Cystoid macular edema (CME) is a well-described feature of certain hereditary retinal degenerations, including retinitis pigmentosa (RP), juvenile X-linked retinoschisis (XLRS), enhanced S-cone syndrome (ESCS), choroideremia, and gyrate atrophy.1 It can affect the central VA of patients who may already have severely constricted peripheral visual fields. The pathogenesis of CME in hereditary retinal degenerations is poorly understood. Breakdown of the blood-retinal barrier, dysfunction of the retinal pigment epithelium (RPE) pumping mechanism, Müller cell dysfunction, disruption of the retinal architecture by defects in cell-to-cell adhesion, antiretinal antibodies, and vitreous traction are thought to contribute to CME in RP.2 Fluorescein angiography (FA) shows minimal or no leakage into these cystoid spaces, suggesting that vascular leakage does not play a role in this clinical setting.3 While there is no known therapy to halt the progression of photoreceptor degeneration, we review here the options for the treatment of CME in hereditary retinal degenerations.
Joon-Bom Kim, MD, is a vitreoretinal resident with the Flaum Eye Institute, University of Rochester, in New York. Mina M. Chung, MD, and Ajay E. Kuriyan, MD, MS, are vitreoretinal specialists with the Flaum Eye Institute. Dr. Kim reports no related disclosures. Dr. Chung reports consultancy to Santen, Inc., and Wave Life Sciences and research grant support from Lowy Medical Research Institute. Dr. Kuriyan reports consultancy to Allergan and Alimera Sciences. Reach Dr. Kuriyan at ajay.kuriyan@gmail.com.
RETINITIS PIGMENTOSA
Retinitis pigmentosa encompasses a complex group of hereditary retinal dystrophies characterized by the degeneration of rod-greater-than-cone photoreceptors. Early symptoms include nyctalopia and insidious progressive peripheral visual field loss that can culminate in central vision loss and complete blindness.4 Hallmark funduscopic features include attenuated retinal arterioles, RPE atrophy and hyperplasia with bone spicule pigmentation, and optic nerve pallor (Figure 1). Electroretinography (ERG) typically shows diminished responses under scotopic greater than photopic conditions, but results can range from near-normal to undetectable depending on disease severity. The prevalence of CME in RP patients has been reported to be between 20% and 50%, with more recent studies showing higher rates of CME found on optical coherence tomography (OCT) than previously reported with FA.5-8
JUVENILE X-LINKED RETINOSCHISIS
Juvenile X-linked retinoschisis is an early-onset retinal degeneration affecting males. Patients typically present around school age with bilateral mild to moderate central vision loss. Fundus examination shows a spoke-wheel pattern of macular schisis in the inner retinal layers in 98% to 100% of patients (Figure 2). Less than 50% of patients additionally develop peripheral retinoschisis, characterized by a sharply delineated separation of the inner retinal layer usually in the temporal peripheral retina, but it can extend to the macula. Spectral-domain OCT (SD-OCT) has identified that foveomacular schisis occurs due to splitting of the inner nuclear layer (INL) (Figure 2C), and extramacular schisis is present in the INL, outer nuclear layer, and ganglion cell layer.9 The characteristic ERG is “electronegative,” with the a-wave larger than the b-wave.10 Multifocal electroretinography (mfERG) demonstrates widespread central and peripheral cone-system dysfunction.11

ENHANCED S-CONE SYNDROME
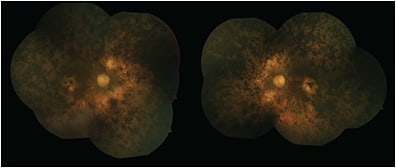
Enhanced S-cone syndrome, also called Goldmann-Favre syndrome, is an autosomal recessive vitreoretinal degeneration related to mutations in the NR2E3 gene, also called photoreceptor-specific nuclear receptor (PNR).12,13 Patients present with night blindness and visual field deficits. Fundus examination typically shows nummular pigmentary deposition at the level of the RPE along the vascular arcades (Figure 3),14,15 and in more severe cases, it may show fibrillar vitreous degeneration, chorioretinal atrophy, a sharply demarcated circumferential pigmentary retinal degeneration, macular and/or peripheral retinoschisis, presenile cataracts and hyperopia.13,16

