Posterior dislocation of lens fragments into the vitreous (“dropped lens”) is a fairly uncommon complication of cataract surgery with an incidence of approximately 0.2% to 1.5% depending on surgeon experience,1 but it can be sight threatening due to severe intraocular inflammation causing secondary glaucoma, corneal edema, cystoid macular edema (CME), and retinal detachment.2 Proper management both intraoperatively and postoperatively is essential to reducing the risk of these complications. Furthermore, retained lens fragments are associated with malpractice claims and, in cases with greater visual acuity decline, greater likelihood of indemnity payments.3
INITIAL APPROACH
Early recognition of a dropped lens is critical to prevent further problems. While there are series demonstrating adequate results with posterior levitation techniques, in general, the cataract surgeon should avoid retrieving lens fragments that descend beyond the posterior capsule, as this can create vitreoretinal traction and cause small retinal breaks, giant retinal tears, and retinal detachment.4 Instead, the cataract surgeon should generally focus on stabilizing the anterior chamber.
Michael J. Venincasa, BS, is a medical student at the University of Miami Miller School of Medicine in Miami, Florida. Jayanth Sridhar, MD, is assistant professor of clinical ophthalmology and vitreoretinal surgery, and Rahul Tonk, MD, is an assistant professor of ophthalmology at Bascom Palmer Eye Institute, University of Miami Miller School of Medicine in Miami, Florida. Mr. Venincasa reports no related disclosures. Dr. Sridhar reports personal fees from Alimera Science. Dr. Tonk reports no related disclosures. Reach Dr. Sridhar at jsridhar1@med.miami.edu.
Editor’s note: This article is featured in a journal club episode of Straight From the Cutter’s Mouth: A Retina Podcast. Listen to the episode at www.retinapodcast.com .
DEALING WITH THE ANTERIOR CHAMBER
Reducing complications associated with posteriorly dislocated lens fragments begins with the anterior-segment surgeon. Once posterior capsular rupture and vitreous prolapse have been identified, the anterior-segment surgeon should not instinctively withdraw the phacoemulsification probe from the main corneal incision. Instead, the irrigation or bottle height level should be decreased, the second instrument should be withdrawn from the paracentesis wound, and a viscoelastic agent should be injected to tamponade the vitreous in the area of capsular rupture. Removing the phacoemulsification probe without utilizing viscoelastic tamponade may result in further anterior migration of vitreous and incarceration of vitreous in the corneal wound, increasing the risk of retinal tear. Similarly, it is hazardous to proceed with phacoemulsification in this scenario; the phacoemulsification tip is at high risk of aspirating and dragging vitreous, leading to vitreoretinal traction and a possible retinal tear or retinal detachment.5
Once the rupture has been successfully tamponaded, the phacoemulsification probe may be withdrawn, and the surgeon can reassess the situation. If at this point posteriorly retained lens material is known or suspected, the cataract surgeon’s goal should be to close the main surgical wound and remove as much anterior vitreous as possible. 10-0 Nylon suture can be placed through the main cataract wound to provide a stable anterior chamber.
Bimanual anterior vitrectomy can then be performed through 2 separate limbal incisions or with an anterior infusion and 1 port through the pars plana. With the latter technique, the vitrector is introduced through the pars plana via a trocar or small sclerotomy.6 This technique has been advocated as maintaining an anterior-to-posterior pressure relationship that may limit further vitreous prolapse. If a transconjunctival, sutureless trocar was not used, the sclerotomy and conjunctival peritomy are typically closed using absorbable sutures. Preservative-free triamcinolone acetonide may be useful to stain the vitreous and ensure that the anterior segment and all surgical wounds are clean by the conclusion of the vitrectomy.
