Diagnosis of intraocular tumors is based on clinical and ancillary imaging studies, including ultrasonographic evaluation. The rate of clinical misdiagnosis of uveal melanoma is estimated to be less than 1%.1 Hence, biopsies are reserved for diagnosis of atypical cases, confirmation of a known diagnosis prior to definitive treatment, such as plaque radiotherapy or enucleation, and prognostic studies. Common indications for diagnostic biopsies include differentiation between melanocytic lesions and amelanocytic lesions, such as amelanotic melanoma, metastasis without a known primary, and uveal or vitreoretinal lymphoma. Depending on the tumor location, size, suspected diagnosis, and media opacities, different biopsy techniques can be performed.
BIOPSY TECHNIQUE
Iris
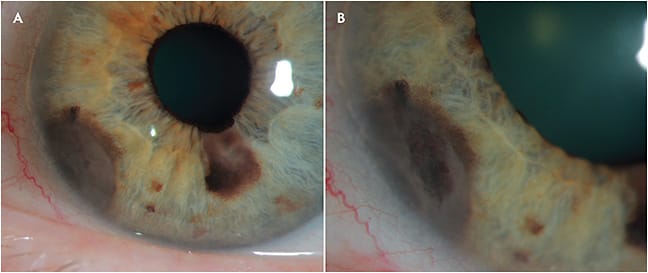
For small tumors without invasion of the angle, the small-incision guarded hydroaspiration (SINGH) technique can be considered to obtain an excisional biopsy with clear margins.2 For larger lesions, transcorneal fine-needle aspiration biopsy (FNAB) is the best approach (Figure 1). A 25- to 30-gauge needle is passed through a clear corneal incision parallel to the iris plane, near the lesion and not going across the pupil. Aspiration of tumor material is performed with the bevel up while slowly turning the needle.3,4 Some authors recommend using the bevel down, in a “vacuum cleaner” fashion.5 We prefer using the bevel up to visualize the cells entering the needle.
Ciliary body
For small tumors of unknown origin, iridocyclectomy is a good option for excisional biopsy, because it offers both diagnosis and treatment in a single procedure. However, such biopsies should be performed with particular caution for ciliary body medulloepitheliomas. Enucleation or adjuvant brachytherapy therapy may be required, because excision alone is not sufficient for local control and may result in metastatic spread.6,7 For larger tumors, trans-scleral FNAB can be performed (Figure 2). The tumor area is marked by transillumination. A 3-mm square scleral flap of 80%8 thickness is marked, and a 25- to 30-gauge needle attached to a 5-mL syringe by a short tubing, is inserted tangentially to aspirate the tumor cells.

Choroid
For pre-equatorial tumors, biopsy technique is similar to that used in ciliary-body tumors. The scleral flap is optional, depending on the tumor position and the surgeon’s preference. In some cases, as in almost all melanomas, plaque therapy is performed at the same time as the biopsy. In those cases, the scleral flap can be omitted. In other cases, we recommend performing a scleral flap. Careful hemostasis and cautery after needle withdrawal are other measures that may improve safety and decrease the risk of tumor seeding.
In postequatorial tumors, depending on the experience of the surgeon, different techniques can be selected. For the experienced pathologist, a small sample with just a few cells can be enough for diagnosis, so FNAB can be performed either directly through the sclera or with the use of trocars 180 degrees away at the pars plana, 4 mm behind the limbus (Figure 3).9 Using a valved 25-gauge canula offers the potential advantage of isolating the needle tract and allowing retrieval of the contaminating cells.10

Different viewing systems can be used depending on surgeon experience, such as indirect biomicroscopy, microscopy with contact or no-contact viewing systems, and optical coherence tomography (OCT)-guided methods.11 Tissue samples can also be obtained by a vitrectomy-assisted approach.12
Vitreous
The most frequent indication for a vitreous biopsy in ocular oncology is primary vitreoretinal lymphoma (PVRL). In those cases, FNAB is not a good option, because of the difficulty to acquire tumor cells, so vitrectomy must be performed if cytologic diagnosis is needed. First, a sample of undiluted vitreous should be taken, with the infusion canula closed and using a low cut rate with a 5-mL syringe. Then the second sample of diluted vitreous can be submitted together with the cassette for examination.13,14 Air infusion is another elegant way of obtaining such specimens.15 In presence of subretinal infiltrates, subretinal aspiration can enhance positive yield.
