For neovascular age-related macular degeneration (nAMD), visual outcomes have been frustratingly static in the era of anti-VEGF therapy. Although retinal treatments have improved by leaps and bounds since the end of the twentieth century — and notwithstanding the advent of potentially better options now appearing on the therapeutic horizon — it is arguable that functional results in patients with nAMD generally fall short of optimal expectations. Several explanations exist for this reality, including a plethora of real-world treatment protocols. However, stage of detection of choroidal neovascularization is undoubtedly a contributing factor.
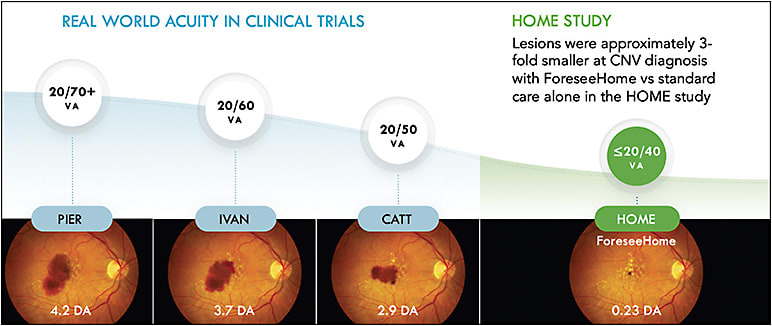
Ample evidence suggests that the stage of detection of choroidal neovascularization (CNV) directly impacts visual prognosis. Lesion size also strongly correlates with prognosis, as evidenced by the CATT study. Data from the CATT study as well as the IRIS registry demonstrated that vision at detection corresponds with long-term visual acuity after anti-VEGF treatment (Tables 1 and 2), with the CATT 5-year data demonstrating declining visual acuity over time.1 A similar series of 224 eyes assessed at Northwestern University showed that eyes that initiated treatment with good vision (defined as 20/50 or better) at onset were more than 4 times more likely than eyes with baseline vision of 20/200 or worse to have long-term vision of 20/50 or better, and twice as likely to have resolution of fluid on optical coherence tomography (OCT).2
| BASELINE VISUAL ACUITY | VISUAL ACUITY AT 1 YEAR |
|---|---|
| 20/40 | 20/25 |
| 20/60 | 20/40 |
| 20/100 | 20/60 |
| 20/250 | 20/150 |
| VISUAL ACUITY AT DIAGNOSIS | VISUAL ACUITY AT 1 YEAR |
|---|---|
| 20/20 | 20/25 |
| 20/40 | 20/40 |
| 20/60 | 20/60 |
| 20/100 | 20/100 |
| 20/200 | 20/150 |
| 20/1000 | 20/400 |
The real-world results for patients undergoing treatment for nAMD can appear discouraging. The SIERRA study, which assessed nearly 100,000 eyes over a 4-year period, found that both the number of injections and visual acuity steadily declined over this period, while the proportion of eyes receiving injections more frequently than every 8 weeks increased over that time.3 This shift may have represented clinicians’ responses to worsening results. Similarly, the SEVEN-UP study followed nAMD patients with long-term treatment and follow-up who received ranibizumab in the ANCHOR, MARINA, and HARBOR studies.4 Only 37% of patients had best-corrected visual acuity of 20/70 or better, while only 23% were better than 20/40, after an average of 7.3 years of follow-up. These poor visual acuities come at an average cost of almost $10,000 per year per beneficiary, with treatment expenses accounting for 12% of the Medicare Part B budget.5
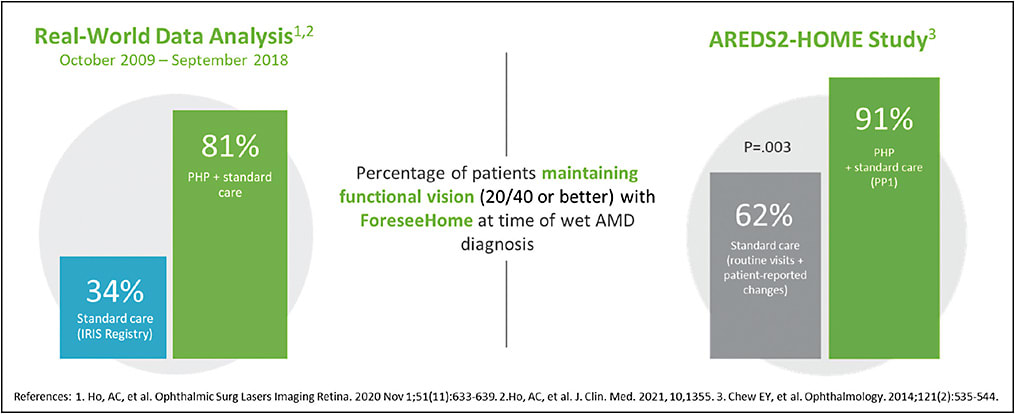