Once the anterior chamber is free of prolapsed vitreous, any smaller nuclear or epinuclear fragments still available anterior to the posterior lens capsule may be carefully removed (Figure 1). Dispersive viscoelastic can be used to bring fragments into the iris plane. This viscoelastic can be injected through a limbal incision or through the pars plana (posterior assisted levitation [PAL]).7 In general, the cataract surgeon may wish to avoid mechanical PAL with a spatula or other device, as such maneuvers may inadvertently cause further retinal traction.

Once the lens fragments are at or above the iris plane, the surgeon can consider employing a Sheet’s glide or intraocular lens (IOL) scaffold technique8 to prevent further posterior lens displacement or vitreous prolapse while the fragments are aspirated. Manual extraction may be preferred for larger lens fragments for situations in which phacoemulsification may worsen posterior displacement and cause increased vitreoretinal traction.
At this point, an IOL may be inserted at the surgeon’s discretion as long as the anterior chamber is stable.2,5 If there are any questions about the status of the eye, it may be preferable to defer lens placement for the future rather than potentially cause vitreous traction or worsen corneal edema.
The quantity, size, and location of any posteriorly dislocated lens fragments should be noted. Because each patient will have a different extent of vitreous liquefaction, it is important to identify where fragments have stopped their descent in the posterior chamber.4
The surgeon should ensure that all wounds are watertight prior to exiting the operating room and should counsel the patient appropriately postoperatively. While there may be an inclination to try to arrange same-day pars plana vitrectomy (PPV) to remove retained lens material, this may not be feasible in all practice environments. Visualization for the retinal surgeon may also be initially poor due to corneal edema. As such, it may preferable to wait for edema and inflammation to decrease with medical therapy prior to PPV. In fact, a large retrospective series reported no difference in visual acuity outcomes and complication rates between same-day and deferred PPV.9 Still, the patient should be referred early to a vitreoretinal surgeon for evaluation, because early removal of lens material limits intraocular inflammation and reduces the risk of uveitis, CME, and glaucoma.10 In this particular study, other independent risk factors for worse visual prognosis included pre-existing eye disease, phacoemulsification of lens particles located in the posterior chamber, and retinal detachment.
INITIAL CONSIDERATIONS FOR THE VITREORETINAL SURGEON
How should this case progress now in the hands of the vitreoretinal surgeon? Initial evaluation should focus on signs of intraocular inflammation, infection, and increased IOP. Remember that peaked corectopia can suggest anterior vitreous incarceration, requiring either close follow-up or surgical intervention to prevent sight-threatening complications.11
The first important consideration is the amount and type of retained lens material. Lens nucleus is usually less tolerated than lens epinucleus, which in turn is less tolerated than lens cortex. One rule of thumb is that lens fragments smaller than 2 mm may resolve on their own, and the physician can consider medical management with topical corticosteroids and glaucoma treatment as needed for these pieces.4 Larger fragments generally require surgical intervention.
The mainstay for treatment of significant retained lens material is complete vitrectomy using a 3-port pars plana approach to reduce inflammation, to repair possible retinal detachment, and to restore visual acuity.5 Timing of surgery, as noted previously, varies case by case. In some cases, it may be preferable to treat the patient aggressively with topical steroids with or without aqueous suppressants to reduce corneal edema, inflammation, and fluctuation in the IOP prior to undertaking a secondary surgery. In cases in which retained lens material is abutting the cornea, IOP is uncontrolled with medical management, or early retinal detachment is noted on clinical examination or ultrasonography, the surgeon may not have the luxury of waiting to pursue a PPV (Figure 2).

SURGICAL TECHNIQUE
Pars plana vitrectomy for retained lens material begins with a thorough anterior (if needed for visualization) and posterior core vitrectomy to release any vitreous adhesions around the lens and retinal surface. Preservative-free triamcinolone can be utilized to facilitate visualization and complete removal of vitreous strands. It is the authors’ opinion that a posterior vitreous detachment should be induced if not already present to reduce risk of postoperative retinal tears, although occasionally a large complete crystalline lens atop the posterior hyaloid may make induction technically more difficult. The retinal surgeon should avoid the temptation to pursue lens material with aspiration before complete removal of the core vitreous, as vitreous may become incarcerated and induce retinal breaks. The surgeon may choose to employ a 20-, 23-, 25-, or 27-gauge system for PPV, bearing in mind that smaller-gauge cutters are more likely to encounter difficulty in the removal of larger lens nuclear fragments without the assistance of a fragmatome or phacoemulsification probe.
