Photic retinopathy is an umbrella term that encompasses retinal damage from light of varying sources and wavelengths — ranging from infrared to ultraviolet. Reports of photic retinopathy date back to the biblical ages, when Saint Paul was temporarily blinded by “a bright light,” with full recovery of vision 3 days later.1 Photic retinopathy has also contributed to the historic development of landmark, groundbreaking ophthalmic treatments: in the 1940s, solar retinopathy would inspire Dr. Gerhard Meyer-Schwickerath to use sunlight to apply diathermy to the retina for treating retinal detachments.2 This revolutionary concept gave rise to photocoagulation. Here, we review the various forms of photic retinopathy, as well as its risk factors, pathophysiology, diagnosis, treatment, and prevention.
MECHANISMS OF INJURY
While we are most familiar with solar retinopathy, photic retinopathy also includes other mechanisms of light-induced injury; namely, lasers, arc welding, and iatrogenic intraoperative microscope lights.3-5 Solar retinopathy most commonly occurs during solar eclipses, but it also occurs during episodes of sungazing related to psychoses, religious ceremonies, military exposure, sunbathing, outdoor sports, and even drone operation.3,6
In solar retinopathy, damage is thought to be mediated by phototoxic reactions leading to photoreceptor and retinal pigment epithelium (RPE) cell death. Patients usually present with decreased visual acuity (bilateral or unilateral, depending on the exposure), central scotoma, and negative afterimage of the sun lasting several hours. On exam, the macula may have a pale, yellow spot near the fovea, which may progress to a lamellar hole or foveal depression over time. Prognosis is generally good, with improvement of visual acuity occurring within weeks, though scotomas may persist.
Arc welding is a process that binds metal to metal by utilizing electricity to generate heat, simultaneously producing significant radiation. In the rarer arc-welding retinopathy, patients typically present after exposure to arc welding without proper filtering goggle protection; symptoms include decreased vision, bilateral central scotomas, and metamorphopsia.7 Exam findings and prognosis are similar to that of solar retinopathy.
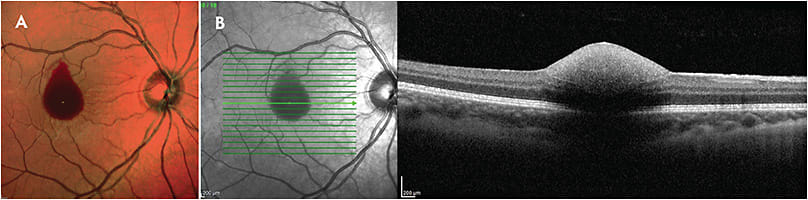
Laser-induced retinopathy is caused by exposure of the retina to high-powered lasers. Such injuries are increasingly common among children and minors due to ease of access. Patients generally present with sudden unilateral loss of vision (20/200 or worse) after laser exposure that is occasionally accompanied by a popping noise at the time of injury. They may also have a visual field defect, and examination may show retinal edema, macular hole, or hemorrhage in any location (vitreous cavity, subhyaloid, intraretinal, subretinal) (Figure 1). Prognosis is generally good, with visual acuity improving over the course of days to months. However, permanent vision loss may occur in patients with foveal involvement.
In 1983, McDonald and Irvine first described iatrogenic light-induced maculopathy from the operating microscope.8 While operating-room phototoxicity is classically associated with cataract extraction, cases of iatrogenic photic retinopathy have also been reported from coaxial microscope illumination during pterygium excision and endoillumination during vitrectomy.9,10 Patients are frequently asymptomatic or may complain of a paracentral scotoma postoperatively. Fundus examination may reveal yellow-white pigmented mottling, with fluorescein angiography (FA) classically exhibiting mottled hyperfluorescence.
RISK FACTORS
What are the risk factors for the various photic retinopathies? For solar retinopathy, Sadun et al proposed several risk factors: young age, clear crystalline lens, and lack of ocular pain while gazing at the sun.11 Emmetropia has been shown to be a risk factor, given that light is more likely to focus precisely on the retina.12,13 Climatic risk factors for solar retinopathy include bright, clear weather conditions, solar eclipse, and solar altitude greater than 60 degrees from the horizon.11
For laser-induced retinopathy, several case series suggest that it affects the male sex and pediatric population more frequently.14,15 A case series and literature review by Torp-Pederson et al suggests a rise in laser-induced retinopathy after 2013.
