Retinopathy of prematurity (ROP) is characterized by severe retinal ischemia, vascular tortuosity and shunting, pathological angiogenesis with fibrovascular proliferation, and progressive vitreoretinal traction that may result in retinal detachment. At any time in the course of the disease, except in the event of detachment, ROP may stop or reverse itself or it may progress quite rapidly to tractional retinal detachment. Risk factors for ROP include low birth weight, young gestational age, and supplemental oxygen exposure.
While some patients receive treatment during infancy with laser photocoagulation, anti-VEGF therapy, or surgery, others may experience spontaneous regression of the retinopathy and can safely be observed. These patients, however, may be prone to vitreoretinal interface disorders and high myopia later in life that predispose them to other conditions in adulthood, such as retinal tears, vitreous hemorrhage, and rhegmatogenous retinal detachment,1,2 sometimes following cataract surgery, which often occurs earlier in these eyes.3 Using a case-based approach, we will discuss how to identify these patients prior to surgery and adjust surgical planning to maximize the chances of success.
CASE 1
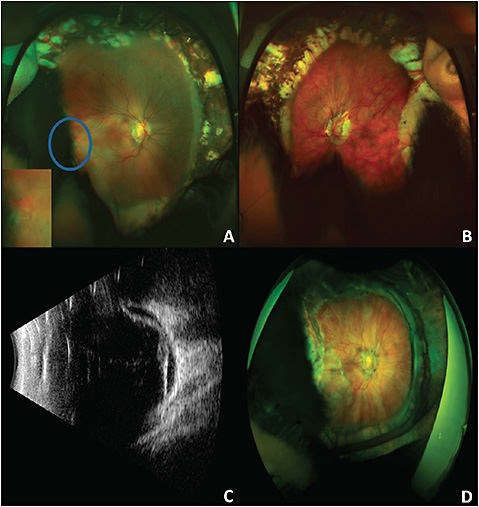
A 19-year-old woman presented with decreased vision in the right eye for 2 weeks. Her past medical history included prematurity and developmental delay. She also developed ROP, which was treated with laser photocoagulation. Visual acuity (VA) was “counting fingers” in the right eye and 20/200 in the left eye. There was horizontal nystagmus in both eyes. An anterior slit lamp exam was normal. Posterior examination showed a myopic appearing disc with peripapillary atrophy, shallow subretinal fluid within the macula and a near peripheral retinal detachment extending to a peripheral zone of 360° laser photocoagulation (Figure 1A). Examination of the fellow eye showed a myopic-appearing fundus with peripheral laser scars and no detachment (Figure 1B). An ultrasound was also performed, which showed a total retinal detachment with the temporal break previously visualized along with another break at 12 o’clock (Figure 1C). The patient underwent repair with combined pars plana vitrectomy (PPV) with scleral buckling, drainage through the preexisting break, air fluid exchange, endolaser, and instillation of 1,000 centistoke silicone oil. At postoperative month 6, the patient’s VA was “E” at 4 feet, and silicone oil removal was discussed with the family and patient, but they elected to observe (Figure 1D).
CASE 2
A 62-year-old man presented with floaters and blurred vision in the left eye. He had a history of cataract extraction in both eyes as well as laser-assisted in situ keratomileusis (LASIK) in both eyes. Visual acuity was 20/40 in the affected eye. A slit lamp examination of the anterior chamber demonstrated a LASIK flap and a well-positioned monofocal intraocular lens in the capsular bag. The vitreous was hazy with moderate hemorrhage. Indirect ophthalmoscopy revealed a myelinated nerve fiber layer along with a superonasal retinal tear and localized macula-sparing retinal detachment. He underwent PPV with drainage from the preexisting break, air fluid exchange, endolaser, and instillation of perfluoropropane (C3F8) gas. Intraoperatively, there were no complications, but the patient was noted to have an abnormal and sticky vitreoretinal interface with what appeared to be posterior insertion of the vitreous base. Postoperatively, he maintained 20/25 VA; however, he developed a small stretch hole superotemporally, which was barricaded by light laser without progression (Figure 2A). Upon further questioning, he disclosed a history of retinopathy of prematurity at birth, which resolved without treatment. A postoperative fluorescein angiography showed hyperfluorescence of the foveal avascular zone and mild avascularity of the peripheral fundus with late temporal vascular leakage (Figure 2B).