Once the core vitreous has been cleared, as well as peripheral vitreous around the ports, attention is directed to removal of the lens material. Especially when the lens fragment is located near the macula, perfluorocarbon liquid (PFCL) may be used to float the lens away from the retina to protect the macula from vitrector or fragmatome manipulation of the fragment.5 If utilized, it is essential to ensure complete removal of all PFCL prior to closure to prevent ocular toxicity. If PFCL is not used, and manipulation must occur at the posterior pole, the surgeon should rotate the globe such that macular contact during phacoemulsification is minimal.4
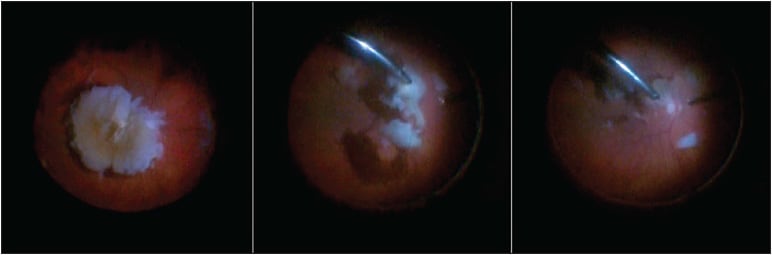
The surgeon may assess the fragment and decide that the vitreous cutter is adequate for efficient removal of smaller nuclear, epinuclear, and cortical pieces. In cases with larger nuclear fragments, more efficient removal can be undertaken, utilizing either a 19-gauge fragmatome or a phacoemulsification probe (Figure 3).12 Either of the superior ports can be removed, or a separate, fourth sclerotomy can be created. A local conjunctival peritomy is created, wet-field cautery can be applied as needed for scleral hemostasis, and a 20-gauge microincisional vitreoretinal blade is utilized to create a 19-gauge sclerotomy.
Once again, it is critical to ensure that the area chosen for creation of this sclerotomy is cleaned of vitreous gel prior to this step to avoid vitreous dragging and potential retinal breaks. Also, whether utilizing the phacoemulsification probe or the fragmatome, the surgeon must remember that the bore of the ultrasound instrument is larger than the infusion line, especially when employing a small-gauge vitrectomy platform. This difference in size can result in the aspiration “outrunning” the infusion line when the tip of the phacoemulsification instrument is not engaged with lens material and collapse of the vitreous cavity and potential iatrogenic trauma.
Occasionally, very dense nuclear fragments may be removed using manual extraction. Once a fragment is brought into the midvitreous using suction, a short burst of ultrasound energy can be used to embed the fragment onto the tip of the fragmatome and transfer it into the anterior chamber. Harder nuclei can then be removed via extracapsular extraction by extending a corneal incision or creation of a scleral tunnel.13
SMALL-GAUGE INSTRUMENTATION
As mentioned previously, although the conventional 20-gauge system can be used for lens fragment removal, many surgeons have been moving toward smaller-gauge instrumentation to reduce operative and healing times, postoperative discomfort, and refractive changes.5 Early 25-gauge instrumentation improved these metrics but differed in tactile flexibility from the 20-gauge instrumentation that surgeons to which were accustomed.
As a result, 23-gauge instruments were developed and became the preference of an increasing number of vitreoretinal surgeons,4,5 as they were shown to be safe and effective for this use.14 There are now stiffer 25-gauge and newer 27-gauge instruments available as well.