SPECIMEN HANDLING
Aspirated material from FNAB samples can be processed with different methods of sample concentration. Liquid-based cytology techniques like ThinPrep (Healthdxs) processing system are widespread in many countries, as they preserve morphology and allow cells to be placed in a monolayer. This is particularly important in small samples with limited material, such as ophthalmic FNAB samples.16,17 However, if handled carefully, other methods including cytocentrifugation, Millipore filter concentration, and celloidin bag techniques18 can be used with good results and are good options in settings where access to liquid-based cytology is limited. Cell-block preparation can be performed regardless of the method used (liquid-based vs conventional cytology) in cases of sufficient sample.19 Although immunostaining is possible on cytologic smears (immunocytochemistry), most pathology laboratories prefer immunohistochemistry methods on paraffin-embedded cell blocks.20
Differential diagnosis of intraocular tumors is broad and can be separated into 2 groups: melanocytic and non-melanocytic lesions. The first step in cytological evaluation of FNAB specimens is to identify the presence of melanic pigment in the cell cytoplasm of lesional cells and to identify the presence of spindle cells (Figure 4).21,22 Melanin is finely granular and is evident in HE stained slides; however, it can be focal and subtle. Spindle cells are observed in 98% of uveal melanoma samples and are unlikely to be present in a metastatic tumor.23 Careful examination by the pathologist is mandatory, and interpretation within the clinical context is fundamental for correct diagnosis.

MELANOCYTIC LESIONS
Melanocytic intraocular lesions include ocular melanoma and nevi. Cytologic classification of melanoma cells is based on the modified Callender system and includes spindle type A (nevus-like) cells, spindle type B, epithelioid, and mixed spindle B and epithelioid cells.24 Spindle type A cells have oval, folded nuclei with small nucleoli and fusiform appearance. Spindle type B cells are large and the nuclei are cigar shaped with larger nucleoli and tend to have bipolar cytoplasmic processes. Epithelioid melanoma cells are large and polygonal, with irregular nuclei with coarse chromatin and distinct nucleoli. While melanomas can be composed of epithelioid and spindle cells, uveal nevi are exclusively composed of type A spindle cells. Distinction between nevi and spindle-cell melanoma in FNAB specimens can be challenging.25 Interpretation of the cytologic finding should be done in the clinical context and in communication with the cytopathologist.
NONMELANOCYTIC NEOPLASMS
Nonmelanocytic lesions include metastasis, lymphoproliferative processes, retinoblastoma, choroidal hemangioma, and medulloepithelioma. Age and clinical information are mandatory for correct assessment.
Metastases are the most common intraocular malignancy.26 Most patients have known history of cancer; however, identification of the ocular tumor may precede a cancer diagnosis or result in the identification of a recurrence. Breast cancer represents almost half of metastasis, followed by lung and gastrointestinal tract cancer.27 Cytological characteristics are of those of the primary tumor. In some cases, immunohistochemistry on cell-block preparation may be needed for characterization of primary origin. In presence of a lesion suspicious of metastasis, computed tomography scanning of the chest, abdomen, and pelvis should be performed before intraocular tumor biopsy is attempted, because a biopsy area outside of the choroid with more straightforward surgical access is usually identified.
Lymphoproliferative processes may secondarily affect the uveal tract and retina. Patient history and monomorphic and discohesive nature of cells should raise suspicion. Primary vitreoretinal lymphomas are almost always diffuse, large, B-cell type characterized by cells with relatively large nuclei with prominent nucleoli, associated with necrosis.28 Cellular features usually suffice to establish the diagnosis. Immunohistochemistry can be helpful in problematic cases. Specifically, immunostains can confirm the lymphoid B-cell phenotype. A positive flow cytometry result is helpful because it establishes light chain restriction (monoclonality). Importantly, a negative flow cytometry result can be misleading because widespread necrosis, common in these specimens, often causes false-negative flow cytometry results.
FNAB should not be performed in patients with suspicion of retinoblastoma because of the significant risk of tumor seeding.29-31 Cytological diagnosis can also be done in cerebrospinal fluid or extraocular metastasis. Smears show small undifferentiated cells with markedly hyperchromatic nuclei, frequent apoptotic debris and mitotic figures.32 Presence of calcifications is a useful clue in retinoblastoma. In well-differentiated tumors, cytoplasmic processes and Flexner-Wintersteiner rosettes may be seen.
Medulloepithelioma is a rare neoplasm that occurs in children. Cytologic preparations show single or grouped primitive looking cells with high nuclear–cytoplasmic ratio, nuclear molding, and rosette formation.33
COMPLICATIONS
More invasive procedures, such as iridocyclectomy, are associated with a higher number of complications such as glare, monocular diplopia, hyphema, cataract, infection, intraocular pressure fluctuations, and postsurgical astigmatism.
