eyes in both arms showed no fluctuations. In this study, the Susvimo arm demonstrated the potential to achieve real-world outcomes similar to those found in clinical trials without the need for frequent injections. Susvimo was voluntarily recalled in October 2022.
NONEXUDATIVE FLUID
When treating nAMD, it is important to determine whether fluid as a marker for activity is exudative in nature. As the nomenclature of AMD develops,9 the terms exudative, nonexudative, and non-neovascular are becoming more widely applicable. Optical coherence tomography angiography has revealed that nonexudative macular neovascularization is more commonly encountered than previously thought. However high-quality imaging also demonstrates that fluid in AMD may not always be neovascular in origin. Cuffs of fluid seen at the edges of a pigment epithelium detachment may not be from exudation, but instead arise from the tenting of the overlying retina as it is stretched by the pigment epithelium detachment. As the macula becomes atrophic, it is also not uncommon to see chronic areas that resemble cystic change but that, in fact, represent a loss of retinal tissue in a degenerative manner rather than cystic exudation.
CONCLUSION
The growing body of evidence suggests that better control of retinal fluid and minimizing retinal thickness fluctuations of nAMD allows retina specialists to optimize visual outcomes when treating patients with intravitreal anti-VEGF. While treatment regimen is an important factor in outcomes, stabilization of the retinal anatomy and minimizing fluctuations in central retinal thickness should be of high priority. There are multiple post hoc analyses indicating that the presence of SRF may not be a significant biomarker for poor visual outcomes3 and that fluctuations in this fluid compartment may not have a negative impact on BCVA. The evidence suggests that the converse may be true with IRF: fluctuations correlate to worse outcomes. Further real-world studies would lend greater significance to this complex relationship. Additionally, in managing nAMD, it is important to ensure the fluid being treated is truly exudative in nature. RP
REFERENCES
- Evans RN, Reeves BC, Maguire MG, et al. Associations of variation in retinal thickness with visual acuity and anatomic outcomes in eyes with neovascular age-related macular degeneration lesions treated with anti-vascular endothelial growth factor agents. JAMA Ophthalmol. 2020;138(10):1043-1051. doi:10.1001/jamaophthalmol.2020.3001
- Bailey C, Scott LJ, Rogers CA, et al. Intralesional macular atrophy in anti–vascular endothelial growth factor therapy for age-related macular degeneration in the IVAN trial. Ophthalmology. 2019;126(1):75-86. doi:10.1016/j.ophtha.2018.07.013
- Guymer RH, Markey CM, McAllister IL, et al. Tolerating subretinal fluid in neovascular age-related macular degeneration treated with ranibizumab using a treat-and-extend regimen: FLUID study 24-month results. Ophthalmology. 2019;126(5):723-734. doi:10.1016/j.ophtha.2018.11.025
- Sheth V, D’Rozario M, Gune S, Blotner S. Fluctuations in central foveal thickness and association with vision outcomes with anti-VEGF therapy for nAMD: HARBOR post hoc analysis. BMJ Open Ophthalmol. 2022;7(1). doi:10.1136/bmjophth-2021-000957
- Sadda S, Holekamp NM, Sarraf D, et al. Relationship between retinal fluid characteristics and vision in neovascular age-related macular degeneration: HARBOR post hoc analysis. Graefes Arch Clin Exp Ophthalmol. 2022;260(12):3781-3789. doi:10.1007/s00417-022-05716-4
- Dugel PU, Jhaveri CD, Chakravarthy U, et al. Effect of retinal thickness variability on visual outcomes and fluid persistence in neovascular age-related macular degeneration: a post hoc analysis of the HAWK and HARRIER studies. Retina. 2022;42(3):511-518. doi:10.1097/IAE.0000000000003349
- Chakravarthy U, Havilio M, Syntosi A, et al. Impact of macular fluid volume fluctuations on visual acuity during anti-VEGF therapy in eyes with nAMD. Eye (Basingstoke). 2021;35(11):2983-2990. doi:10.1038/s41433-020-01354-4
- Holekamp NM, Campochiaro PA, Chang MA, et al. Archway randomized phase 3 trial of the Port Delivery System with ranibizumab for neovascular age-related macular degeneration. Ophthalmology. 2022;129(3):295-307. doi:10.1016/j.ophtha.2021.09.016
- Sharma A, Parachuri N, Kumar N, et al. Terms non-exudative and non-neovascular: awaiting entry at the doors of AMD reclassification. Graefes Arch Clin Exp Ophthalmol. 2021;259(6):1381-1383. doi:10.1007/s00417-021-05164-6








