Roth-like spots may be a clue to underlying endothelial dysfunction, making it imperative that ophthalmologists comprehensively evaluate patients presenting with this finding with consideration given to multiple etiologies. Roth spots are white-centered retinal hemorrhages, usually round, oval, or flame-shaped, that can be seen in conjunction with a wide variety of systemic conditions. First described in 1872 by Moritz Roth, Roth spots were so named 6 years later by Moritz Litten who claimed they appeared in approximately 80% of cases of subacute bacterial endocarditis.1-3 More recent research has found Roth spots in just 2% of patients with endocarditis.4 Today it is recognized as a sign of underlying disease processes, such as leukemia, anemia, preeclampsia, diabetic retinopathy, hypertension, and anoxia (see Table 1).5-7 Therefore, the differential diagnosis is rather extensive, with endothelial dysfunction being the common thread. Roth spots are most often seen in the peripheral or posterior poles during a fundoscopic exam.
|
| Adapted from Ruddy SM, Bergstrom R, Tivakaran VS. Stat Pearls. https://www.ncbi.nlm.nih.gov/books/NBK482446/ . Updated July 26, 2021. Accessed March 18, 2022. Adapted from Pittner A, Phillips H, Patel S, Kolata I. Roth spots. https://eyewiki.org . Updated August 2, 2021. Accessed March 18, 2022. |
BACKGROUND
When seen on a routine ophthalmologic exam in asymptomatic patients, Roth spots and Roth-like spots should prompt further diagnosis and evaluation. Patients can also present with signs and symptoms of systemic illness with retinal hemorrhages noted during acute evaluation. A detailed history with a full review of systems and complete exam is warranted.8,9 Symptoms associated with the more common etiologies of Roth-like spots, such as endocarditis and infection, are fever, chills, and night sweats. In the setting of hematologic disease, symptoms can include unexplained weight loss, fatigue, abnormal bleeding or bruising, and shortness of breath.
Other retinal abnormalities may accompany Roth-like spots; therefore, a comprehensive ophthalmologic examination including spectral-domain optical coherence tomography should be performed. Roth-like spots will demonstrate hypoautofluorescence and hypofluorescence due to blockage similar to other types of intraretinal hemorrhages on fundus autofluorescence and fluorescein angiography.10,11
CASE REPORT
Roth-like spots are not an uncommon finding in infants with intractable seizures secondary to pyridoxine deficiency due to genetic mutations of the ALDH7A1 gene. Early intervention with pyridoxal-5'-phosphate has been shown to halt the seizures and arrest developmental delays in these infants.12 We recently described a case that illustrates what we believe to be the first reported case of a white-centered hemorrhage in a 22-year-old woman with a 3-year history of daily, dramatic nonepileptic seizures due to pyridoxine (vitamin B6) deficiency.13
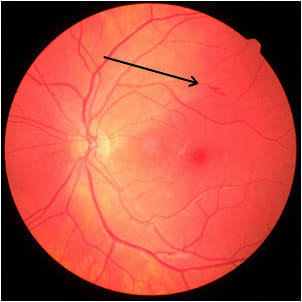
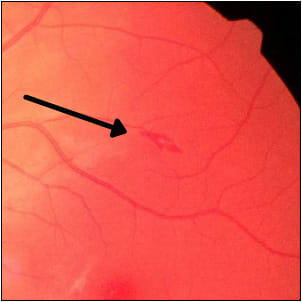
Although the patient was not fully conscious during the seizures, her electroencephalogram findings were normal. She had been diagnosed with psychogenic nonepileptic seizures 3 years prior as well as with postural orthostatic tachycardia syndrome (POTS). Ophthalmic findings were normal except for mild punctate corneal epithelial ero sions in both eyes and a white-centered hemorrhage in the left eye just superior to the macula on fundoscopic exam (Figures 1 and 2).
Upon general examination, significant findings were joint hypermobility, reduced heart rate variability, and exaggerated heart rate response to standing. Laboratory testing was normal save for high levels of anti-Sjogren’s syndrome-A antigen antibodies.
