Corticosteroids are a mainstay for the treatment of noninfectious uveitis and associated macular edema. Local delivery methods include topical drops as well as deposition in the subtenon, intravitreal, and more recently, suprachoroidal spaces. The Uveitis Corner column in the September 2017 issue of Retinal Physician (https://www.retinalphysician.com/issues/2017/september-2017/treatment-of-uveitic-macular-edema ) provides an excellent review of these options.1
Currently, there are only 2 local steroid implant treatments approved by the FDA for noninfectious uveitis: Retisert (Bausch + Lomb), a 0.59-mg fluocinolone acetonide intravitreal surgical implant that was FDA approved in 2005, and Ozurdex (Allergan), a 0.7-mg dexamethasone intravitreal injectable implant that was FDA approved in 2010. Here we will review the latest phase 3 study results on 2 local treatments emerging on the horizon.
DURASERT
The Durasert implant (Yutiq; EyePoint Pharmaceuticals, Inc.) is a sustained-release 0.18-mg fluocinolone intravitreal implant measuring 3.5 mm in length and 0.37 mm in diameter (Figure 1). The implant can be injected in the office using a 25-gauge needle and is designed to last up to 3 years.

EyePoint Pharmaceuticals, Inc. (formerly pSivida) currently has 2 parallel phase 3 studies on Durasert for the treatment of chronic noninfectious posterior-segment uveitis. Both studies were multicenter, masked, prospective studies with patients randomized to Durasert vs sham injections with a primary endpoint of uveitis recurrence. To date, 12-month results have been published (Tables 1 and 2),2,3 and the studies expect to gather data out to 3 years.
| DURASERT GROUP | SHAM GROUP | |
|---|---|---|
| Uveitis recurrence | 37.9% | 97.6% |
| Average IOP rise | 1.3 mmHg | 0.2 mmHg |
| IOP >25 mmHg | 19.5% | 11.9% |
| Cataract surgery (phakic patients) | 3.3% | 4.8% |
| DURASERT GROUP | SHAM GROUP | |
|---|---|---|
| Uveitis recurrence | 36.6% | 71.2% |
| Average IOP rise | 2.0 mmHg | 0.0 mmHg |
| Cataract surgery (phakic patients) | 18.0% | 8.6% |
Both studies show the implant significantly reduced uveitis occurrences over 12 months by at least half. In PSV-FAi-001, a higher proportion of patients in the sham group required additional therapy for inflammation control. Implant-treated patients had better visual acuity than the sham group prior to local injections.4,5 Regarding intraocular pressure (IOP), in the first study the percentage of patients requiring IOP-lowering medications or surgeries was not different between the 2 groups. In the second study, the percentage of patients requiring IOP-lowering therapy at any time over the first 12 months was similar between both groups (50.5% Durasert vs 51.9% sham), but 1 patient treated with Durasert required glaucoma surgery. Cataract formation was significantly higher in the Durasert-treated groups in both studies.
EyePoint Pharmaceuticals, Inc. announced in March that the FDA accepted its New Drug Application (NDA) for Durasert for 3-year treatment of noninfectious posterior-segment uveitis. The goal date for the FDA to complete its review is November 5, 2018.6
CLS-TA
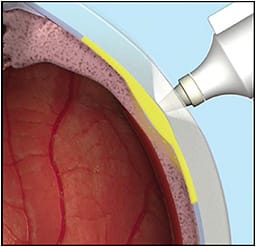
CLS-TA is a sterile, preservative-free suspension of 4-mg triamcinolone acetonide (TA) in 100 µL from Clearside Biomedical, Inc. The drug is provided with a prepackaged “microinjector” syringe, with a 30-gauge 1-mm needle (Figure 2). It is injected 4 mm posterior to the limbus into the suprachoroidal space, where it flows into posterior-segment tissues without depot at the injection site. This unique suprachoroidal route allows drug concentrations to be high at target sites posteriorly, while minimizing drug concentrations anteriorly, providing the potential for efficacy while mitigating side effects such as cataract and ocular hypertension.
