“They’re all the same.” So reads a headline from a publication on DRCR Retina Network’s Protocol V study: laser, aflibercept, and observation are all equal when it comes to patients with diabetic macular edema (DME) and good vision. But underneath the surface, there is more to Protocol V than a one-size-fits-all conclusion. By understanding the study in depth, you can customize the results for your patients.
REVIEW OF PROTOCOL V
In 1967, Sir Stewart Duke-Elder wrote that diabetic retinopathy is “one of the major tragedies of ophthalmology of our generation.”1 The treatment at the time was pituitary ablation. In the 21st century, diabetic eye disease remains a major cause of vision loss in the working-age population both in the US and worldwide, and diabetic macular edema (DME) is the most likely cause of that vision loss. Today, intravitreal anti-VEGF drugs are the standard of care treatment for center-involved DME (CIDME) for patients with vision of 20/32 or worse. All modern studies require patients to have a maximum visual acuity (VA) of 20/32 (DRCR Protocols T and I),2 or 20/40 (PANORAMA, RISE/RIDE, VISTA/VIVID).3-5 However, many patients have DME and good vision (20/25 or better). Approximately two-thirds of patients with DME in the early Treatment in Diabetic Retinopathy Study had 20/25 or better pretreatment vision.6 How should you manage these patients who fall into the no man’s land of DME and good vision?
The DRCR Retina Network designed Protocol V to answer this question. Seven hundred and two adults with CIDME and VA of 20/25 (79 ETDRS letters) or better were randomized equally into 1 of 3 treatment groups: initial treatment with aflibercept using a treat-and-extend strategy, initial laser with pro re nata (PRN) laser retreatment q13 weeks, or initial observation. Rescue with aflibercept or laser was allowed for the laser and observation groups under prespecified conditions. Optical coherence tomography and best-corrected VA technicians were masked to the treatment arms, but patients and investigators were unmasked.
The primary outcome measure was defined as loss of at least 5 ETDRS letters of VA at 2 years. The percentage of eyes with at least a 5-letter decrease was 16% for the aflibercept arm, 17% for laser, and 19% for observation first.
However, further investigation into the treatment arms and secondary outcomes begins to show differences. Mean change in VA letter score was +1.5 letter with aflibercept, no change with laser, and -0.4 letters with observation. The percentage of eyes with VA of 20/20 or better at 2 years was greatest with aflibercept (77%), then laser (71%), and finally observation (66%).
All of these secondary outcomes are statistically significant. But are they clinically significant? How can retina specialists apply this information to individual patients?
A SNAPSHOT IN TIME
The study presents a snapshot in time, but patients aren’t standing still — they are all headed in some direction. Some, with mild retinopathy and good glycemic control, should do well in the future. Others may not be so fortunate.
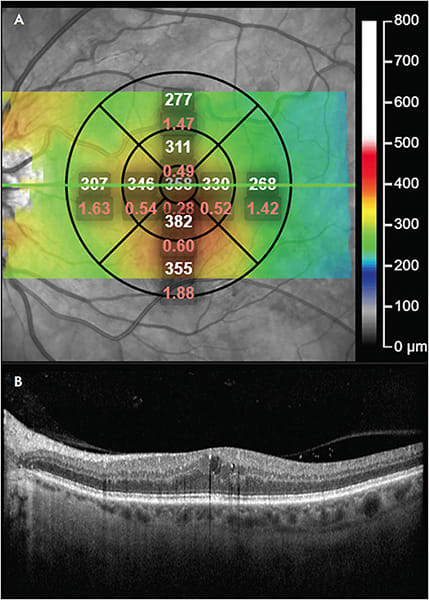
Glassman et al published a secondary analysis of Protocol V. He noted that 74% of the laser group and 64% of the observation group did not need injections at all during the 2-year study.7 If lumping all patients together gives us a result of “all treatments are the same,” could stratifying patients by risk help us direct treatment to the patients who need it and avoid treating those who do not? Glassman found that eyes were twice as likely to need aflibercept injections if they had central subfield thickness of at least 300 μm or greater, moderately severe diabetic retinopathy (Diabetic Retinopathy Severity Scale [DRSS] level 47 or higher), or required treatment of their nonstudy eye. Hemoglobin A1c ≥7.5% was associated with a higher risk of vision loss.
