Retina specialists are increasingly seeing patients in the operating room who require complex procedures. Retinal Physician convened a roundtable of surgeons experienced in complex surgical cases to present and discuss approaches to a series of difficult cases. Part 1 of this series appeared in the May 2021 issue.
Dr. Weng: This case is probably more challenging from a thought process standpoint than a technical standpoint. This is a 52-year-old male with keratoconus and 3 prior penetrating keratoplasties (PKs). He unfortunately had a muscle cramp in his leg in the middle of the night, jolted up, and hit his left eye on the corner of his nightstand. His open globe was repaired at an outside facility; of note, they did not find a lens at time of surgery. When he was sent to me a few weeks later, his cornea was completely opacified. B-scan ultrasonography (Figure 1) revealed a vitreous hemorrhage without evidence of retinal detachment. I decided to proceed with a pars plana vitrectomy to clear out the hemorrhage, and my cornea colleague joined me for a temporary keratoprosthesis (TKP), PK, and possible secondary intraocular lens (IOL). Intraoperatively, I was surprised by a localized inferonasal retinal detachment (Figure 2), and that’s when the mental gymnastics really happened. I think you have 4 options here. The first option is to let the cornea specialist perform PK and then you go back in and do the air–fluid exchange, endolaser, and gas. I’ve done that before successfully but sometimes find the view suboptimal through a fresh PK.


The second option is to proceed with air–fluid exchange and endolaser, inject oil to the level of the iris, let the cornea specialist do the PK, and then top off with oil. I’ve also approached it that way before, but I was hesitant in this case because he was aphakic. Given the surprise retinal detachment, we were not planning to put in the secondary IOL, so I was concerned about oil in an aphakic eye damaging the new corneal graft.
The third option is to fill the vitreous cavity with PFO, let the cornea specialist do the PK, and then either exchange the PFO for oil — but then you face the same situation as above — or leave PFO short-term. The latter has been described by others, but again with the aphakia, I was worried about the possibility of PFO damaging the cornea.
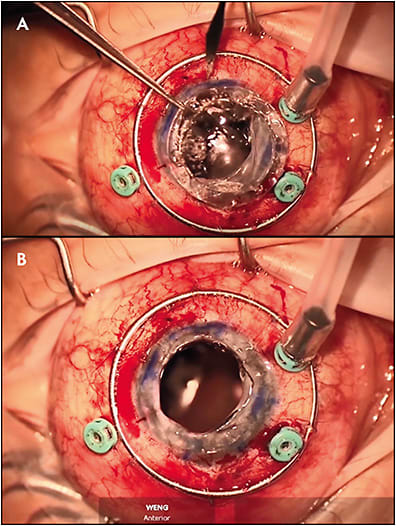
The fourth option is what I decided to proceed with, which is to do an air–fluid exchange, endolaser, let the cornea specialist do the PK under air, and then come back and inject gas. I was hesitant because I didn’t know if the eye was going to collapse. After performing a complete vitrectomy through the TKP, I performed an air–fluid exchange (Figure 3). This hampered my visualization due to condensation on the inner surface of the Eckardt; coating it with viscolastic restored my view. Once all breaks were treated with endolaser, the retina was flat under air, and I turned the field over to my colleague who then removed the TKP. With the Flieringa ring in place, the globe surprisingly stayed stable. Following suturing of the PKP graft, I went back in and touched up the air–fluid exchange and injected 16% C3F8 at the end of this case.
The 2 lessons I learned from this challenging case are that open sky under air is actually feasible if necessary, and it does not necessarily lead to globe collapse. The second lesson was that if you use an Eckardt TKP and go to air, you can get condensation similar to what can happen with an intraocular lens implant, and viscoelastic works really well to clear that up.
Dr. Kaiser: Very beautiful case. This is something we all face, unfortunately. Dr. Khanani, of those options, which would you have chosen?