Although the 23-gauge cutting probe can remove smaller fragments without much nuclear material when at relatively lower cut rates and higher vacuum settings (often referred to as a “dense” or “momentary vitrectomy” setting), a disadvantage to this instrumentation is the inevitably lower infusion and aspiration rate5 and the inability to remove some large, hard lens fragments (the smaller-gauge cutting probe can be more easily blocked by lens material).14
Because no 23-gauge phacofragmatome is currently available for use, many surgeons choose to enlarge the 23-gauge sclerotomy port to accommodate a 20-gauge phacofragmatome when such difficult lens fragments are encountered, avoiding the need for an additional incision during the procedure. It is important to re-emphasize that use of the larger-gauge phacofragmatome with smaller-gauge vitrectomy systems requires higher infusion pressures and flow rates that can lead to hypotony and more vitreal traction.
ALTERNATIVE TECHNIQUES
Alternatively, Watanabe and colleagues reported successful retrieval of a dislocated lens without using PPV.15 A transcorneal vitrectomy was performed through the same incision as the cataract surgery using a 23-gauge anterior-segment maintainer, vitreous cutter, and light guide. In this case, the nucleus was removed via phacoemulsification and aspiration, but prior studies have shown that nuclear fragments less than one-half the size of the lens can be crushed with a light pipe and vitreous cutter16 and that nuclear fragments less than one-quarter the size of the lens can be removed through the sclerocorneal incision of the cataract surgery.17 This method allowed for safe removal of the dropped lens with an excellent postoperative course, but the downside was that manipulation near the cornea led to distortion that made for difficult visualization of the posterior eye.15
Finally, a number of devices have been developed to assist in the retrieval of the dislocated lens. One such device was created to address concerns of the cyclodialysis spatula being unable to stabilize multiple fragments or the fragment falling off the side of the narrow instrument. Called the Sabet Lenticular Safety Net (Katena Products), this device opens into a radially expanding set of wires that create a plane, rather than a single rod, to support the fragments and to perform phacoemulsification.18 Since one of the surgeon’s hands will be needed to hold the device in place, a single-port vitrectomy must be used, and this vitrectomy can be carefully performed posteriorly as the device keeps the fragments from falling posteriorly. Other surgeons have described use of a “frag bag” nitinol retractable basket.19 Originally used for cystoscopic removal of kidney stones, this instrument can fit through a 23-gauge port and can be used to stabilize large nuclear pieces in the midvitreous for removal with the vitreous cutter alone.
SECONDARY IOL OPTIONS
Following lens fragment removal, the surgeon has a number of options for secondary IOL placement if necessary.20 A sulcus 3-piece acrylic IOL is preferred by the authors if good ciliary sulcus support is present and verified after inflation with viscoelastic and inspection of the anterior capsule. In the absence of adequate sulcus support, options include anterior-chamber IOLs (ACIOLs), iris-sutured IOLs, scleral-sutured IOLs (SSIOLs), and sutureless scleral-fixated IOLs (SFIOLs).
Recent open-loop ACIOLs have demonstrated good visual outcomes with reduced risk of the angle involvement that plagued early, closed-loop ACIOLs. Iris fixation can be performed with both ACIOLs and posterior-chamber IOLs (PCIOLs), but they carry a risk of ocular hypertension secondary to pupillary block. SSIOLs are more surgically complex to place than ACIOLs, but they provide a stability less dependent on anterior-segment anatomy. The Akreos IOL (Alcon) and CZ70BD (Bausch + Lomb) utilize 4-point fixation that allows for accurate placement and possibly superior fixation compared to 2-point options. The Akreos IOL has the advantage over the CZ70BD of being a foldable IOL that can be inserted through a smaller corneal incision. One consideration for the Akreos IOL is that it is hydrophilic and may irreversibly opacify after exposure to gas tamponade.21 Use of a Hoffman pocket with SSIOLs allows the surgeon to accomplish scleral fixation with minimal conjunctival dissection and scleral cauterization.22 Complications may be further reduced with the use of Gore-Tex, which is gaining preference over Prolene due to a lower incidence of suture hydrolysis and breakage (thereby reducing infection and lens subluxation).