In iatrogenic microscope light-induced photic retinopathy, Cetinkaya et al identified the following risk factors by literature review: increased body temperature,16 increased arterial oxygen saturation,16,17 increased choroidal pigmentation,8 lightly pigmented ocular fundus,18 preexisting maculopathy,16 degree of pupillary dilatation,19 small refractive error,20 history of hydrochlorothiazide use,21 and coexistence of vascular diseases such as hypertension and diabetes mellitus.18,20-22
PATHOPHYSIOLOGY
Electromagnetic radiation, including UV and visible light, can induce retinal damage by 3 mechanisms: thermal, mechanical, and photochemical. Photochemical damage is thought to be the most common mechanism by which photic retinopathy causes retinal damage.3 Photochemical damage occurs when photon-induced chemical reactions alter cellular molecules, converting them into toxic byproducts of reactive oxygen species. Formation of these free radicals causes lipid peroxidation and retinal tissue damage. Retinal photoreceptors, particularly the outer segments, possess long membranes and thus are postulated to be especially susceptible to free-radical damage.23
Thermal and mechanical damage are lesser contributors to retinal damage from photic retinopathy but are the primary mechanisms of action for several ophthalmic laser treatments. Thermal damage occurs when light is absorbed by a chromophore, leading to the production of heat, protein denaturation, and cell death. It is the basis for argon/krypton laser photocoagulation. Mechanical damage occurs when high energy absorption causes the rapid vaporization of water and tissue, leading to an explosive force that is transmitted to adjacent tissues. The amount of damage is related, in a nonlinear fashion, to the amount of energy absorbed and the rate of delivery.4,23 This type of damage occurs with Nd:YAG lasers.
DIAGNOSIS, EXAMINATION, AND IMAGING
To discern and diagnose photic retinopathies, ophthalmologists must take a good history, soliciting occupation, hobbies, medication history, recreational drug use, and possible psychiatric history, among other risk factors. However, it is important to note that in a retrospective study of solar retinopathy in Nepal and Germany by Rai et al, 49% of patients could not remember that they had looked at the sun.13 Patients may frequently be asymptomatic or complain of central scotoma. Solar and arc welding retinopathy present similarly and may have bilateral, symmetric findings, while laser-induced and iatrogenic photic retinopathy typically present unilaterally.
Examination in solar and arc-welding retinopathy may reveal subtle, symmetrical hypopigmented foveal lesions. Acutely, fluorescence angiography is usually normal, but with chronic injury may reveal RPE atrophy without leakage. Optical coherence tomography (OCT) may reveal bilateral symmetrical atrophy in the outer retinal segments, ellipsoid zone, and RPE (Figure 2).

Of the photic retinopathies, laser-induced retinopathy may manifest with the most severe examination findings. These include retinal edema, macular hole, or hemorrhage in any location (vitreous cavity, subhyaloid, intraretinal, subretinal). OCT may show outer retinal and RPE disruption, macular edema, full-thickness macular hole, subhyaloid hemorrhage, or epiretinal membrane (Figure 3).14,24 In a case report by Tabatabaei et al, OCT angiography revealed localized low signal area in the choriocapillaris layer, demonstrating deep penetration of laser beams.25 This focal low signal area improved and demonstrated reperfusion of the choriocapillaris 70 days later.

Differing the most in presentation and diagnostic imaging, iatrogenic microscope light-induced photic retinopathy has several distinguishing features on examination. It is the most likely of all the photic retinopathies to be non-fovea involving. A literature review by Brod et al revealed that of 54 reported cases of microscope light-induced retinal injury, 28 were inferior in location, and only 4 were fovea involving.26 Fundus exam will typically reveal an elliptical area with pigmented mottling and RPE changes. Fluorescein angiography shows an elliptical area of staining and mottled hyperfluorescence overlying an area of blockage.27 OCT may show loss of the ellipsoid zone with disruption of the RPE.28
TREATMENT
There are no randomized control trials for the treatment of photic retinopathy, and no therapy has been proven effective. Most cases resolve with observation, although few cases result in permanent, but modest decrease in visual acuity with persistent scotoma or metamorphopsia. Although there are a few animal models of photic retinal injury demonstrating therapeutic efficacy of corticosteroids, evidence of efficacy in humans is anecdotal with case reports at best.29,30 Practitioners hypothesize that treatment with corticosteroids in theory reduces the cellular inflammatory response from laser injury (Figure 4).

More severe clinical presentations, particularly with laser-induced retinopathy, may rarely require surgical intervention. Nonresolving full-thickness macular holes from retinal laser injury may require pars plana vitrectomy with membrane peel for improvement in vision. Preretinal, intraretinal, and subretinal hemorrhages typically resolve with observation. Uncommonly, laser-induced retinopathy may lead to choroidal neovascular membrane formation if the laser causes a break in Bruch’s membrane.31 Intravitreal anti-vascular endothelial growth factor may be considered in these cases.
