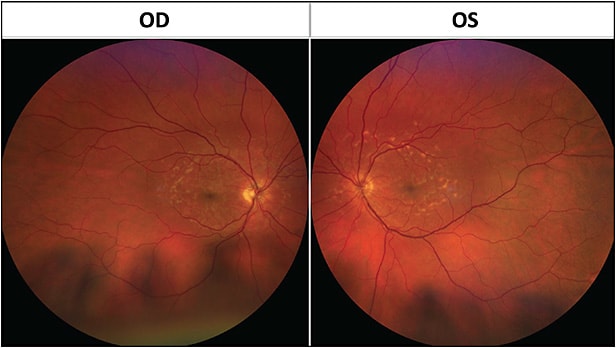
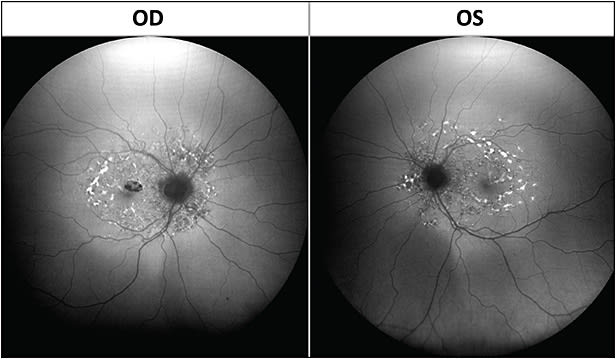
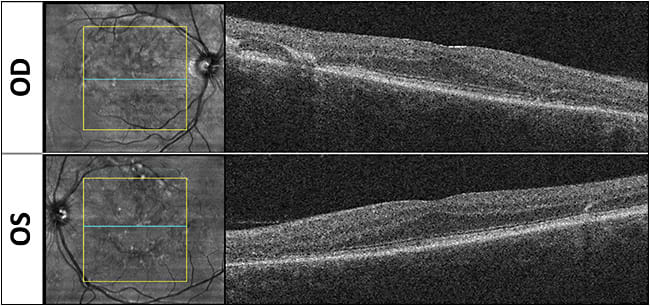
In a recent Retinal Physician Imaging Challenge livestream discussion, I presented a case of a 53-year-old male referred by an outside provider for maculopathy evaluation. Although he denied any family history of vision loss, he endorsed slow decline in vision over years. On examination, his visual acuity (VA) was 20/50 in the right eye and 20/40 in the left, and he had normal intraocular pressures. Anterior-segment examination was significant for a 1+ nuclear sclerosis cataract but otherwise was unremarkable. On dilated examination (Figure 1), we detected scattered yellow-whitish pisciform fundus flecks throughout the posterior pole bilaterally. On fundus autofluorescence (Figure 2), we captured these flecks, which were a mix of hyperautofluoresence (corresponding to increased lipofuscin accumulation) and hypoautofluorescence (atrophy and photoreceptor loss). On optical coherence tomography (Figure 3), some of the flecks could be noted, but there was no intraretinal or subretinal fluid noted. There was also no choroidal neovascularization detected.
Based on our physical examination and the elicited history, we suspected the patient had Stargardt disease. This is a rare disease affecting 1 in 10,000 individuals, caused by mutations in the ABCA4 gene1 through autosomal recessive homozygous or compound heterozygous transmission. Phenotypic presentation of the disease is variable2 (VA can range from 20/20 to 20/400) correlating with the expressed levels of ABCA4. Age of onset of the visual symptoms is also highly variable. The disease arises as AE2 accumulates as lipofuscin3 in the retinal pigment epithelium (RPE) leading to poor function of the epithelium, which subsequently leads to retinal damage.
Stargardt disease remains an incurable condition, but as new trials are under way for inherited retinal disorders, the first step for these patients is in getting a definitive diagnosis. We obtained genetic testing for this patient using Blueprint Genetics and confirmed that he indeed was compound heterozygous for Stargardt disease.
Patients with Stargardt disease should be advised to avoid UV light exposure and to avoid smoking. Given that there are multiple clinical trials that are currently enrolling patients with his condition, we referred him to the Center for Inherited Retinal Disorders in Boston and will follow him yearly. RP

Editor’s note: Follow Retinal Physician on YouTube, Facebook, Linkedin, and Twitter to guess the diagnosis for the next imaging challenge and to catch future livestreamed case discussions with Dr. Mari Rodriguez.
REFERENCES
- Allikmets R, Singh N, Sun H, et al. A photoreceptor cell-specific ATP-binding transporter gene (ABCR) is mutated in recessive Stargardt macular dystrophy [published correction appears in Nat Genet. 1997 Sep;17(1):122]. Nat Genet. 1997;15(3):236-246. doi:10.1038/ng0397-236
- Westeneng-van Haaften SC, Boon CJ, Cremers FP, Hoefsloot LH, den Hollander AI, Hoyng CB. Clinical and genetic characteristics of late-onset Stargardt’s disease. Ophthalmology. 2012;119(6):1199-1210. doi:10.1016/j.ophtha.2012.01.005
- Molday RS, Zhang K. Defective lipid transport and biosynthesis in recessive and dominant Stargardt macular degeneration. Prog Lipid Res. 2010;49(4):476-492. doi:10.1016/j.plipres.2010.07.002.








