Posterior vitreous detachment (PVD), vitreous hemorrhage, or degenerative changes of the vitreous are some of the more common causes of symptomatic floaters in patients. Although these patients complain of subjective visual disturbances, it is difficult to clinically appreciate the impact of floaters using Snellen acuity alone, because most cases of floaters do not have substantially reduced visual acuity. Most often, these opacities are monitored by clinical biomicroscopic exam, examination with an indirect ophthalmoscope, or in some cases B-scan ultrasonography. Ultrasound based quantification of vitreous opacities (VO) has been previously reported1 but getting an ultrasound on every patient who complains of floaters in a busy retina clinic can be cumbersome.
Contrast sensitivity has also been reported to be decreased in patients with symptomatic VO, and to normalize with surgery,2 but such testing is also difficult to obtain in the setting of a busy clinic. Formal reading speed testing also showed improvement following surgery for VO, but also is somewhat time consuming.3 In this study, video SLO was carried out, and documented resolution of shadowing from VO following surgery. Currently in any retina clinic any spectral domain optical coherence tomography (SD-OCT) studies are easily acquired. Most OCT machines utilize a combination of confocal scanning laser ophthalmoscope (c-SLO) and SD-OCT to generate an image. With this technology the infrared image generated by the c-SLO can show shadows from the VO projected on the surface of the retina. During the collection of an OCT, the SLO screen is viewed live, often showing the VO, either stationary or in motion.4
The Heidelberg Spectralis device uses an 870 nm laser as the light source for OCT, which generates 40,000 scans per second with an axial resolution of 7 µm. The wavelength of the c-SLO laser is 820 nm (near-infrared), and operates also at 40,000 A-scans per second. The near-infrared fundus image is generated in a raster pattern that is 30° x 30° in the standard format, and the entire image is refreshed 9 times per second. This refresh rate is significantly slower than that of cinema, which is 24 frames per second, but it still allows for movie-like evaluation of movement of the VO.
By having the patient perform a saccade followed by refixation, the vitreous gel is set in motion and the shadowing and movement of the VO is easily visualized. The scan protocol utilized in our clinic has the patient perform a saccade followed by 3 seconds of refixation. The saccades are performed twice to the left, twice to the right, once up, then once down. The whole process of recording the images takes less than a minute. This can be performed using a 55° or a 30° lens. The 30° capture provides for a clearer image with better resolution, smaller file size, and reduced artifacts, whereas the 55° capture provides a larger field capturing more opacities. However, this creates a slightly larger file, poorer resolution, and artifacts on some older models of Heidelberg OCT. While the 30° capture shows obscuration of the macula very well, we have found the 55° lens to be slightly more useful, because the larger area captured demonstrates the broader areas of shadows that the patients find disturbing.
Below are a few examples of the utilization of these techniques to capture the impact of floaters.
Case 1: A 54-year-old male had 20/20 vision, but he had prominent central VO in both eyes that interfered with his career as a truck driver. The initial images were recorded with an iPhone, because Heidelberg had not yet added the feature allowing recording with the imaging device. A video of the right eye (Video 1) shows an opacity that blocks out most of the light transmission when situated over the macula. The postoperative video (Video 2) shows absence of any shadowing, and the patient had complete relief of symptoms after surgery.
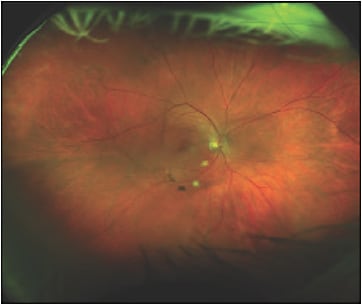
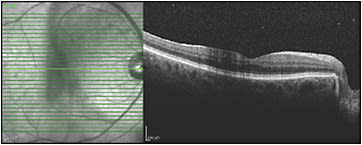
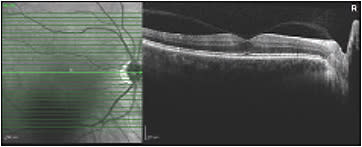
Case 2: A patient complains of significant “amoeba-like” vitreous floaters. On examination (Figure 1) some vitreous floaters are visible, but we are unable to assess the true impact of these floaters. Optical coherence tomography shows attenuation caused by the vitreous veil on the central macula (Figure 2). However, the 55° SLO video shows significant shadowing movement in an “amoeba-like” pattern over the central macula from these opacities (Video 3).