PROGNOSIS
Overall, the prognosis for photic retinopathy is good. In a study following 319 patients with solar retinopathy in Nepal and Germany, 80.9% of the affected eyes had a visual acuity of 6/12 (Snellen US 20/40) or better.13
Regarding arc-welding retinopathy, a retrospective analysis by Zhang et al showed patients with presenting best-corrected visual acuity (BCVA) of Snellen equivalent 20/25 to 20/100 improved to a final BCVA of 20/25 to 20/66 over an average of 1 to 4 months.32 Final BCVA was significantly correlated with baseline BCVA based on univariate regression analysis.32
While there are few data on visual outcomes after iatrogenic microscope light-induced photic retinopathy, nonfoveal retinal damage typically portends excellent prognosis, and patients are frequently asymptomatic. Lastly, although laser-induced retinopathy can manifest with more severe clinical signs, like macular hole and hemorrhage, prognosis is generally good for these patients as well. In a case series by Mtanes et al, 6 out of 7 patients recovered to BCVA of 20/40 or better.15 Another multicenter case series showed that higher powered lasers >5 milliwatts are significantly associated with worse visual recovery — with only 5 out of 36 making full recovery and 31 out of 36 having lasting symptoms.14
PREVENTION AND PROTECTION
Given the lack of effective treatments for photic retinopathy, education, prevention, and protection are all of paramount importance. The American Academy of Ophthalmology recommends protection with sunglasses that block 99% to 100% of UVA and UVB light. Before a solar eclipse, the government should provide adequate public health information educating the public that an eclipse is not safe to view with the naked eye. The safest and cheapest method involves a pinhole system with a screen 50 cm behind its opening.3 Alternatively, silver, aluminum, or chromium may be embedded in films to attenuate UV, visible, and infrared energy. In addition, arc welders’ glass numbers 12 and 14, as well as aluminized Mylar, are safe filters for eclipse viewing.3
For arc welders’ protection, the US Department of Labor’s Occupational Safety and Health Administration advises goggles or head gear with the appropriate minimum protective shade number, depending on what arc current is being utilized.33 Parents should avoid giving children laser pointers given the higher risk and prevalence of laser-induced retinopathy in this population. Lastly, regarding iatrogenic microscope light-induced photic retinopathy, Khwarg et al found that the most significant, and also most modifiable, risk factor is prolonged duration of surgery.21 Thus, it is recommended to perform surgeries safely and efficiently, avoiding prolonged operating times if possible. With the operating microscope, surgeons may use ultraviolet filters and opaque filters when applicable.
CONCLUSION
Although light is requisite for vision, excess and concentrated forms of light can cause phototoxicity to the retina in the form of photic retinopathy. We have reviewed the following various forms of photic retinopathy: solar retinopathy, arc welding retinopathy, laser-induced retinopathy, and iatrogenic microscope light-induced retinopathy. Safety and education are essential for prevention and protection from light-induced retinal damage. Thankfully, these photic retinopathies generally have good prognoses. RP
REFERENCES
- Bullock JD. The blindness of Saint Paul. Ophthalmology. 1978;85(10):1044-1053.
- Meyer-Schwickerath GR. The history of photocoagulation. Aust N Z J Ophthalmol. 1989;17(4):427-434.
- Begaj T, Schaal S. Sunlight and ultraviolet radiation—pertinent retinal implications and current management. Surv Ophthalmol. 2018;63(2):174-192.
- Barkana Y, Belkin M. Laser eye injuries. Surv Ophthalmol. 2000;44(6):459-478.
- Azzolini C, Brancato R, Venturi G, Bandello F, Pece A, Santoro P. Updating on intraoperative light-induced retinal injury. Int Ophthalmol. 1994;18(5):269-276.
- Rohring V, Rehmani A, Smith E, Smith E, Berg P. Drone retinopathy. J Curr Ophthalmol. 2019;31(1):106-108.
- Uniat L, Olk RJ, Hanish SJ. Welding arc maculopathy. Am J Ophthalmol. 1986;102(3):394-395.
- McDonald HR, Irvine AR. Light-induced maculopathy from the operating microscope in extracapsular cataract extraction and intraocular lens implantation. Ophthalmology. 1983;90(8):945-951.
- Kuhn F, Morris R, Massey M. Photic retinal injury from endoillumination during vitrectomy. Am J Ophthalmol. 1991;111(1):42-46.
- Bonyadi MJ. Bilateral photic maculopathy following pterygium excision: spectral domain optical coherence tomography findings. J Ophthalmic Vis Res. 2016;11(4):436-438.
- Sadun AC, Sadun AA, Sadun LA. Solar retinopathy a biophysical analysis. Arch Ophthalmol. 1984;102(10):1510-1512.
