Surgery is an ever-evolving field, driven toward achieving better outcomes with fewer complications. Therefore, it is a natural frontier for the development and application of novel technologies, designed to improve results, make procedures easier, and make the impossible a reality. Vitreoretinal surgery is a highly advanced and specialized subfield of surgery, which relies heavily on technology. For instance, although primitive forms of ocular surgery have existed for centuries, vitreoretinal surgery has only been possible for several decades.
Taking retinal detachment as an example, it was an irreversible blinding condition until the development of scleral buckling by Schepens in the 1950s.1 The technique has been refined since then, and subsequently, pars plana vitrectomy was introduced by Machemer,2 providing another surgical approach. In the past several decades, surgical techniques and instrumentation have evolved significantly, and today retinal detachments are relatively simple to treat with a very high success rate.
Over the past 2 decades, the majority of technological advances have involved instrumentation, leading to the development of small-gauge, sutureless vitrectomy systems and important intraoperative tools such as perfluorocarbon liquid, silicone oil, and a wide array of specialized instruments and cannulas. However, recent years have seen a rise in research and development of novel systems that incorporate digital technologies for the improvement of intraoperative visualization. This trend corresponds with advances made in other types of surgery, in which digital technologies are used intraoperatively for improved visualization. The purpose of this piece is to review in brief the current leading advances in this area.
INTRAOPERATIVE OCT
Optical coherence tomography (OCT) has revolutionized the practice of ophthalmology and most notably of vitreoretinal diseases. At present, it is the most commonly performed imaging modality in ophthalmology, and in many cases it guides clinical decision making regarding medical and surgical treatments.
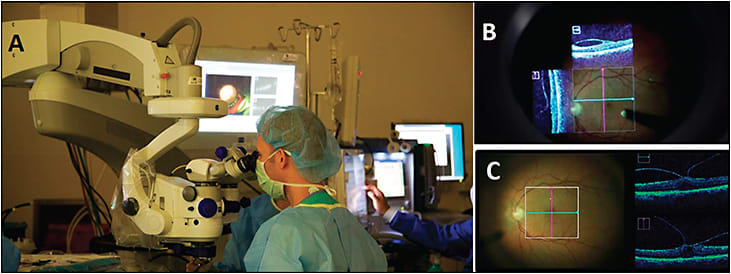
Because vitreoretinal surgery is often targeted at very small structures, such as macular holes and membranes whose size is measured in micrometers, intraoperative OCT can provide real-time feedback and aid surgeons during surgeries. In recent years, visualization systems that allow performance of intraoperative OCT have been developed, starting with portable hand-held OCT systems that could be used during surgery and, more recently, integrated systems that are part of the surgical microscope.3 Two such systems are FDA approved and commercially available: the Zeiss RESCAN 700 and the Leica Microsystems EnFocus. Such systems are controlled by the surgeon using the foot pedal and allow for real-time OCT targeted at the location of interest. The OCT scan is projected in real time and is seen by surgeons through the microscope without requiring them to turn their heads toward a monitor. This way, OCT can be performed while the surgeons are using their instruments inside the eye with no interruption of the surgical procedure (Figure 1). The intraoperative OCT can be turned on and off at the discretion of the surgeon, can be viewed by assistants and nurses on a monitor, and can be used to capture intraoperative OCT scans as single photographs or movie clips.