Preclinical data showed that 90 days after suprachoroidal injection, the concentration of TA in the sclera, choroid, and retinal pigment epithelium is 12 times higher compared to the same TA dose injected intravitreally. Retinal concentration at 90 days was equal following suprachoroidal and intravitreal injections. In the vitreous, lens, and ciliary body, there were substantially lower concentrations of triamcinolone following suprachoroidal injection as compared to intravitreal injection. Through the 90 days after suprachoroidal injection, TA was below limits of quantification in the aqueous humor.7
Clearside Biomedical announced in March the results of the PEACHTREE phase 3 study of suprachoroidal CLS-TA in patients with macular edema arising from any noninfectious uveitis (anterior, intermediate, posterior, or panuveitis). The randomized, controlled, masked clinical trial enrolled 160 patients, with 96 patients receiving 2 doses of 4.0-mg suprachoroidal CLS-TA 12 weeks apart and 64 patients receiving sham doses 12 weeks apart. The primary endpoint was proportion of patients gaining ≥15 EDTRS letters after 24 weeks.8
This phase 3 trial met its primary endpoint with a significantly greater proportion of patients in the CLS-TA (46.9%) arm compared to those in the sham control (15.6%) arm gaining ≥15 ETDRS letters in BCVA (P<.001). The study also met its secondary endpoint: reduction of central subfield thickness. At 24 weeks, the CLS-TA arm saw a reduction in CST of 153 microns, compared to 18 microns in the sham group (P<.001). In addition, the mean gain in ETDRS letters was greater in the CLS-TA arm compared to sham. Treated subjects gained 9.6 letters at 4 weeks, and 13.8 letters at 24 weeks, compared to 1.3 letters and 3.0 letters for the sham group, respectively.8
There were no treatment-related serious adverse events in this trial. At 24 weeks, 11.5% of patients receiving CLS-TA had an adverse event related to elevated IOP. No patients in the sham group had an elevated IOP adverse event, excluding those who required corticosteroid rescue. Cataract formation was similar between the CLS-TA and sham groups, with no cataract-related surgeries in either group at 6 months.8 Clearside Biomedical expects to file an NDA for CLS-TA with the FDA in the fourth quarter of 2018.
CONCLUSIONS
With prolonged drug-delivery systems, improved target-tissue localization, and lower rates of ocular adverse events, local corticosteroids will become increasingly effective and attractive treatment choices for uveitis. New devices on the market will offer more options to manage this chronic disease before advancing to oral steroids or immunologic treatments. We anticipate the addition of 2 new treatments to our armamentarium as Durasert and CLS-TA both progress through the FDA registration process this year. RP
REFERENCES
- Hassman L, Bessette A, Kuriyan AE. Treatment of uveitic macular edema. Retin Physician. 2017;14(7): 34-36,38,57.
- Nguyen QD, Patel K, Paggiarino D. Controlling posterior segment uveitic recurrences: results from a phase 3 study of fluocinolone acetonide intravitreal insert (FAI) in subjects with chronic non-infectious uveitis affecting the posterior segment. Presented at: the 2018 ARVO Annual Meeting; April 29-May 3, 2018; Honolulu, Hawaii.
- EyePoint Pharmaceuticals. pSivida’s second phase 3 study for Durasert three-year treatment for posterior segment uveitis maintains positive efficacy and safety profile at 12 months [press release]. February 7, 2018.
- Srivastava S. injectable fluocinolone acetonide intravitreal insert reduces the need for adjunctive treatment in noninfectious posterior segment uveitis. Presented at: the 2018 ASRS Annual Meeting; July 25, 2018; Vancouver, British Columbia.
- Hariprasad SM. Effect of a 0.18mg Sustained Release Injectable Intravitreal Fluocinolone Acetonide Insert on Macular Edema in Patients with Posterior Segment Uveitis. Presented at: the 51st Annual Retina Society Scientific Meeting; September 14th, 2018. San Francisco, California.
- pSivida Announces FDA acceptance for filing of new drug application (NDA) for Durasert three-year treatment for posterior segment uveitis [press release]. March 19, 2018.
- Clearside Biomedical. Data on file. April 2018.
- Yeh S. Suprachoroidally injected CLS-TA improves visual acuity and macular edema in noninfectious uveitis: results of the phase 3 PEACHTREE study. Presented at: the 2018 ASRS National Meeting; July 25, 2018; Vancouver, British Columbia.