Roth-like spots and nonepileptic seizures combined with episodes of angular cheilitis and seborrheic dermatitis led to suspected pyridoxine deficiency. Forty-eight hours after daily pyridoxal-5'-phosphate 100 mg, the seizures resolved with the Roth-like spot almost completely resolving in 4 days. The underlying cause of this patient’s vitamin B6 malabsorption was lymphocytic colitis likely secondary to Sjogren syndrome. Vitamin B6 deficiency should be considered as part of the differential diagnosis in patients with psychogenic nonepileptic seizures and in white-centered hemorrhages of unknown origin.
IMPLICATIONS
Increasingly, physicians are paying more attention to the importance of the vascular endothelium both in overall health and retinal health; however, our ability to test for dysfunction in this area is limited. Numerous vascular conditions can be tied to fundus findings, with Roth-like spots being an example of this link. Frequently, Roth-like spots are the first indicator of a systemic problem. This means that when there is a finding of a white-centered hemorrhage, clinicians should be prompted to consider relatively rare systemic causes — beyond bacterial endocarditis — in the differential diagnosis. More often, patients are being encouraged to have ultrawidefield retinal imaging performed in the optometrist’s office, which will often pick up these subtle findings.
A full dilated exam with scleral depression should be performed to evaluate for other retinal abnormalities, such as diabetic retinopathy. If there is a suspicion of endocarditis, additional possible ophthalmic findings include conjunctival hemorrhage, retinal hemorrhage, cotton-wool spots, retinal infarction, chorioretinitis, and, rarely, endophthalmitis.
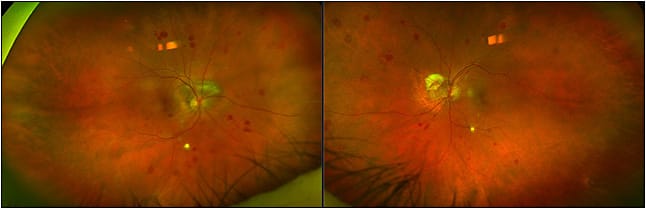
The first thing the physician should do when seeing a Roth-like spot (Figure 3), is get a good history from the patient, paying particular attention to the existence of common diseases like hypertension and diabetes. A review of systems will include finding out if the patients have recent weight loss, night sweats, chronic fatigue, or a lack of energy. These symptoms can point toward hematologic conditions like collagen vascular diseases, anemia, or even leukemia. An example of another sign to look for during an exam is small hemorrhages underneath the fingernails, which can also be an indication of associated hematologic disorders. In today’s environment, physicians should also ask about patients’ COVID status.
Patients should be referred to their primary care provider for a basic systemic evaluation, which will usually include a complete blood count, an erythrocyte sedimentation rate, and C-reactive protein level. Along with a good history, these results will start to pinpoint the cause (see sidebar). It is important not to attribute the Roth-like spot to a common condition and fail to complete a thorough investigation. For example, hypertension is prevalent, but many people with the condition do not have Roth-like spots, so the clinician should not stop there. In a tertiary care retina practice, patients with a Roth-like spot are not uncommon.
Review, History, Exam, Evaluation, Symptoms
Review
- Past medical history of prior infections, cardiac history, dental history, intravenous drug use, immunodeficiency, diabetes, hypertension, anemia, and known hematologic disorders.
- Patient’s vital signs and overall hemodynamic stability should be assessed.
Evaluation
- Complete blood count with differential to assess for leukocytosis, anemia, and thrombocytopenia along with other hematologic abnormalities.
- Fasting plasma glucose or HbA1C to assess for diabetes.
- Erythrocyte sedimentation rate, C-reactive protein and blood cultures indicated if infectious etiology is suspected.
- Transthoracic echocardiogram as initial diagnostic test if endocarditis is suspected.
- Additional tests to consider are HIV antibody testing, imaging studies, or peripheral blood smear.
Symptoms/Findings
- Endocarditis/infection: fever, chills, and night sweats; Janeway lesions; Osler nodes; splinter hemorrhages; petechiae; and cardiac murmurs.
- Hematologic disease: unexplained weight loss, fatigue, abnormal bleeding or bruising and shortness of breath.
- Leukemia: digital clubbing, the presence or absence of splenomegaly and respiratory abnormalities.