SFIOLs are also gaining popularity because they eliminate complications related to suture material. After 2 peritomies and partial-thickness scleral flaps are made at the 3 and 9 o’clock positions, a sclerotomy is performed near the ciliary sulcus for insertion of the IOL; the haptics are placed into the scleral flaps, and the surgical wounds are closed using tissue adhesive and glue. Prenner et al expanded on this technique by taking advantage of the instrumentation and skill set of the posterior-segment surgeon to complete ciliary sulcus-based scleral fixation without the use of scleral flaps or fibrin glue.22 Yamane et al demonstrated a similar procedure, which they termed “flanged IOL fixation,” utilizing a flange at the end of the haptic for firm fixation without using sutures or glue.23
IOL decisions should be made on a case-by-case basis. While sulcus IOLs are preferred, if tears or detachment is encountered during vitrectomy, and air or gas tamponade is employed, there is a risk of haptic or whole IOL displacement anteriorly with poor postoperative positioning. ACIOLs and iris-fixated PCIOLs should generally be avoided in individuals with anterior-chamber pathology or corneal disease or in eyes at risk for ocular hypertension.21 It may be preferable to avoid utilizing SSIOLs and SFIOLs in patients with conjunctival or scleral thinning due to increased risk of erosion and exposure of sutures or haptics, respectively. These latter 2 techniques may also be more time consuming and could expose patients to longer operative times.
PATIENT OUTCOMES
When referred early, most eyes with retained lens fragments generally do well with good recovery of vision post vitrectomy.2 in 2003, Smiddy et al reported a retinal detachment rate of 8% and final visual acuity of 20/40 or better in 54% of eyes undergoing PPV for this purpose.24 These outcomes emphasize the importance of early recognition and referral.
FOLLOW-UP
Patients should be closely followed for signs of inflammation, elevated IOP, and retinal tears or detachment.5 Optical coherence tomography can be considered at the 4-week follow-up visit to check for CME. If CME is present, it should be treated aggressively with an escalating regiment of topical nonsteroidal anti-inflammatory medications and intravitreal or sub-Tenon corticosteroid injections. Persistent CME despite adequate therapy should lead the surgeon to consider the possibility of retained lens material in the angle or posterior segment or continued vitreous incarceration in one of the corneal wounds.4,5
CONCLUSION
Posterior dislocation of lens fragments is a rare but serious complication of cataract surgery. With early recognition, careful planning, and meticulous surgical techniques, both at the time of cataract surgery and in possible subsequent retinal procedures, outcomes can be excellent following fragment removal. RP
REFERENCES
- Salehi A, Razmju H, Beni AN, Beni ZN. Visual outcome of early and late pars plana vitrectomy in patients with dropped nucleus during phacoemulsification. J Res Med Sci. 2011;16:1422-1429.
- Olokoba L, Islam T, Nahar N, Mahmoud A, Olokoba A. A 3-year review of the outcome of pars plana vitrectomy for dropped lens fragments after cataract surgery in a tertiary eye hospital in Dhaka, Bangladesh. Ethiop J Health Sci. 2017;27:427-432.
- Kim JE, Weber P, Szabo A. Medical malpractice claims related to cataract surgery complicated by retained lens fragments (an American Ophthalmological Society thesis). Trans Am Ophthalmol Soc. 2012;110:94-116.
- Villegas VM, Gold AS, Wildner A, Ehlies F, Murray TG. Retinal management of dropped lens as a complication of phacoemulsification. Retin Physician. 2014;11(3):44-47.
- Nagpal M, Jain P. Dropped lens fragment, dislocated intraocular lens. Dev Ophthalmol. 2014;54:234-242.