The disappointing real-world results seen with nAMD treatment are exacerbated by the current state of affairs regarding vision at presentation. Matters such as transportation and access to care surely play a role in this, but current screening and detection methods are also falling short. Amsler grid monitoring has been estimated to be only 50% effective,6 and general eye exams fail to pick up early CNV in many cases where hemorrhage is not present and fluid is not biomicroscopically visible. IRIS registry data of 160,000 eyes demonstrate that mean vision at presentation for nAMD is 20/83 for all eyes, 20/85 for first eyes, and only a marginally better 20/79 for second eyes. Given the increasing demands of an evermore active aging population, the need for functional vision has become critical. IRIS registry data show that only 34% of eyes with nAMD present for treatment with vision that is 20/40 or better.7
THE BENEFITS OF HOME MONITORING
The advent of home-based teleconnected preferential hyperacuity perimetry (PHP) has provided a means to detect patients with nAMD at an earlier stage in the disease process and with better visual acuity. The Foreseehome monitoring system (Notal Vision) is an FDA-approved device that utilizes PHP technology to monitor patients with intermediate nonexudative AMD. This device offers eye care providers an opportunity to remotely track a patient’s condition with a much higher sensitivity to detect conversion than an Amsler grid. While the IRIS registry data showed that only 34% of AMD patients monitoring with traditional methods between 2009 and 2018 presented with visual acuity of 20/40 or better at time of detection of nAMD, real-world data of almost 9,000 patients that utilized the Foreseehome device for remote monitoring during the same period revealed significantly better results.8 In this series from the IRIS registry, 83% of patients presented with vision ≥20/40 at conversion. This is comparable to the results of the pivotal HOME study.9 Although 94% of patients who used the Foreseehome device presented with visual acuity ≥20/40 at time of nAMD diagnosis, only 62% of those detected by routine exams and self-reported changes had that same level of functional vision at presentation (Figure 1). Lesion size at presentation was also significantly smaller in the Foreseehome arm of the HOME study than in other pivotal trials, a criterion that is known to impact prognosis (Figure 2).1
TOWARD SUCCESSFUL RESULTS
Although early detection is a noble objective, it is only truly consequential if it yields successful long-term visual outcomes. The Analyisis of the Long-term visual Outcomes of Foreseehome remote Telemonitoring (ALOFT) study recently sought to evaluate whether this would be possible.10
In the ALOFT study, clinical data of 3,334 eyes of 2,123 patients referred to the Foreseehome AMD monitoring program between 2010 and 2020 by multiple centers was assessed. The median visual acuity at baseline for eyes that did not convert to nAMD was 20/27 and 20/34 at final follow-up. For the 285 eyes that converted during the monitoring period (2.72% annual conversion rate), the median visual acuity at baseline, conversion, and final follow-up was 20/30, 20/39, and 20/32, respectively. This appears to suggest that early detection does correlate with long-term visual success, and that home monitoring can play a crucial role in this continuum. Moreover, a stable number of on average 6.4 injections per year in eyes treated for more than 1 year illustrated good adherence to therapy as patients realized the benefit of anti-VEGF injections.