Dr. Khanani: I have done what Dr. Weng did. The idea that the eye can collapse is scary, but with the air being on and going quickly from the temporary to permanent PK helps. Oil is not an option here because you don’t want the graft to fail.
Dr. Murray: Dr. Weng, a couple of things you said are important. You couldn’t really evaluate this eye preoperatively, so you did diagnostic ultrasound, which is critical. The Flieringa ring that was put on by your cornea colleague before the cornea was opened is critical because it provides support, and these eyes can collapse. You’re lucky your patient was in his 50s, so there’s a little bit of scleral rigidity.
The technique of using viscoelastic against the TKP is also critically important, because you’ll get condensation every time. Some surgeons will still use oil in these complex eyes, even though they know the cornea is going to fail. One of the most common things that happens with oil is you get an oil underfill because you tend to do the oil exchange first and then turn the case over. Often, surgeons don’t appreciate that the eye has had a slight collapse. They think they’ve got an excellent fill. And then on postoperative day 1, if they’re able to look, it’s 70% filled instead of 100%. And now you’ve protected the cornea. But you’ve compromised the detachment, so my motto always is fix the detachment first. If you don’t fix the detachment, it doesn’t matter how clear the cornea is.
I think you were thoughtful about the way you approached the case before you entered the OR, and I think you handled the surprise detachment beautifully. But when we’re working with these eyes that have had trauma, especially when the cornea is potentially opacified, you need to expect the worst, and things change a lot in in a couple of weeks. The only thing I do differently is to see these patients within a 1 or 2 days of going to the OR and almost always inject these complex trauma eyes with an anti-VEGF a 1 or 2 days before the OR to try to stabilize the potential for a bleeding risk. There’s no right or wrong answer here, so great job.
Dr. Kaiser: Dr. Vajzovic, let’s flip it around and say that the B scan actually showed a detachment. Do you buckle these cases or would you do just a straight vitrectomy in this situation?
Dr. Vajzovic: I think it depends on chronicity of the retinal detachment and my preoperative suspicion as to whether I’m going to be doing a 360 retinectomy or salvaging the retina. If it’s chronic, closed funnel, total retinal detachment, I most likely will not place the buckle and assume it’s going to need a 360 retinectomy with silicone oil tamponade. We want to salvage as much of the retina as possible, and when we are confident, I would place the buckle first.
Another factor that plays a role in getting these eyes to stay attached is proliferative vitreoretinopathy (PVR) formation, and I have found it helpful to use intravitreal methotrexate (MTX), primarily the GUARD trial injection protocol.1,2 I’ve been using this investigationally, even prior to the Guard phase 3 trial. It requires weekly injections for the first 9 injections (one at the time of surgery) followed by biweekly injections for another 4 injections (13 total), which is quite a toll and burden for patients to maintain postoperatively, and during these COVID times it has been even more troublesome. That said, I have found this MTX treatment protocol to work well in these tough PVR cases and especially trauma cases. Additionally, even patients who miss injections have done well. One concern is corneal toxicity, but with aggressive lubrication with tears and ointment, it is manageable. Lastly, MTX injections are only given in silicone oil filled eyes. I think Dr. Weng did a beautiful job as usual and going to air and gas is a perfect choice. I definitely would have tried to stay away from silicone oil to preserve cornea as much as possible. RP
REFERENCES
- Aldeyra Therapeutics announces first patient enrolled in the phase 3 GUARD trial for prevention of proliferative vitreoretinopathy [press release]. Aldeyra Therapeutics. December 19, 2019. Accessed May 20, 2021. https://ir.aldeyra.com/news-releases/news-release-details/aldeyra-therapeutics-announces-first-patient-enrolled-phase-3
- The GUARD trial - part 1: a phase 3 clinical trial for prevention of proliferative vitreoretinopathy. clinicaltrials.gov . NCT04136366. Updated January 26, 2021. Accessed May 20, 2021. https://clinicaltrials.gov/ct2/show/NCT04136366 .








