When contemplating intraocular lens (IOL) placement in a patient in need of an IOL following a pars plana vitrectomy, a surgeon may choose among a host of options, including placement of an anterior chamber IOL (ACIOL) or a posterior chamber intraocular lens (PCIOL) with or without suture fixation. Each has its own set of advantages and disadvantages; unfortunately, no randomized controlled trial exists to guide selection. ACIOL placement, which is faster and simpler to perform than secondary fixation of a PCIOL, unfortunately may increase the risk of corneal decompensation, glaucoma, and uveitis.1-4
To avoid these issues, techniques for secondary posterior IOL and IOL rescue using intrascleral haptic fixation were described in 1997 by Maggi and Maggi.5 The techniques were made more user friendly by Gabor and Pavlidis in 20076 and Scharioth et al in 2010.7 The technique was modified by others to accommodate smaller gauge pars plana vitrectomy techniques.8-10 Because the technique doesn’t include suture fixation, concern may exist regarding dislocation of these lenses.
A suture-fixated posterior-chamber IOL may lessen, but not eliminate, dislocation concern, because Prolene retention sutures may degrade and rupture over time.11 These concerns about Prolene sutures may be avoided by utilizing nonabsorbable monofilament 7-0 CV-8 Gore-Tex retention suture material (W. L. Gore and Associates), which has great resistance to rupture.12 Two acrylic Bausch + Lomb IOLs with “eyelets” are popular for suture fixation: the hydrophilic (therefore prone to opacification with gas contact) Akreos AO-60 and the hydrophobic enVista MX60. Some may favor larger IOLs (for example Alcon CZ70BD, with a 7.0-mm rather than a 6.0-mm optic) to minimize decentration and glare in those with pupillary abnormalities and to stabilize the iris to minimize iris mobility, mitigating iritis.13
Regarding IOL exchange after pars plana vitrectomy, unique considerations are appropriate: extracting the IOL to be replaced through a large corneal or scleral wound can be associated with corneal trauma, significant astigmatism, intraocular bleeding, ocular structure collapse, and suprachoroidal hemorrhage.
There are several considerations and options, which continue to evolve! We are fortunate this month to have the experienced viewpoints of Alex Melamud, MD, MA, of The Retina Group of Washington, and Omesh Gupta, MD, MBA, of the Retina Service, Wills Eye Hospital/Mid Atlantic Retina.
Michael Colucciello, MD, is a partner at South Jersey Eye Physicians and a clinical associate at the University of Pennsylvania/Scheie Eye Institute. He is a member of the Retina Society and the American Society of Retina Specialists. Alex Melamud, MD, is a vitreoretinal specialist at The Retina Group of Washington in Washington, DC. Omesh Gupta, MD, MBA, is a vitreoretinal specialist at Wills Eye Hospital/Mid Atlantic Retina in Philadelphia, Pennsylvania. The authors report no related financial disclosures.
REFERENCES
- Dick HB, Augustin AJ. Lens implant selection with absence of capsular support. Curr Opin Ophthalmol. 2001;12:47-57.
- Auffarth GU, Wesendahl TA, Brown SJ, et al. Are there acceptable anterior chamber intraocular lenses for clinical use in the 1990s? An analysis of 4104 explanted anterior chamber intraocular lenses. Ophthalmology. 1994;101:1913-1922.
- Ellerton CR, Rattigan SM, Chapman FM, et al. Secondary implantation of open-loop, flexible, anterior chamber intraocular lenses. J Cataract Refract Surg. 1996;22:951-954.
- Hennig A, Evans JR, Pradhan D, et al. Randomised controlled trial of anterior-chamber intraocular lenses. Lancet (London). 1997;349:1129-1133.
- Maggi R, Maggi C. Sutureless scleral fixation of intraocular lenses. J Cataract Refract Surg. 1997;23:1289-1294.
- Gabor SG, Pavlidis MM. Sutureless intrascleral posterior chamber intraocular lens fixation. J Cataract Refract Surg. 2007;33:1851-1854.
- Scharioth GB, Prasad S, Georgalas I, et al. Intermediate results of sutureless intrascleral posterior chamber intraocular lens fixation. J Cataract Refract Surg. 2010;36:254-259.
- Prenner JL, Feiner L, Wheatley HM, et al. A novel approach for posterior chamber intraocular lens placement or rescue via a sutureless scleral fixation technique. Retina. 2012;32:853-855.
- Prasad S. Transconjunctival sutureless haptic fixation of posterior chamber IOL: a minimally traumatic approach for IOL rescue or secondary implantation. Retina. 2013;33:657-660.