Several studies have reported on vitreoretinal surgeries in which intraoperative OCT was used. The DISCOVER study is a large, multisurgeon study that systematically investigated the use of intraoperative OCT, and it recently reported its 3-year results of a cohort of more than 800 surgeries.4 Notably, successful image acquisition was documented in 98% of cases. In vitreoretinal surgeries, surgeons reported that information obtained by the intraoperative OCT had altered their decision-making during surgery in 29% of cases. These results indicate the clinical utility of intraoperative OCT. To date, use of intraoperative OCT has been reported in surgeries for a wide variety of vitreoretinal disorders, such as epiretinal membranes, macular holes, vitreomacular traction, and retinal detachments.4-7
HEADS-UP DISPLAY
Another novel technology that is currently being developed is the digital heads-up display system (NGENUITY 3D Visualization System; Alcon). This technology was designed to digitally improve the visualization in vitreoretinal surgeries, and includes a high dynamic range (HDR) camera with excellent resolution, image depth, clarity, and color contrast. The surgeon is no longer required to look through the microscope but can view the surgical field in 3D (ie, without losing depth perception) on a monitor (Figure 2). It is also possible to increase magnification while maintaining a wide field of view or to digitally highlight ocular structures of interest. The majority of surgeons who evaluated this technology reported that its ergonomics were superior to those of the standard surgical microscope, and that the digital image processing and use of a large display are significant advantages.8 Heads-up display may also be used together with intraoperative OCT to combine the advantages of both technologies.9

The Clarity Bionic Visualization Platform (Beyeonics; not yet commercially available) is a novel platform that integrates advanced technology into surgical workflow to allow for enhanced visualization and a constant stream of information during surgery. The platform provides augmented reality vision that replaces surgical microscopes, allowing integration of unlimited data. The system consists of dual 3D ultra-resolution cameras suspended on a remote arm, a transparent head wearable display, and a processing core. The system allows instant integration of information from multiple digital sources in real time (such as previously acquired retinal imaging), and the surgeon has simultaneous visualization of multiple fields of view while being able to move freely (Figure 3). Using head gestures, the surgeon can control the display, shifting between different virtual screens and controlling functions such as focus, magnification, and transparency transitions. This technology holds promise to improve clinical decision-making during surgery.

CONCLUSION
Digital visualization is being actively developed toward integration in vitreoretinal surgery. It is likely that advances made in this area will facilitate vitreoretinal surgery, possibly improve its results, and change the way it is performed and taught. RP
REFERENCES
- Schepens CL, Okamura ID, Brockhurst RJ. The scleral buckling procedures. I. Surgical techniques and management. AMA Arch Ophthalmol. 1957;58(6):797-811.
- Norton EW, Machemer R. A new approach to the treatment of selected retinal detachments secondary to vitreous loss at cataract surgery. Trans Am Ophthalmol Soc. 1971;69:63-70.
- Carrasco-Zevallos OM, Viehland C, Keller B, et al. Review of intraoperative optical coherence tomography: technology and applications. Biomed Opt Express. 2017;8(3):1607-1637.
- Ehlers JP, Khan M, Petkovsek D, et al. Outcomes of intraoperative OCT-assisted epiretinal membrane surgery from the PIONEER study. Ophthalmol Retina. 2018;2(4):263-267.
- Borrelli E, Palmieri M, Aharrh-Gnama A, Ciciarelli V, Mastropasqua R, Carpineto P. Intraoperative optical coherence tomography in the full-thickness macular hole surgery with internal limiting membrane inverted flap placement. Int Ophthalmol. 2018 Mar 3 [Epub ahead of print].
- Dusova J, Hejsek L, Stepanov A, Marak J, Jirásková N. Intraoperative optical coherence tomography in vitreoretinal surgery. Cesk Slov Oftalmol. 2017;73(3):94-100.
- Ehlers JP, Han J, Petkovsek D, Kaiser PK, Singh RP, Srivastava SK. Membrane peeling-induced retinal alterations on intraoperative oct in vitreomacular interface disorders from the PIONEER study. Invest Ophthalmol Vis Sci. 2015;56(12):7324-7330.
- Eckardt C, Paulo EB. Heads-up surgery for vitreoretinal procedures: an experimental and clinical study. Retina. 2016;36(1):137-147.
- Ehlers JP, Uchida A, Srivastava SK. The integrative surgical theater: combining intraoperative optical coherence tomography and 3D digital visualization for vitreoretinal surgery in the DISCOVER study. Retina. 2018;38 Suppl 1:S88-S96.