- Arbisser LB, Charles S, Howcroft M, Werner L. Management of vitreous loss and dropped nucleus during cataract surgery. Ophthalmol Clin North Am. 2006;19:495-506.
- Chang DF, Packard RB. Posterior assisted levitation for nucleus retrieval using Viscoat after posterior capsule rupture. J Cataract Refract Surg. 2003;29:1860-1865.
- Kumar DA, Agarwal A, Prakash G, Jacob S, Agarwal A, Sivagnanam S. IOL scaffold technique for posterior capsule rupture. J Refract Surg. 2012;28:314-315.
- Modi YS, Epstein A, Smiddy WE, Murray TG, Feuer W, Flynn HW Jr. Retained lens fragments after cataract surgery: outcomes of same-day versus later pars plana vitrectomy. Am J Ophthalmol. 2013;156:454-9.
- Scupola A, Abed E, Sammarco MG, et al. 25-gauge pars plana vitrectomy for retained lens fragments in complicated cataract surgery. Ophthalmologica. 2015;234:101-108.
- Vien L, Yang D. Anterior vitreous incarceration after phacoemulsification cataract extraction imaged with spectral-domain optical coherence tomography. Optometry: Open Access. 2015;1:101.
- Chiang A, Garg SJ, Alshareef RA, et al. Removal of posterior segment retained lens material using the OZil phacoemulsification handpiece versus fragmatome during pars plana vitrectomy. Retina. 2012;32:2119-2126.
- Agarwal A. Management of Phaco Complications: Newer Techniques. Philadelphia, PA; JP Medical Ltd; 2014.
- Koh KM, Kim HS, Cho HJ, et al. Surgical outcomes of 23-gauge vitrectomy for the management of lens fragments dropped into the vitreous cavity during cataract surgery. Saudi J Ophthalmol. 2014;28:253-256.
- Watanabe A, Gekka T, Tsuneoka H. Treatment of a dislocated lens by transcorneal vitrectomy and bimanual phacoemulsification. Clin Ophthalmol. 2014;8:1539-1542.
- Wang ZY, Zhao K, Li JK, Biswal M, Zhao PQ. Immediate corneal vitrectomy for posteriorly dislocated lens fragments during cataract surgery. Retina. 2013;33:1715-1719.
- Nakasato H, Uemoto R, Kawagoe T, Okada E, Mizuki N. Immediate removal of posteriorly dislocated lens fragments through sclerocorneal incision during cataract surgery. Br J Ophthalmol. 2012;96:1058-1062.
- Sabet SJ. Managing a dropped lens during phaco. Ophthalmol Manag. 2008;10(8).
- Berry DE, Walter SD, Fekrat S. A frag bag for efficient removal of dislocated nuclear material. Ophthalmic Surg Lasers Imaging Retina. 2017;48:1006-1008.
- Sieber M, Sridhar J. Secondary intraocular lenses by the retinal surgeon: from sclerotomies to sutures. Curr Ophthalmol Rep. 2017;5:169-175.
- Kalevar A, Dollin M, Gupta RR. Opacification of scleral-sutured Akreos AO60 intraocular lens after vitrectomy with gas tamponade: case series. Retin Cases Brief Rep. 2017 Sep 27. [Epub ahead of print]
- Prenner JL, Feiner L, Wheatley HM, Connors D. A novel approach for posterior chamber intraocular lens placement or rescue via a sutureless scleral fixation technique. Retina. 2012;32:853-855.
- Yamane S, Sato S, Maruyama-Inoue M, Kadonosono K. Flanged intrascleral intraocular lens fixation with double-needle technique. Ophthalmology. 2017;124:1136-1142.
- Smiddy WE, Guererro JL, Pinto R, Feuer W. Retinal detachment rate after vitrectomy for retained lens material after phacoemulsification. Am J Ophthalmol. 2003;135:183-187.