DISCUSSION
Adults with a history of ROP, independent of their prior need for treatment during infancy, are at higher risk of retinal detachment as adults. Often in cases where ROP has previously regressed, the hyaloid is more adherent, especially at the area between avascular and vascular retina. In patients with ROP, the location of the vitreous base may be displaced posteriorly, leading to more posterior retinal breaks.
Patients with a history of ROP are also more likely to have developed high myopia, which predisposes them to retinal detachment.4 The etiology of progression of myopia is unclear and may be a combination of factors including corneal steepening, decreased anterior chamber depth, increased lens thickness, and other developmental changes that may or may not be related to laser treatment.
Case 1 is illustrative of typical ROP treatment-related detachments in adulthood where the breaks localize to the border of the laser photocoagulation scars. The location of the break was quite posterior so it was difficult to get the buckle to support it directly; however, the buckle still served to release and support other more anterior traction. A vitrectomy is often necessary to address posterior pathology, but the vitreous may be difficult to remove in its entirety in this young group of patients and the buckle adds additional support to unrelieved traction.
In case 2, a history of prematurity was not obtained preoperatively and a buckle could have been useful. While this patient was older, the vitreoretinal interface was still quite abnormal and postoperative contraction led to a stretch hole which could potentially have been avoided had a buckle been added. Generally speaking, we have never regretted placing a buckle in these eyes, but we have certainly regretted not placing a buckle. In addition to using a buckle, we also prefer to use a long-acting gas and to conduct a thorough scleral-depressed vitreous shave.
Eliciting a history of prematurity prior to repair, if not clinically obvious, may enhance surgical outcomes. Subtle cases may be detected by recognizing avascular peripheral retinal, vascular straightening, or an abnormal vitreoretinal interface. When basic clinical examination is insufficient to obtain a diagnosis but offers some diagnostic clues, we recommend obtaining a widefield angiogram. Fluorescein angiograms for adult patients treated for ROP early in infancy may show a variety of vascular abnormalities including nonvascularized peripheral retina, leakage at this interface, hyperfluorescence of the foveal avascular zone, and arteriovenous shunting or vascular anastomoses.5,6
CONCLUSION
Patients who develop retinal detachment in adulthood with a history of prematurity present unique challenges to the vitreoretinal surgeon. Thorough preoperative clinical examination with adjunctive dye-based angiography may be useful in identifying peripheral pathology prior to surgery. Intraoperatively, we find combined scleral buckling with PPV, a thorough vitreous shave, and long-acting gas offer the best chance for anatomical success. RP
REFERENCES
- Ruth A, Hutchinson AK, Baker Hubbard G. Late vitreous hemorrhage in patients with regressed retinopathy of prematurity. J AAPOS. 2008;12(2):181-185.
- Kaiser RS, Trese MT, Williams GA, Cox MS Jr. Adult retinopathy of prematurity: outcomes of rhegmatogenous retinal detachments and retinal tears. Ophthalmology. 2001;108(9):1647-1653.
- Kaiser RS, Fenton GL, Tasman W, Trese MT. Adult retinopathy of prematurity: retinal complications from cataract surgery. Am J Ophthalmol. 2008;145(4):729-735.
- Geloneck MM, Chuang AZ, Clark WL, et al; and BEAT-ROP Cooperative Group. Refractive outcomes following bevacizumab monotherapy compared with conventional laser treatment: a randomized clinical trial. JAMA Ophthalmol. 2014;132(11):1327-1333.
- Cernichiaro-Espinosa LA, Williams BK Jr, Martínez-Castellanos MA, Negron CI, Berrocal AM. Peripheral vascular abnormalities seen by ultra-widefield fluorescein angiography in adults with history of prematurity: report of three cases. Ophthalmic Surg Lasers Imaging Retina. 2018;49(4):278-283.
- Lepore D, Quinn GE, Molle F, et al. Follow-up to age 4 years of treatment of type 1 retinopathy of prematurity intravitreal bevacizumab injection versus laser: fluorescein angiographic findings. Ophthalmology. 2018;125(2):218-226.