THE CASE FOR HOME MONITORING
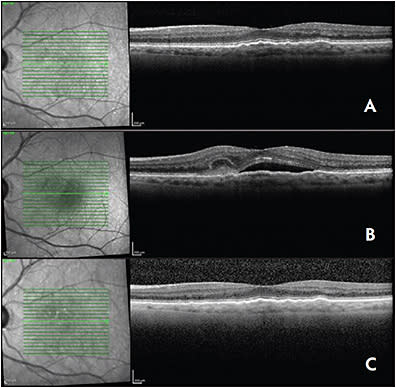
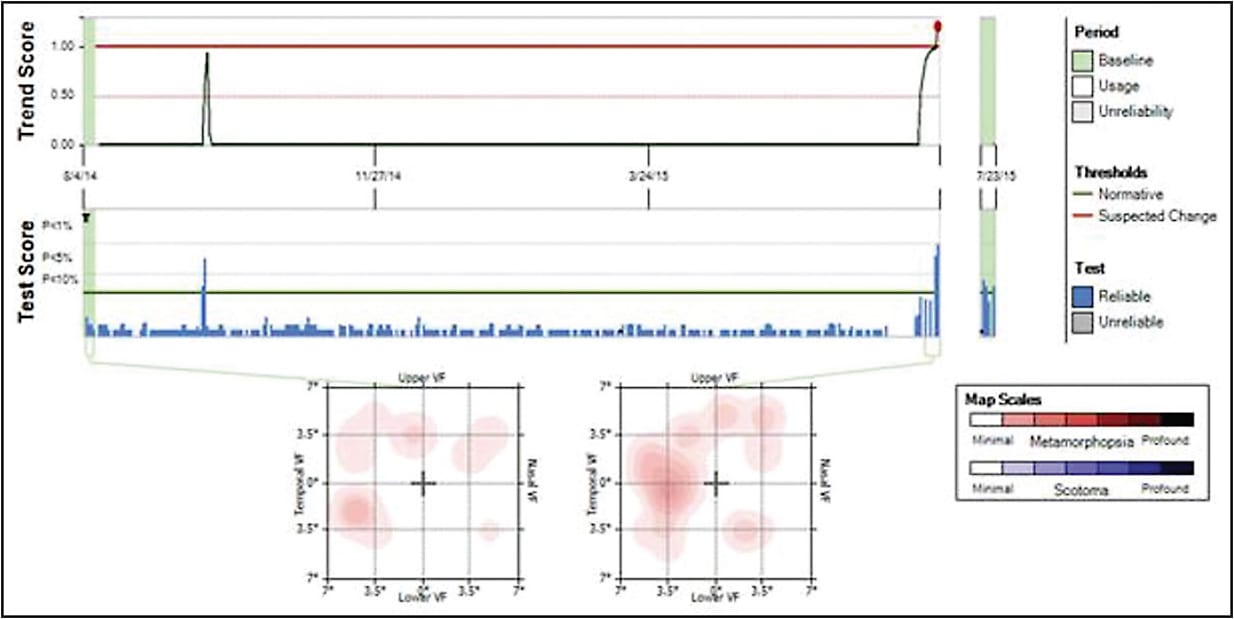
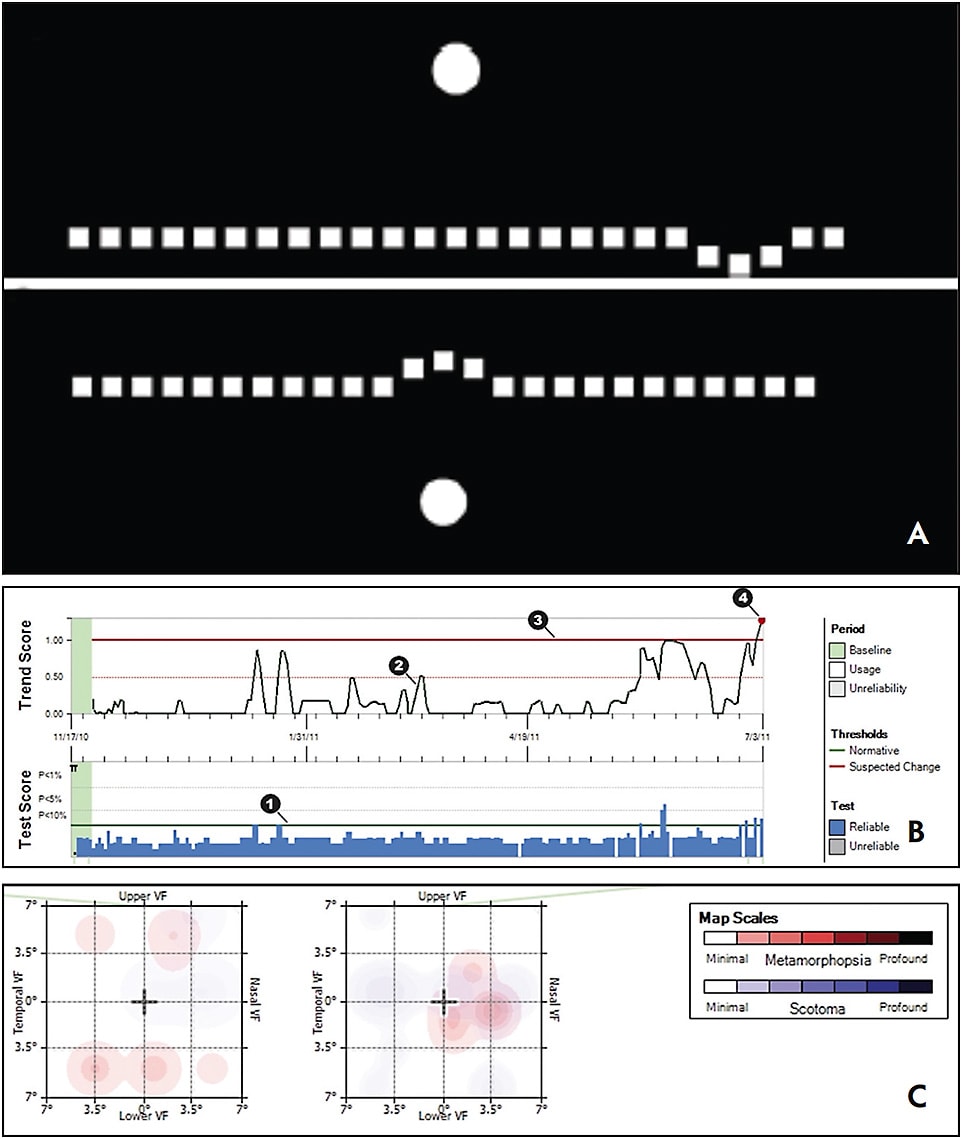
A recent patient had best-corrected visual acuity of 20/20 when started monitoring with Foreseehome. The left eye presented after a Foreseehome alert with best-corrected visual acuity of 20/40. She was asymptomatic but OCT demonstrated a clear CNV. Immediate implementation of anti-VEGF therapy yielded rapid resolution of subretinal fluid with recovery to of 20/25 vision at last follow-up. In between injection visits, the same patient monitored the fellow, right eye with a baseline vision of 20/20. When that eye produced a Foreseehome alert, the vision was 20/30. With similar intervention, the patient’s vision remained 20/30 (Figures 3 and 4).
While this case may be somewhat unique, it perfectly exemplifies the potential utility of home monitoring services for early detection of nAMD and prompt referral to a specialist. Office visits provide a snapshot of the disease course for AMD patients, but many cases of nAMD can progress asymptomatically. This phenomenon may account for the poor mean visual acuity at presentation that the data bears out. Home monitoring service providers help to close the gap between office visits and optimal timing of diagnosis of nAMD.
Compliance and interpretability of data are key factors in any successful remote monitoring program to ensure early detection and referral to a retina specialist. Ease of use for patients is essential in achieving adequate patient compliance. Preferential hyperacuity perimetry technology uses the eye’s ability to detect the offset between 2 stimuli as the basis for establishing conversion to nAMD. Although the science behind this principle is complex, its execution within the monitoring system is simple. The ALOFT study proved that the compliance rate with the Foreseehome system is extremely high, with a 5.2 tests performed per week per patient across the cohort.11 The Medicare-accredited Notal Vision Monitoring Center not only ensures a process for patient engagement that contributes to the high compliance rate associated with this program, but also provides an artificial intelligence based digital platform to automatically interpret changes in metamorphopsia maps generated by the home monitoring system. The combination of ease of patient use, monitoring center engagement with patients and direct reports to the clinician provides a complementary system that maximizes the likelihood of successful outcomes (Figure 5).