Techniques that are less invasive than FNAB have fewer and more minor complications. The most common complication is a small hemorrhage at the site of retinal puncture (Figure 3).9,34 To prevent massive hemorrhage, vascular tumors such as hemangiomas should not be biopsied and vascular structures of solid tumors should be avoided. If active bleeding is seen during the procedure, pressure should be raised either by pressing the entrance site with a cotton tip, injecting saline solution, or increasing the pars plana infusion pressure, if available.
Only 2 cases of endophthalmitis have been reported.35,36 It is essential to perform the procedure under sterile conditions after asepsis and antisepsis with povidone–iodine 5%. Further studies have not shown any case of endophthalmitis.37 Retinal detachment after FNAB for choroidal tumors is extremely rare. The retinal break created at the biopsy site is small and self-sealed by the hemorrhagic clot. The tumor also acts as a “scleral buckle” indenting on the retinal site, preventing detachment.
Seeding has always been one of the main concerns for intraocular biopsies. Although the literature has reported seeding on the needle tract,38 the number of tumor cells was less than that associated with tumor growth in experimental models.39 In clinical practice, the rate of extraocular extension after FNAB is low, and a few cases of extraocular extension of uveal melanoma have been reported. Special care should be taken in avoiding diagnostic biopsy in cases that could harbor unsuspected retinoblastoma, because of the high risk of seeding the tumor outside the eye.29-31
CONCLUSION
Although diagnosis on most intraocular tumors can be done based on clinical examination and imaging studies, for atypical cases, diagnostic biopsy is a safe method.40 However, a negative cytologic diagnosis should not be considered proof that an intraocular malignancy does not exist. In addition to use of careful surgical techniques, proper sample handling and consultation with an expert cytopathologist are essential to reaching the correct diagnosis. RP
REFERENCES
- Accuracy of diagnosis of choroidal melanomas in the Collaborative Ocular Melanoma Study. COMS report no. 1. Arch Ophthalmol. 1990;108(9):1268-1273.
- Singh AD. Small incision guarded hydroaspiration of iris lesions. Br J Ophthalmol. 2017;101:1570-1575.
- Gokhale R, Medina CA, Biscotti CV, Singh AD. Diagnostic fine-needle aspiration biopsy for iris melanoma. Asia Pac J Ophthalmol (Phila). 2015;4(2):89-91.
- Shields CL, Manquez ME, Ehya H, Mashayekhi A, Danzig CJ, Shields JA. Fine-needle aspiration biopsy of iris tumors in 100 consecutive cases: technique and complications. Ophthalmology. 2006;113(11):2080-2086.
- Grossniklaus HE. Fine-needle aspiration biopsy of the iris. Arch Ophthalmol. 1992; 110(7):969-976.
- Kaliki S, Shields CL, Eagle RC Jr, et al. Ciliary body medulloepithelioma: analysis of 41 cases. Ophthalmology. 2013;120(12):2552-2559.
- Poon DS, Reich E, Smith VM, et al. Ruthenium-106 Plaque Brachytherapy in the Primary Management of Ocular Medulloepithelioma. Ophthalmology. 2015;122(9):1949-1951.
- Singh AD, Biscotti CV. Fine needle aspiration biopsy of ophthalmic tumors. Saudi J Ophthalmol. 2012;26(2):117-123.
- Singh AD, Pelayes DE, Brainard JA, Biscotti CV. History, indications, techniques and limitations. Monogr Clin Cytol. 2012;21:1-9.
- Singh AD, Aziz HA, Pelayes D, Biscotti CV. Twenty-five-gauge cannula–assisted fine-needle aspiration biopsy of choroidal melanoma: cytopathological analysis. Retina. 2017;37(9):1674-1677.
- Grewal DS, Bhullar PK, Pasricha ND, et al. Intraoperative 4-dimensional microscope-integrated optical coherence tomography-guided 27-gauge transvitreal choroidal biopsy for choroidal melanoma. Retina. 2017;37(4):796-799.
- Nagiel A, McCannel CA, Moreno C, McCannel TA. Vitrectomy-assisted biopsy for molecular prognostication of choroidal melanoma 2 mm or less in thickness with a 27-gauge cutter. Retina. 2017;37(7):1377-1382.
- Coupland SE. Vitreous biopsy: specimen preparation and interpretation. Monogr Clin Cytol. 2012;21:61-71.
- Hwang CS, Yeh S, Bergstrom CS. Diagnostic vitrectomy for primary intraocular lymphoma: when, why, how? Int Ophthalmol Clin. 2014;54(2):155-171.
- Gariano RF. Vitreous biopsy with air infusion: safety and effectiveness. Retina. 2000;20:422-423.
- Brainard JA, Biscotti CV. Cytological preparation. Monogr Clin Cytol. 2012;21:10-16.