- Feistmann JA, Prasad S, Gentile RC et al. Bimanual intraocular lens rescue with transconjunctival scleral fixation. Retina. 2014;34:812-815.
- Wagoner MD, Cox TA, Ariyasu RG, et al. American Academy of Ophthalmology. Intraocular lens implantation in the absence of capsular support: a report by the American Academy of Ophthalmology. Ophthalmology. 2003;110:840-859.
- David TE, Armstrong S, Sun Z. Replacement of chordae tendineae with Gore-Tex sutures: a ten-year experience. J Heart Valve Dis. 1996;5:352-355.
- Mantopoulos D, Vloka CN, Halperin SJ, et al. Novel surgical approach for fixation of a posterior chamber intraocular lens using Gore-Tex suture. Retina. 2017;37:2362-2364.tions. Ophthalmology. 2001;108:1485-1492.
Comments from Alex Melamud MD, MA, The Retina Group of Washington:
When presented with an aphakic patient in the setting of a dislocated intraocular lens (IOL) or status post complex cataract surgery or trauma, today’s vitreoretinal specialist has an increasing array of options for surgical management. Vitrectomy surgery is performed routinely to address posterior segment pathology. In the absence of capsular support, IOLs are commonly placed in the anterior chamber or the sulcus (SFIOL).
Which of these surgical techniques is best? Although numerous studies exist describing excellent outcomes with any individual technique, in our recent review of the literature we found few studies that systematically compared visual outcomes or surgical complication rates of the different approaches. To answer this question in our practice, we performed a retrospective review of 57 eyes that underwent pars plana vitrectomy with placement of either an anterior chamber or sulcus sutured intraocular lens implant.1
Anterior-chamber IOL placement is the traditional approach. In the 1990s, flexible, open-loop ACIOLs were developed that minimized some of the complications traditionally associated with these lenses, such as uveitis, glaucoma, hyphema, and cystoid macular edema. In this method, the IOL is ideally placed in the iridocorneal angle with the footplates in contact with the scleral spur. In our review, we included 33 eyes with ACIOL placement using the Alcon series MTA-U0 single-piece polymethyl methacrylate (PMMA) lenses.
Sulcus-fixated IOLs are a newer and more heterogeneous category with numerous techniques described and others continuing to evolve. In our review, we included 24 eyes with the Alcon CZ70BD one-piece PMMA IOL.
Our study looked at visual outcomes and complication rates between the 2 groups. At a median of 13.2 months follow-up, we found that the visual outcomes in both groups were statistically similar. Moreover, we found no differences in the rates of postoperative inflammation, elevated intraocular pressure, vitreous hemorrhage, corneal edema or cystoid macular edema. Unusually, it appeared that the ACIOL group was more likely to develop postoperative epiretinal membrane.
What should the surgeon take away from these findings? Our study concluded that because both surgical techniques offered similar visual outcomes the decision of which surgery to use should continue to fall on physician and patient preference. Arguments for using SFIOLs include greater success in younger patients and in patients with preexisting corneal pathology, diabetes, cystoid macular edema, and glaucoma. It should be noted, however, that SFIOL surgery is a more complex procedure overall, with a steeper learning curve. Further, it has been debated that some SFIOL techniques may predispose to post-operative hypotony and hemorrhage. Arguments for ACIOL use include faster surgical time, better outcomes in older patients and in patients with bleeding disorders or extensive conjunctival scarring, and decreased risk for iatrogenic suture breaks. Many also argue, conversely, that ACIOL surgery results in increased endothelial cell count losses, a substantial shortcoming for the procedure. However, this point is under debate, with some research pointing to surgical trauma in general resulting in the endothelial cell count losses rather than specifically the implanted ACIOL.
In my own practice, I continue to use both the ACIOL technique and the SFIOL technique. I have used a number of the SFIOL techniques, including the trans-scleral haptic fixation, IOL fixation using Hoffmann scleral pockets, fixating the CZ70BD with Prolene suture, and fixating the foldable Akreos IOL with Gore-Tex suture.
When choosing the lens, I am mindful of the patient’s history and comorbidities. I avoid ACIOLs in patients with glaucoma, although this isn’t an absolute contraindication. I tend to prefer smaller-incision foldable IOLs for sulcus fixation to minimize the size of the surgical wound. On the other hand, in patients who are on anticoagulation, or with other risk factors for suprachoroidal hemorrhage, I tend to prefer the ACIOL lenses because of the relative speed of the procedure and because of some of the reports of postoperative hypotony and vitreous hemorrhage that have been associated with SFIOL.