Adapted from Ruddy SM, Bergstrom R, Tivakaran VS. Stat Pearls. https://www.ncbi.nlm.nih.gov/books/NBK482446/ . Updated July 26, 2021. Accessed October 1, 2021.
CONCLUSION
Although classically associated with infective endocarditis, Roth-like spots are a nonspecific ophthalmologic finding with multiple etiologies. They can regularly be the first indication of an underlying disease process involving the vascular endothelium; therefore, a thorough history and physical examination are paramount to identifying the root cause and establishing the treatment course. When found on a routine eye examination, patients with Roth-like spots should be referred to their primary care provider for further evaluation and a comprehensive workup for systemic disease. With prompt identification and treatment, ophthalmologists and optometrists can help patients with a spectrum of previously undiagnosed systemic conditions, from anemia to leukemia to HIV to pyridoxine deficiency. Early diagnosis of these conditions with appropriate medical management can prevent further systemic or ocular complications. RP
REFERENCES
- Arora N, Dhibar DP, Bashyal B, Agarwal A. Roth’s Spots, a clinical diagnostic clue for Infective Endocarditis. Perm J. 2020;24:20.038. doi:10.7812/TPP/20.038
- Ling R, James B. White-centred retinal haemorrhages (Roth spots). Postgrad Med J. 1998;74(876):581-582. doi:10.1136/pgmj.74.876.581
- Litten M. Ueber akute maligne endocarditis und die dabei vorkommenden retinal veranderungen. Charite-Ann. 1878;3:135.
- Loughrey PB, Armstrong D, Lockhart CJ. Classical eye signs in bacterial endocarditis. QJM. 2015;108(11):909-910. doi:10.1093/qjmed/hcv055
- Wang L, Petrak M, Holz FG, Müller A, Krohne TU. Retinal hemorrhages in shaken baby syndrome. J Pediatr. 2019;207:256. doi:10.1016/j.jpeds.2018.12.054
- Ścisłowicz A, Piejko P, Nowak M, Renke P, Chaniecki P, Rucka A. Infekcyjne zapalenie wsierdzia u chorej z zaburzeniami widzenia [Infective endocarditis in a patient with vision disorders]. Pol Merkur Lekarski. 2018;45(269):198-200.
- Sabrane I, Belkhadir K, Saoudi S, Benchekroun S, El Ikhloufi M, Cherkaoui O. Taches de Roth évoquant une leucémie myéloïde : à propos d’un cas [Roth spots suggestive of myeloid leukemia: Case report]. J Fr Ophtalmol. 2018;41(9):e423-e424. doi:10.1016/j.jfo.2018.02.017
- Lin AL, Burnham JM, Pang V, Idowu O, Iyer S. Ocular manifestations of primary myelofibrosis. Retin Cases Brief Rep. 2016;10(4):364-367. doi:10.1097/ICB.0000000000000264
- Furtado JM, Toscano M, Castro V, Rodrigues MW. Roth spots in ocular toxoplasmosis. Ocul Immunol Inflamm. 2016;24(5):568-570. doi:10.3109/09273948.2015.1047035
- Zehetner C, Bechrakis NE. White centered retinal hemorrhages in vitamin b(12) deficiency anemia. Case Rep Ophthalmol. 2011;2(2):140-144. doi:10.1159/000328123
- Veronese C, Pellegrini M, Maiolo C, Morara M, Armstrong GW, Ciardella AP. Multimodal ophthalmic imaging of staphylococcus aureus bacteremia associated with chorioretinitis, endocarditis, and multifocal brain abscesses. Am J Ophthalmol Case Rep. 2019;17:100577. doi:10.1016/j.ajoc.2019.100577
- Mills PB, Footitt EJ, Mills KA, et al. Genotypic and phenotypic spectrum of pyridoxine-dependent epilepsy (ALDH7A1 deficiency). Brain. 2010;133(Pt 7):2148-2159. doi:10.1093/brain/awq143
- Driscoll D, Callanan D. Roth-like Spot in an adult with vitamin b6 deficiency and nonepileptic seizures. J VitRet Dis. August 2021. doi:10.1177/24741264211028788.