- Pelayes DE, Zarate JO. Fine needle aspiration biopsy with liquid-based cytology and adjunct immunohistochemistry in intraocular melanocytic tumors. Eur J Ophthalmol. 2010;20(6):1059-1065.
- Engel H, de la Cruz ZC, Jimenez-Abalahin LD, Green WR, Michels RG. Cytopreparatory techniques for eye fluid specimens obtained by vitrectomy. Acta Cytol. 1982;26(4):551-560.
- Kim RS, Chevez-Barrios P, Bretana ME, Wong TP, Teh BS, Schefler AC. Histopathologic analysis of transvitreal fine needle aspiration biopsy needle tracts for uveal melanoma. Am J Ophthalmol. 2017;174:9-16.
- Duker JS, Shields JA, Ross M. Intraocular large cell lymphoma presenting as massive thickening of the uveal tract. Retina. 1987;7(1):41-45.
- Biscotti CV, Singh AD. Uveal melanoma: diagnostic features. Monogr Clin Cytol. 2012;21:44-54.
- Czerniak B, Woyke S, Domagala W, Krzysztolik Z. Fine needle aspiration cytology of intraocular malignant melanoma. Acta Cytol. 1983;27(2):157-165.
- Medina CA, Biscotti CV, Singh N, Singh AD. Diagnostic cytologic features of uveal melanoma. Ophthalmology. 2015;122(8):1580-1584.
- McLean IW, Foster WD, Zimmerman LE, Gamel JW. Modifications of Callender’s classification of uveal melanoma at the armed forces institute of pathology. Am J Ophthalmol. 2018;195:lvi-lx.
- Biscotti CV, Singh AD. Uveal metastases. Monogr Clin Cytol. 2012;21:17-30.
- Konstantinidis L, Damato B. Intraocular metastases--a review. Asia Pac J Ophthalmol (Phila). 2017;6(2):208-214.
- Shields CL, Shields JA, Gross NE, Schwartz GP, Lally SE. Survey of 520 eyes with uveal metastases. Ophthalmology. 1997;104(8):1265-1276.
- Mulay K, Narula R, Honavar SG. Primary vitreoretinal lymphoma. Indian J Ophthalmol. 2015;63(3):180-186.
- Eide N, Walaas L. Fine-needle aspiration biopsy and other biopsies in suspected intraocular malignant disease: a review. Acta Ophthalmol. 2009;87(6):588-601.
- Karcioglu ZA. Fine needle aspiration biopsy (FNAB) for retinoblastoma. Retina. 2002;22(6):707-710.
- Shields JA, Shields CL, Ehya H, Eagle RC Jr, De Potter P. Fine-needle aspiration biopsy of suspected intraocular tumors. The 1992 Urwick Lecture. Ophthalmology. 1993;100(11):1677-1684.
- Decaussin M, Boran MD, Salle M, Grange JD, Patricot LM, Thivolet-Bejui F. Cytological aspiration of intraocular retinoblastoma in an 11-year-old boy. Diagn Cytopathol. 1998;19(3):190-193.
- Babu N, Dey P. Medulloepithelioma of ciliary body diagnosed by fine needle aspiration cytology. Cytopathology. 2003;14(2):93-94.
- Singh AD, Medina CA, Singh N, Aronow ME, Biscotti CV, Triozzi PL. Fine-needle aspiration biopsy of uveal melanoma: outcomes and complications. Br J Ophthalmol. 2016;100(4):456-462.
- Cohen VM, Dinakaran S, Parsons MA, Rennie IG. Transvitreal fine needle aspiration biopsy: the influence of intraocular lesion size on diagnostic biopsy result. Eye (Lond). 2001;15(Pt 2):143-147.
- Faulkner-Jones BE, Foster WJ, Harbour JW, Smith ME, Davila RM. Fine needle aspiration biopsy with adjunct immunohistochemistry in intraocular tumor management. Acta Cytol. 2005;49(3):297-308.
- McCannel TA, Chang MY, Burgess BL. Multi-year follow-up of fine-needle aspiration biopsy in choroidal melanoma. Ophthalmology. 2012;119(3):606-610.
- Karcioglu ZA, Gordon RA, Karcioglu GL. Tumor seeding in ocular fine needle aspiration biopsy. Ophthalmology. 1985;92(12):1763-1767.
- Glasgow BJ, Brown HH, Zargoza AM, Foos RY. Quantitation of tumor seeding from fine needle aspiration of ocular melanomas. Am J Ophthalmol. 1988;105(5):538-546.
- Finn AP, Materin MA, Mruthyunjaya P. Choroidal tumor biopsy: a review of the current state and a glance into future techniques. Retina. 2018;38 Suppl 1:S79-s87.