In the end, any technique for secondary IOL implantation has its drawbacks and advantages, but all can be used with relative success. The modern surgeon should be adaptable in his or her own surgical approach to these complex cases.
REFERENCES
- Melamud A, Topilow JS, Cai L, He X. Pars plana vitrectomy with either scleral-fixated or anterior chamber intraocular lens implantation. Am J Ophthalmol. 2016;168:177-182.
Comments from Omesh Gupta MD, MBA, Retina Service, Wills Eye Hospital/Mid Atlantic Retina:
We are fortunate to have many ways to manage secondary IOL placement in the setting of pars plana vitrectomy and lensectomy. The surgical approach can be dictated by the patient age, comorbid ocular conditions, anatomic considerations, surgeon preference, and referring doctor preference. Comorbid ocular conditions such as glaucoma may preclude the insertion of an ACIOL. Iris trauma or other causes of iris defects may also eliminate the option of an ACIOL.
Most importantly, surgeon and referring provider preference have been the primary drivers in dictating the surgical procedure. Surgeons gravitate toward techniques with which they have had the most experience and reliable results. Especially in these cases, patients typically have a very good visual potential and sometimes have unrealistic expectations. They come to your office already disappointed that their cataract experience was not what their family member or friend told them it would be. Regardless of the condition of the eye, both the patient and referring doctor hope that the ultimate outcome will be just as good as an uncomplicated cataract surgery.
For these reasons, scleral fixation of a foldable IOL with Gore-Tex suture is my preferred technique. The use of Gore-Tex suture was initially described in ocular surgery in 1996.1 Since that report, there have been no reports of suture breakage or erosion. Gore-Tex has been used in vascular and cardiac surgery, which underscores its resiliency. Moreover, there is minimal biologic response and the porous quality allows for cellular ingrowth. In particular, this suture remains quiet between the conjunctiva and sclera and over time becomes barely visible. The safety and efficacy of this procedure has been previously described.2-4
Recently, this technique was shown to have a lower rate of postoperative corneal edema compared to ACIOL insertion.5 This is a relatively straightforward technique to learn, and even beginning surgeons can usually perform this around the same time as inserting an ACIOL.
Initially, this technique was described using the Bausch + Lomb Akreos AO60 lens. This lens is hydrophobic and can opacify with air or gas contact. The Bausch + Lomb MX60 lens has been more recently described using a similar technique.6 This lens is hydrophilic and does not opacify with air or gas contact (Figure 1).
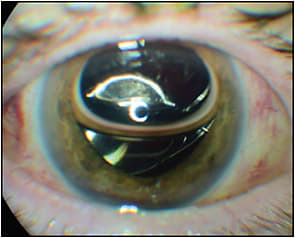
At 1 month, these eyes have an excellent visual outcome with minimal refractive error (Figure 2). We conducted a retrospective review of the 52 cases performed at our institution using this lens. There were no significant intraoperative or postoperative complications noted, and the IOL was well centered with minimal IOL tilt. Air or gas was used in 21 eyes (40%) and no opacification was noted.

Ultimately, the surgeon chooses the appropriate procedure based on the clinical scenario. Considering the known intraoperative and postoperative complications with all lens procedures, Gore-Tex scleral fixated IOLs have the most universal application with reliable results in my hands. RP
REFERENCES
- Rosenthal KJ. Baylor Welsh Cataract and Refractive Congress; 1996 Sept 5-7; Houston, TX.
- Khan MA, Gerstenblith AT, Dollin ML, Gupta OP, Spirn MJ. Scleral fixation of posterior chamber intraocular lenses using gore-tex suture with concurrent 23-gauge pars plana vitrectomy. Retina. 2014:34:1477-1480.
- Khan MA, Gupta OP, Smith GD, et al. Scleral-fixation of intraocular lenses using Gore-Tex suture: clinical outcomes and safety profile. Br J Ophthalmol. 2016;100(5):638-643.
- Khan MA, Rahimy E, Gupta OP, Hsu J. Combined 27-gauge pars plana vitrectomy and scleral fixation of an Akreos AO60 intraocular lens using Gore-Tex suture. Retina. 2016;36(8):1602-1604.
- Khan MA, Gupta OP, Pendi K, et al. Pars plana vitrectomy with anterior chamber versus Gore-Tex sutured posterior chamber intraocular lens placement: long-term outcomes. Retina. In press.
- Gupta OP. A novel technique for IOL fixation using Gore-Tex suture and vitreoretinal instrumentation: outcomes and imaging. Presented at: 2017 Retina Society Annual Meeting, Boston, MA.