Are there any reasons to be hesitant about treating patients early? Certainly, cost is a dominant factor. Patients in the aflibercept arm had an average of 18 visits over 2 years, compared to 11 visits for the laser group, and 12 for observation. The treatment costs are dominated by drug charges for aflibercept, which costs $1,850 per dose. But even in the observation group, 34% of patients eventually required aflibercept, with a mean of 9 doses over 2 years, compared to 8 doses in the aflibercept early group. Another argument against early treatment is the risk of endophthalmitis, but thankfully there were no cases of endophthalmitis in Protocol V.
PATIENTS EXCLUDED FROM PROTOCOL V
Protocol V provides results that apply to some, but not all, patients with diabetes. The inclusion and exclusion criteria for the study naturally creates a subset of all diabetic patients. As we have seen, Protocol V patients were unusually good at keeping appointments, with a 92% completion rate. This rate is better than other 2-year studies: PANORAMA (79.6%), RISE (83.3%), RIDE (84.6%), VIVID (81.3%), and VISTA (82.6%). Patient compliance is much worse in the real world. One study from Germany reported that 46% of DME patients had a therapy break-off, defined as lateness >100 days.8 A US study found 25% of treated DME patients were lost to follow-up (no visits for 12 months).9
Another difference is the degree of glycemic control. Protocol V patients had a median hemoglobin A1c of 7.6%. In PANORAMA, the mean hemoglobin A1c was 8.5%. The DCCT (Diabetes Control and Complications Trial) showed that a 1% reduction in hemoglobin A1c lowers the risk of retinopathy by 30% to 40%.10 The effect on DME is less clear.11
PUTTING PROTOCOL V INTO PRACTICE: FOUR PATIENTS
To make the jump from journal page to exam room, let us hypothesize 4 case examples and see how Protocol V can apply to them.
- The perfect patient: Ms. O is a 50-year-old nurse educator with diabetes. She wears a continuous glucose monitor and has an A1c of 5.3%. Her central subfield thickness is 270 μm. She has never missed an appointment. She wants to do everything possible to keep her vision. You reassure her that she can be safely observed, and that 31% of patients in the study had spontaneous resolution of CIDME by 2 years.
- The newly diagnosed: Mr. A is a 55-year-old commercial truck driver. He was recently diagnosed with diabetes and first presented with a hemoglobin A1c of 13%. He has no visual symptoms but moderately severe nonproliferative diabetic retinopathy (NPDR) with central subfield thickness of 350 μm. He is afraid of losing his well-paying job and has worked hard to get his A1c down to 7.5%. He drives a regular schedule and will have no problem coming in for monthly visits. Based on his risk factors and the potential for worsening retinopathy in the first year of tight glucose control, you can offer him aflibercept injections, which have the highest chance of keeping his 20/20 vision at 2 years (77%). Aflibercept also has the potential to decrease the severity of his retinopathy. The PANORAMA trial showed that 58% of aflibercept-treated eyes had a 2-step or greater improvement in their DRSS compared to 6% of untreated controls.4
- The uncertain future: Ms. L is a 30-year-old woman with type 1 diabetes. Her A1c is 9.5% with moderately severe NPDR. She has a history of missing appointments due to transportation difficulties and she is worried about getting laid off from her job. Protocol V showed that early laser was associated with less need for later aflibercept treatment compared to observation (24% vs 34%). Given her uncertain future, you discuss with her the option of early macular laser treatment.
- The Protocol I patient: Mr. T is a 65-year-old man with type 2 diabetes who you are seeing at a charity clinic downtown. He does not know his A1c or blood glucose levels. He is pseudophakic. You do not have access to anti-VEGF drugs at the clinic, but you have a laser and some donated intravitreal triamcinolone. Even though you cannot treat him using the results of Protocol V, Protocol I found that in pseudophakic eyes, results with intravitreal triamcinolone plus prompt laser appeared similar to the ranibizumab arm, although with an added risk of intraocular pressure elevation. You offer him prompt laser plus triamcinolone.
