Since its commercial introduction in 2006, optical coherence tomography (OCT) has restructured the landscape of ophthalmic imaging and practice patterns. Here was a technology that not only produced tomographic views of retinal anatomy, but offered quantitative data that was previously not obtainable—all in an easy-to-use diagnostic system.
As is the case with most diagnostic tools, the data produced is only as good as the effort and knowledge of the operator. The perception that producing quality images does not require extensive training of the imager may result in less-than-optimal images, which may then result in a missed diagnosis or erroneously alter the treatment plan.
PROPER TRAINING IS KEY
Proper, extensive training is critical for imagers. Along with learning how to utilize the software, the imager must also be acutely aware of ocular anatomy, disease pathology, and how the pathology affects the patient’s vision.
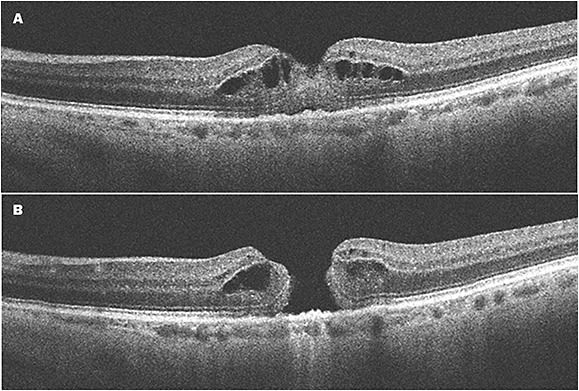
For instance: All OCT systems are equipped with an internal fixation target. When a patient with a full-thickness macular hole (or other pathology that produces a central scotoma) is directed to fixate on the target, the system will scan the patient’s subjective fixation. The resulting scan will be placed juxta-foveal, producing an image that does not reflect the pathology. A trained imager will recognize anatomical structures that indicate the patient is not fixating centrally and should adjust accordingly. In a busy clinical practice, this type of error may go unnoticed.
A trained imager also recognizes disease pathology and scans appropriately. A quality scan of the fovea is beneficial, but not all pathology is within the fovea or central macula. The imager should always consider what scan module to utilize, as well as what areas of the retina should be scanned.
Take diabetic retinopathy and macular edema, for example. A single horizontal line scan that intersects the fovea may appear normal, but if the imager also scans vertically, pathology above and below the fovea may be found. This is also true with the scan modality—protocol should always include a volumetric, or cube scan that covers the entire macula.
With most OCT systems, the software allows for scans to be set as references, which the imager can use to ensure the same scan placement every time the patient is scanned. However, if the initial scan is incorrectly placed, subsequent scans will also be misplaced. This further emphasizes the need for the imager to be trained properly.
4 OCT IMAGING TIPS
1. FINE FOCUS.
The OCT scan has a corresponding fundus image, usually taken in infrared. This helps to orient the imager and viewer, and to illustrate where the scan line is placed on the retina. Having fine focus on the fundus image is critical—the imager should ensure the finest focus on the smallest structure in the center of the frame. Once focus is achieved, then concentrate on the B scan image.
In the case of glaucoma nerve fiber layer scans, focus is even more critical. Focusing deeper than the nerve fiber layer will result in erroneous nerve fiber layer thickness measurement.
2. ID ARTIFACTS.
Learn what artifacts look like. Anything that affects light will affect the image. Therefore, if the patient has a cataract, some of the returning light from the retina will be scattered and not read. Using acomposite function on the OCT will help, but the imager needs to work to find the clearest view in the patient’s optical path.
One of the biggest issues affecting images is dry eyes. To produce the best image possible, the patient’s tear film should be uniform. Dry eye artifacts appear on the fundus image as circular “spots,” and the OCT B scan will appear hazy or out of focus.
Imaging the patient prior to workup is ideal. The effect of drops and applanation will affect the tear film. Always keep artificial tears handy.
If the final image is degraded due to lens or cornea, the imager should take an anterior image reflecting the reason the image is not optimal. This not only helps the viewer understand why the image is not ideal, but also helps the imager when taking future scans of that patient.
3. CLEAR COMMUNICATION.
This applies to communication with clinicians, staff, and the patient. Clinicians need to be clear about OCT protocol they need to diagnose and decide treatment. Not all patients are the same, just as not all retinal disease is the same. Having a clear protocol keeps everyone on the same page, especially if multiple staff members are imaging patients.
Communication with staff is also key. For example, technicians who do not image need to understand how drops and applanation disrupt the optimal optical pathway for imaging.
The imager also must communicate efficiently with the patient. Explaining what is required of the patient and what they can expect during the process will only make the imager’s job easier. Remind the patient that they should blink normally, unless instructed otherwise. Indicating where they should focus, and what not to focus on, will elicit a much more cooperative patient.
4. KEEP LEARNING.
Technology is changing constantly, and even if the hardware or software used in your practice doesn’t change, imagers are finding new and better techniques all the time. Stay in touch with other imagers. Join organizations such as the Ophthalmic Photographers’ Society or one of the communities on social media. These can be perfect venues for voicing issues with technique, artifacts, and other helpful advice from users all over the world.
BETTER TECHNOLOGY CALLS FOR BETTER TRAINING
With the advent of newer technology that allows for more data and faster scans, it is imperative that the imager have proper training to ensure a knowledge base that can be relied upon to make the decisions that lead to correct diagnosis and treatment plans.
Constant vigilance and communication on the part of both the imager and the clinician is critical to success.

WHAT MAKES A GOOD IMAGER?
The OCT imager must possess certain qualities to ensure high-quality scans:
- Knowledge of ocular anatomy
- Understanding of the effect of disease pathology on vision
- Recognition of disease pathology, both anatomically and how it presents on OCT
- Communication with the clinician
- Constantly critiquing their images
- Understanding of how OCT technology works
- The desire to continue learning









