Pediatric retina is a highly subspecialized field in which the scope of practice can vary significantly. Responsibilities typically span from screening and treatment of retinopathy of prematurity (ROP) to broad coverage of pediatric retinal diseases, including ROP, persistent fetal vasculature, Coats disease, retinal detachment, and trauma. Despite these variations, given the time-sensitive nature of diagnosing and treating ROP, call responsibilities for pediatric retina patients generally involve coverage for ROP at the least. Other more urgent conditions include endophthalmitis and intraocular foreign body.
ROP is the leading cause of irreversible vision loss in the pediatric population in the United States.1 About 16,000 infants are affected by some degree of ROP, of which approximately 1,500 develop treatment-requiring disease.1 Screening occurs weekly at all level 3 and 4 neonatal intensive care units (NICUs) across the country. If a patient requires treatment, either the screening physician, or the physician covering pediatric retina call, provides timely management. Given the specialized nature of the conditions and the various systems in place for evaluation and management, call coverage for pediatric retina can be complex. For example, additional arrangements may need to be made to accommodate patients who require an examination under sedation or anesthesia, as examinations may be limited in the pediatric population.
HOSPITAL PRIVILEGES
The first steps are establishing hospital relationships and obtaining privileges. Identifying the type of institution where you will be providing care is a starting point. It may be your home institution, a nearby hospital, a rural hospital, a teaching hospital, a referral center, and/or a community hospital. Understanding the hospital’s needs and clearly identifying your role and obligations is critical. Will you be performing ROP screening? Will you be treating ROP? Are you also expected to cover other pediatric retinal emergencies outside of ROP? Will you provide phone support in addition to in-person consults? Are you expected to interact with trainees? The scope of work and expectations from each party must be clearly defined in a contract, which is typically reviewed by both parties for renewal annually.
SCOPE OF WORK
Next, it is important to determine when you will be providing these services and for what period of time during the year. If you are going to be treating ROP, it is important to know when the infants are typically screened. The earlier in the week that screening examinations are performed, the easier it can be to arrange for treatment. If screenings are performed later in the week, it may be difficult to arrange operating room time or have the pharmacy compound/provide anti-VEGF medications after hours or on the weekend. Will you be the only pediatric retina specialist providing call coverage or are there others? If you are the only one, clarify and understand your responsibilities in providing notice of your absence and how cross coverage will be arranged during this time. If you are sharing the call responsibilities with others, clearly specify how is it shared and identify the person responsible for creating the schedule.
While ophthalmology is largely practiced in an outpatient setting, hospitalized pediatric patients with ocular disease may require care while admitted. Thus, your responsibilities may include performing inpatient consultations. Understand the expectations of how consults will be requested and how urgent consults will be handled during the day if you are seeing patients at another location. At a teaching hospital with residents and fellows, they may see the patient first and triage appropriately.
FACILITIES
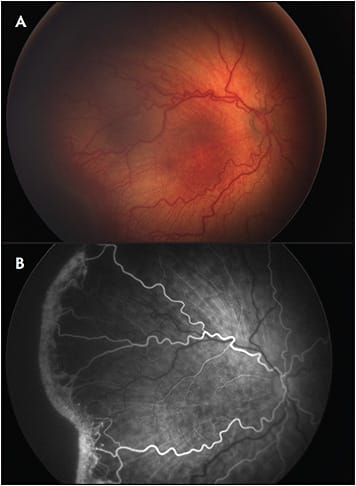
Some of the difficulties in the management of pediatric retinal diseases are the limited options in and specialized nature of the equipment. Prior to commencing care for pediatric retina patients, ensure the hospital can provide the necessary support, including trained staff and up-to-date equipment. Will you be responsible for training and monitoring staff performance? Some of the equipment required for screening and imaging require a large upfront capital investment. This may include a pediatric fundus imaging device with fluorescein angiography capability for the NICU as well as the operating room (RetCam3 ophthalmic imaging system from Natus Medical or ICON from Phoenix Technology Group; Figure 1), access to an indirect laser with a backup machine (including green 532 nm and red 810 nm lasers), timely access to intravitreal medications (such as anti-VEGF injections and intravitreal antimicrobials), and trained ancillary staff support who can operate the equipment and provide assistance during bedside procedures.
Support in the operating room is another important consideration. Staff education and pediatric specific surgical equipment, such as shorter and stiffer small-gauge instrumentation (25+ Short series from Alcon or 27-gauge short vitrectomy probe from Dutch Ophthalmic) or specific scleral buckling components, will need to be obtained. Additional specialized equipment, such as an endoscope (Endo Optiks; BVI), can greatly enhance visualization for vitrectomy in trauma cases or for patients with congenital anterior segment abnormalities. If you will be performing inpatient consultations, you will require access to portable instruments, such as a portable tonometer (Tonopen XL; Reichert Ophthalmic Instruments and Icare TAO1i; Icare USA), portable slit lamp, and wireless indirect ophthalmoscope (Keeler Instruments Inc or Heine USA Ltd).