- Yannuzzi LA, Fisher YL, Slakter JS, Krueger A. Solar retinopathy: a photobiologic and geophysical analysis. 1989. Retina. 2012;32 Suppl 1:28-43.
- Rai N, Thuladar L, Brandt F, Arden GB, Berninger TA. Solar retinopathy: a study from Nepal and from Germany. Doc Ophthalmol. 1998;95(2):99-108.
- Torp-Pedersen T, Welinder L, Justesen B, et al. Laser pointer maculopathy – on the rise? Acta Ophthalmol. 2018;96(7):749-754.
- Mtanes K, Mimouni M, Zayit-Soudry S. Laser pointer-induced maculopathy: More than meets the eye. J Pediatr Ophthalmol Strabismus. 2018;55(5):312-318.
- Michels M, Sternberg P. Operating microscope-induced retinal phototoxicity: Pathophysiology, clinical manifestations and prevention. Surv Ophthalmol. 1990;34(4):237-252.
- Jaffe GJ, Irvine AR, Wood IS, Severinghaus JW, Pino GR, Haugen C. Retinal phototoxicity from the operating microscope: the role of inspired oxygen. Ophthalmology. 1988;95(8):1130-1141.
- Byrnes GA, Antoszyk AN, Mazur DO, Kao TC, Miller SA. Photic Maculopathy after Extracapsular Cataract Surgery: A Prospective Study. Ophthalmology. 1992;99(5):731-737.
- Khwarg SG, Geoghegan M, Hanscom TA. Light-induced maculopathy from the operating microscope. Am J Ophthalmol. 1984;98(5)628-630.
- Kleinmann G, Hoffman P, Schechtman E, Pollack A. Microscope-induced retinal phototoxicity in cataract surgery of short duration. Ophthalmology. 2002;109(2):334-338.
- Khwarg SG, Linstone FA, Daniels SA, et al. Incidence, risk factors, and morphology in operating microscope light retinopathy. Am J Ophthalmol. 1987;103(3 Pt 1):255-263.
- Cetinkaya A, Yilmaz G, Akova YA. Photic retinopathy after cataract surgery in diabetic patients. Retina. 2006;26(9):1021-1028.
- Youssef PN, Sheibani N, Albert DM. Retinal light toxicity. Eye. 2011;25(1):1-14.
- Alsulaiman SM, Alrushood AA, Almasaud J, et al; King Khaled Eye Specialist Hospital Collaborative Retina Study Group. High-power handheld blue laser-induced maculopathy: the results of the king khaled eye specialist hospital collaborative retina study group. Ophthalmology. 2014;121(2):566-572.
- Tabatabaei SA, Soleimani M, Bohrani B, Banafsheafshan A, Faghihi S, Faghihi H. Multimodal imaging in photic retinopathy. Int J Ophthalmol. 2019;12(3):523-525.
- Brod RD, Olsen KR, Ball SF, Packer AJ. The site of operating microscope light-induced injury on the human retina. Am J Ophthalmol. 1989;107(4):390-397.
- Robertson DM, Feldman RB. Photic retinopathy from the operating room microscope. Am J Ophthalmol. 1986;101(5):561-569.
- Almeida FPP De, Alliman KJ, Flynn HWJ. Photic maculopathy following exchange of crystalens: clinical and spectral-domain OCT features. Retinal Physician. 2009. https://www.retinalphysician.com/issues/2009/october-2009/case-study
- Rosner M, Lam TT, Jun J, Tso MOM. Methylprednisolone Ameliorates Retinal Photic Injury in Rats. Arch Ophthalmol. 1992;110(6):857-861.
- Hossein M, Bonyadi J, Soheilian R, Soheilian M, Peyman GA. SD-OCT features of laser pointer maculopathy before and after systemic corticosteroid therapy. Ophthalmic Surg Lasers Imaging. 2011;42.
- Fujinami K, Yokoi T, Hiraoka M, Nishina S, Azuma2 N. Choroidal neovascularization in a child following laser pointer-induced macular injury. Jpn J Ophthalmol. 2010;54(6):631-633.
- Zhang C, Dang G, Zhao T, Wang DL, Su Y, Qu Y. Predictive value of spectral-domain optical coherence tomography features in assessment of visual prognosis in eyes with acute welding arc maculopathy. Int Ophthalmol. 2019;39(5):1081-1088.
- Occupational Safety and Health Administration. Eye protection against radiant energy during welding and cutting in shipyard employment. Accessed May 12, 2020. https://www.osha.gov/Publications/OSHAfactsheet-eyeprotection-during-welding.pdf