Risk Factors for Worsening Diabetic Macular Edema or Vision Loss7
- Central subfield thickness of 300 μm or more
- Moderately severe nonproliferative diabetic retinopathy (DRSS level 47 or higher)
- Required treatment in fellow eye
- Hemoglobin A1c ≥7.5%
CONCLUSION
Treatment of diabetic retinopathy has come a long way since Duke-Elder. In the 1985 ETDRS study, success was defined as loss of less than 15 letters over 2 years. In that study, prompt laser decreased the rate of moderate vision loss from 24% to 12% compared to a control arm of deferred laser. Now with Protocol V and other modern studies, our measure of success is loss of less than 5 letters. Some patients can hope for a gain of vision from treatment — the average vision change for the aflibercept arm of Protocol V was +1.5 letters.
All patients are not the same, and their DME treatment shouldn’t be the same either. By reading carefully through the results of DRCR Protocol V, you can apply the results to your individual patients to give each one the best possible result. RP
REFERENCES
- Duke-Elder S. Diseases of the retina. In: Duke-Elder S, ed. System of Ophthalmology. Vol. X. Henry Kimpton; 1967:736-738.
- Diabetic Retinopathy Clinical Research Network, Wells JA, Glassman AR, et al. Aflibercept, bevacizumab, or ranibizumab for diabetic macular edema. N Engl J Med. 2015;372(13):1193-1203. doi:10.1056/NEJMoa1414264
- Brown DM, Schmidt-Erfurth U, Do DV, et al. Intravitreal aflibercept for diabetic macular edema: 100-week results from the VISTA and VIVID studies. Ophthalmology. 2015;122(10):2044-2052. doi:10.1016/j.ophtha.2015.06.017
- Brown DM, Wykoff CC, Boyer D, et al. Evaluation of intravitreal aflibercept for the treatment of severe nonproliferative diabetic retinopathy: results from the PANORAMA randomized clinical trial. JAMA Ophthalmol. 2021;139(9):946-955. doi:10.1001/jamaophthalmol.2021.2809
- Nguyen QD, Brown DM, Marcus DM, et al. Ranibizumab for diabetic macular edema: results from 2 phase III randomized trials: RISE and RIDE. Ophthalmology. 2012;119(4):789-801. doi:10.1016/j.ophtha.2011.12.039
- Relhan N, Flynn HW Jr. The Early Treatment Diabetic Retinopathy Study historical review and relevance to today’s management of diabetic macular edema. Curr Opin Ophthalmol. 2017;28(3):205-212. doi:10.1097/ICU.0000000000000362
- Glassman AR, Baker CW, Beaulieu WT, et al. Assessment of the DRCR Retina Network approach to management with initial observation for eyes with center-involved diabetic macular edema and good visual acuity: a secondary analysis of a randomized clinical trial. JAMA Ophthalmol. 2020;138(4):341-349. doi:10.1001/jamaophthalmol. 2019.6035
- Weiss M, Sim DA, Herold T, et al. Compliance and adherence of patients with diabetic macular edema to intravitreal anti-vascular endothelial growth factor therapy in daily practice. Retina. 2018;38(12):2293-2300. doi:10.1097/IAE.0000000000001892
- Gao X, Obeid A, Aderman CM, et al. Loss to follow-up after intravitreal anti-vascular endothelial growth factor injections in patients with diabetic macular edema. Ophthalmol Retina. 2019;3(3):230-236. doi:10.1016/j.oret.2018.11.002
- White NH, Sun W, Cleary PA, et al. Prolonged effect of intensive therapy on the risk of retinopathy complications in patients with type 1 diabetes mellitus: 10 years after the Diabetes Control and Complications Trial. Arch Ophthalmol. 2008;126(12):1707-1715. doi:10.1001/archopht.126.12.1707
- Singh RP, Wykoff CC, Brown DM, et al. Outcomes of diabetic macular edema patients by baseline hemoglobin A1c: analyses from VISTA and VIVID. Ophthalmol Retina. 2017;1(5):382-388. doi:10.1016/j.oret.2017.02.003