Given the inherent challenges in obtaining a complete bedside ophthalmologic examination in pediatric patients, some may require examination under anesthesia (EUA). If an immediate EUA is required for timely diagnosis and treatment, what is the process to schedule operating room time and how quickly can it be scheduled? Is there anesthesia support in the operating room in the evening and on the weekend? For patients in the emergency department (ED), is there a separate pediatric ED or are all patients seen in a single ED? Are the resources for bedside sedation in the ED available? Additionally, some patients may require admission to the hospital, thus it is important to delineate the process for admitting these patients.
FOLLOW-UP
Once a patient is discharged from the hospital, it is critical to have a clearly defined plan for outpatient follow-up care. Coordinating follow-up ophthalmology appointments for premature infants can be challenging given multiple comorbidities that require frequent clinic visits with other subspecialties and inevitable hospital admissions. It can be difficult to coordinate care for multiple medical problems, patients may have to relocate frequently (eg, for subacute care, rehabilitation, or readmission for acute illness), and parents or guardians may not understand the severity of retinal disease and importance of follow-up to prevent vision loss. It is essential that there be a system in place, with multiple checks, to ensure optimized evaluation and management. In the management of ROP, this includes having processes for scheduling and notifying parents or guardians of examinations and necessary visits. Depending on your particular practice environment, working with the hospital to ensure there is an ROP coordinator who is involved with coordinating care for treatment and follow-up is critical. In addition, cross-training and coverage are critical components of establishing a system for preventing missed appointments and delayed care. For other pediatric retinal conditions, additional evaluations may be performed as an outpatient, but patients may require frequent inpatient visits if admitted.
COMPENSATION
Compensation for providing pediatric retina call coverage will also need to be addressed. How you are compensated is dependent on a number of factors, including your relationship with the hospital and the scope of your clinical responsibilities, and it may vary greatly across the country. Whether you are employed by the institution or work outside the institution and provide call coverage independently, compensation for coverage may be provided for a period of time and/or may vary with services provided. Specifically, you may be paid a set amount annually that covers call, inpatient consultations, and all procedures performed during this time. Alternatively, you may receive compensation for every procedure performed or patient seen, in addition to a specific amount to take call.
MALPRACTICE RISK
Medicolegal liability is often cited as the leading reason physicians do not want to be involved in ROP screening or treatment. One major concern among ophthalmologists is the long statute of limitations for children. In some states the statute of limitations extends to beyond 20 years of age. Another concern is the large awards granted in some malpractice cases involving ROP. The Ophthalmic Mutual Insurance Company (OMIC) experience with ROP malpractice claims released that the predominant reasons ROP cases were brought to litigation include transfer of care, lack of timely follow-up, and referral error.2 Having a well-established care delivery mechanism with multiple redundancies for identifying infants requiring ROP screening and ensuring timely follow-up is critical to preventing these errors.
When deciding to take pediatric retina call and provide coverage for ROP, a few major considerations are relevant. First, clearly identify the malpractice coverage being provided. Some hospitals indemnify screening and treating physicians while others may augment insurance coverage already in place. Given the length of statute of limitations in some states, it is also important to understand the difference between occurrence and claims-made policies. A claims-made policy only provides coverage if the policy is in effect both when the incident occurred and when the lawsuit is filed. Often, “tail” coverage is added to extend the coverage period of these policies. This is in contrast to occurrence policies that cover claims for events occurring during the period of coverage, even when the lawsuit is filed after the policy has lapsed. If the hospital provides a claims-made policy and tail coverage is required, clarify whose responsibility it is to purchase the policy, the covering physician or the hospital.
CONCLUSION
There are a number of complex and intertwined factors in developing a system for pediatric retina call coverage. Although there are many considerations during this process, including balancing responsibilities and risk, our ultimate goal as physicians is to provide the best possible care for our patients. The future quality of life of these patients can be greatly enhanced by timely and expert care. Keeping this in mind, it is necessary to develop a system with which patient care and safety are prioritized and the physician’s ability to provide pediatric retina coverage is optimized. RP
REFERENCES
- National Institutes of Health. Facts about retinopathy of prematurity (ROP). Accessed January 28, 2020. http://www.nei.nih.gov/health/rop/rop.asp
- Day S, Menke AM, Abbott RL. Retinopathy of prematurity malpractice claims: the Ophthalmic Mutual Insurance Company experience. Arch Ophthalmol. 2009;127(6):794-798.