CONCLUSION
Referral patterns to retina specialists have changed dramatically in the last 2 decades, particularly since the advent of OCT. Today, patients arrive in retina clinics via multiple pathways, ranging from self referrals to those that are sent from general ophthalmology and optometric practices, among others. The potential engagement of eye care professionals in the use of remote monitoring services that extend AMD care to the patients’ home may yield better outcomes, while also ensuring that the patients that we see are truly those that are in most need of office-based care. RP
REFERENCES
- Comparison of Age-related Macular Degeneration Treatments Trials (CATT) Research Group, Maguire MG, Martin DF, et al. Five-year outcomes with anti-vascular endothelial growth factor treatment of neovascular age-related macular degeneration: the Comparison of Age-related macular degeneration Treatments Trials. Ophthalmology. 2016;123(8):1751-1761. doi:10.1016/j.ophtha.2016.03.045
- Veluswamy B, Lee A, Mirza RG, Gill MK. Correlation of baseline visual acuity with outcomes of treatment with anti-VEGF in neovascular age-related macular degeneration. Clin Ophthalmol. 2020;14:1565-1572. doi:10.2147/OPTH.S256009
- Khanani AM, Skelly A, Bezlyak V, Griner R, Torres LR, Sagkriotis A. SIERRA-AMD: a retrospective, real-world evidence study of patients with neovascular age-related macular degeneration in the United States. Ophthalmol Retina. 2020;4(2):122-133. doi:10.1016/j.oret.2019.09.009
- Rofagha S, Bhisitkul RB, Boyer DS, Sadda SR, Zhang K; SEVEN-UP Study Group. Seven-year outcomes in ranibizumab-treated patients in ANCHOR, MARINA, and HORIZON: a multicenter cohort study (SEVEN-UP). Ophthalmology. 2013;120(11):2292-2299. doi:10.1016/j.ophtha.2013.03.046
- Patel S. Medicare spending on anti-vascular endothelial growth factor medications. Ophthalmol Retina. 2018;2(8):785-791. doi:10.1016/j.oret.2017.12.006
- Faes L, Bodmer NS, Bachmann LM, Thiel MA, Schmid MK. Diagnostic accuracy of the Amsler grid and the preferential hyperacuity perimetry in the screening of patients with age-related macular degeneration: systematic review and meta-analysis. Eye (Lond). 2014;28(7):788-796. doi:10.1038/eye.2014.104
- Ho AC, Kleinman DM, Lum FC, et al. baseline visual acuity at wet AMD diagnosis predicts long-term vision outcomes: an analysis of the IRIS registry. Ophthalmic Surg Lasers Imaging Retina. 2020;51(11):633-639. doi:10.3928/23258160-20201104-05
- Ho A, Sanborn GE, Jacobs J, et al. Real-world performance of a self-operated home monitoring system for early detection of choroidal neovascularization in AMD (ForeseeHome device). Paper presented at: ASRS annual meeting; July 25, 2020; Virtual.
- AREDS2-HOME Study Research Group, Chew EY, Clemons TE, et al. Randomized trial of a home monitoring system for early detection of choroidal neovascularization home monitoring of the Eye (HOME) study. Ophthalmology. 2014;121(2):535-544. doi:10.1016/j.ophtha.2013.10.027
- Mathai M, Reddy S, Elman MJ, et al. Analysis of the long-term visual outcomes of Foreseehome remote telemonitoring - the ALOFT study. Ophthalmol Retina. 2022;S2468-6530(22)00193-2. doi:10.1016/j.oret.2022.04.016
- Busquets MA, Sabbagh O. Current status of home monitoring technology for age-related macular degeneration. Curr Opin Ophthalmol. 2021;32(3):240-246. doi:10.1097/ICU.0000000000000756