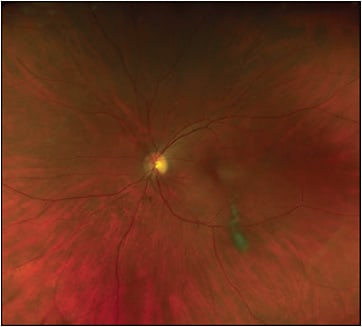
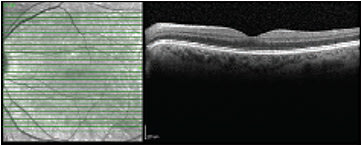
Case 3: A 64-year-old female with minimal cataract has been complaining of a prominent floater in the left eye for 2 years. This caused her difficulty with reading and driving despite her 20/20 measured acuity. She already had a posterior vitreous detachment and stated that the floater “never seems to move out of the way” (Figure 3). Video SLO confirmed this, as it is often the case that patient descriptions of their floaters exactly match video SLO findings (Video 4). She was offered surgery, which she underwent, and she was happy with the outcome. Follow-up SLO imaging shows absence of any shadowing (Figure 4).
Case 4: A 58-year-old male mechanic had undergone scleral buckling 6 months prior for a macula-on retinal detachment and had successful surgery. At 6 months he remained 20/20, had a visually insignificant epiretinal membrane, and had great difficulty reading because of his central vitreous floaters. Thirty-degree video SLO testing (Video 5) shows the floaters briefly moving with a saccade but returning promptly post-saccade to the central position that impaired reading. Fifty-five-degree video SLO imaging (Video 6) shows shadowing well outside the central macula. He was part of a study evaluating reading speed changes after vitrectomy for VO and had a very large improvement in reading speed after surgery. Figure 5 shows postoperative SLO.

Case 5: A 55-year-old male with clear lenses and moderate myopia was seen in 2016 complaining of very symptomatic central floaters in each eye. Both eyes had prominent opacities, but neither eye had yet developed a vitreous detachment (Figure 6). Video SLO of the right eye (Video 7) shows significant shadowing of the macula post saccade. Because he was functional (though unhappy with his symptoms) in his job as a golf instructor, he was recommended to wait before pursuing surgery as the risks of retinal detachment are higher in patients without a vitreous detachment. He later developed a vitreous detachment in each eye spontaneously with development of a localized retinal detachment first in the right eye (Figure 7) then in the left eye, repaired with laser barricade both eyes.Fortunately, his floaters moved out of his central vision, and he did not require vitrectomy.

Case 6: In some cases, video SLO technology can help decide against surgery. This case involves a male airline pilot in his 40s who noted disturbing floaters while flying. His visual acuity was 20/20 in both eyes. Some areas of transient mild shadowing are present post-saccade (Video 8), but these are not prominent, and they were not considered to be severe enough to warrant the risks of surgery. The imaging was useful for demonstrating the mild degree of VO and supporting the decision not to operate, with which the patient was satisfied.
Case 7: Scanning laser ophthalmoscopy technology is quite useful for patient education. A 54-year-old female complained of significant floaters ongoing for 1 year. She was noted to have had a PVD 1 year earlier. We showed her and her husband the SLO video during her clinic visit while discussing management options. This allowed the patient and her husband both to see what she was experiencing. Video 9 demonstrates this.
Case 8: While the visualization and grading of the shadowing caused by VO is still a subjective assessment, there is potential for development in analysis tools that allow for objective quantification. In this patient, we added a heat map corresponding to the density of the opacity. The unmodified 30° video (Video 10) shows the floater passing through the central macula, but the heat map (Video 11) enables more striking visualization of the density of the floater. This shadowing from the opacities is even easier to visualize during pars plana vitrectomy, and it exactly correspond to the video SLO findings and the patient’s subjective description. Surgical video (Video 12) shows the nature of the opacity when illuminated with the vitrectomy light pipe.
CONCLUSION
The infrared image generated by the c-SLO shows shadows from VO projected on the surface of the retina. In patients with VO, this imaging modality can be useful during initial evaluation, correlation to symptoms, postoperative confirmation of clearance of opacities, and to review the decision on whether to operate or not to operate. This technology is excellent for patient education. Patients can visualize the shadowing from the VO as seen on the video c-SLO — one useful example being in cases of clearing vitreous hemorrhage to reassure patients that improvement is occurring.
This technology has great potential future uses, including standardizing the testing to quantify the degree and duration of reduction of light transmission caused by the opacities, and with this information, generating a “vitreous opacities impact” score. Such a score could be useful for supporting the decision for or against surgery. This testing method is offered as a simple and easy method to gather information useful in the management of patients with VO. RP