Electroretinogram recordings show severe reduction in rod function and relatively enhanced function of short wavelength-sensitive cones. The prevalence of CME in ESCS is difficult to estimate due to the rarity of the condition; however, in a case series of 19 ESCS patients, 9 had foveal schisis-like changes, 4 of whom with foveal cysts on OCT.14
TREATMENT OF CME IN HEREDITARY RETINAL DEGENERATIONS
Carbonic Anhydrase Inhibitors
Carbonic anhydrase inhibitors (CAIs) act on membrane-bound carbonic anhydrase (CA) IV receptors on the apical and basolateral cell membrane of the RPE, and they decrease standing potential of RPE and acidify the subretinal space by increasing chloride ion transport. The resulting increase in the rate of subretinal fluid absorption across the RPE to the choroid improves CME.17 Several studies have shown improvement in RP-CME with oral and topical CAIs (Figure 4).18-24 In the largest retrospective series studying RP-CME treated with CAIs, among 81 RP patients (157 eyes) with CME, 40% of eyes treated with topical dorzolamide (Trusopt, Merck) and 28% of eyes treated with oral acetazolamide (Diamox, Duramed) showed objective improvement in CME on OCT.20 Rebound CME in RP patients has been reported after discontinuation of CAIs, but reintroduction of CAI restored treatment response in these patients.24

Carbonic anhydrase inhibitors have been used for treatment of CME in XLRS patients with positive response in several studies.25-27 In the largest retrospective study of the therapeutic effect of topical CAIs on CME in XLRS, in 29 eyes (15 patients) with XLRS treated with topical dorzolamide, 20 (69%) of 29 eyes had anatomic improvement, and 16 eyes (55%) showed improvement in VA.27
Cystoid macular edema in ESCS has shown mixed response to CAIs. Iannaccone et al reported a case of CME in an adult ESCS patient treated with oral acetazolamide, whose VA improved from 20/200 to 20/20.28 However, Busic et al reported a case of a 7-year old patient with ESCS with CME treated with topical dorzolamide with no reduction in thickness or improvement in BCVA.29 These reports suggest either different mechanisms of CME in adults and children with ESCS or, more likely, variable response to CAIs in ESCS.
Anti-VEGF
Vascular endothelial growth factor (VEGF) is an important promoter of vascular permeability and an inhibitor of endothelial barrier function, which can cause CME. Using this rationale, anti-VEGF agents have been tried for the treatment for CME in RP patients with varying results.30-34 Several small case series studying the effect of intravitreal bevacizumab (Avastin; Genentech), ranibizumab (Lucentis; Genentech), and aflibercept (Eylea; Regeneron) have demonstrated improvement in macular edema and/or VA.30-33 However, another study of 2 eyes in 2 patients treated with a single injection of intravitreal bevacizumab demonstrated no anatomic or functional improvement.34
Steroids
Inflammatory cell proliferation and migration can contribute to blood-retina barrier dysfunction, resulting in CME. Various intravitreal corticosteroids have been studied for the treatment of CME in RP patients who are believed to have an impaired blood-retina barrier due to dysfunction of RPE pumping mechanism. A prospective, nonrandomized trial comparing 20 eyes of 20 RP patients who received intravitreal injection of triamcinolone acetonide and 20 eyes of 20 patients who declined treatment found improvement in central macular thickness in the treatment group but no significant change in vision.35 A multicenter, retrospective case series of 45 eyes from 34 patients with RP and CME treated with intravitreal dexamethasone implant (Ozurdex; Allergan) found improvement in VA in 27 (60%) of 45 eyes after 4 months.36 Fourteen eyes required multiple injections, and seven patients developed visually significant cataracts.36
SUMMARY
Cystoid macular edema can cause significant visual impairment. Treatment interventions such as CAIs, anti-VEGF, and corticosteroids have been used with varying success, and no standard of care has been established. Further research to better understand retinal degenerations and the pathogenesis and mechanism of CME will aid in the development of targeted, effective treatment. RP
REFERENCES
- Salvatore S, Fishman GA, Genead MA. Treatment of cystic macular lesions in hereditary retinal dystrophies. Surv Ophthalmol. 2013;58(6):560-684.
- Strong S, Liew G, Michaelides M. Retinitis pigmentosa-associated cystoid macular oedema: pathogenesis and avenues of intervention. Br J Ophthalmol. 2017;101(1):31-37.
- Ganesh A, Stroh E, Manayath GJ, Al-Zuhaibi S, Levin AV. Macular cysts in retinal dystrophy. Curr Opin Ophthalmol. 2011;22(5):332-339.
- Narayan DS, Wood JPM, Chidlow G, Casson RJ. A review of the mechanisms of cone degeneration in retinitis pigmentosa. Acta Ophthalmol (Copenh). 2016;94(8):748-754.
- Chung H, Hwang J-U, Kim J-G, Yoon YH. Optical coherence tomography in the diagnosis and monitoring of cystoid macular edema in patients with retinitis pigmentosa. Retina. 2006;26(8):922-927.
- Hajali M, Fishman GA, Anderson RJ. The prevalence of cystoid macular oedema in retinitis pigmentosa patients determined by optical coherence tomography. Br J Ophthalmol. 2008;92(8):1065-1068.
- Adackapara CA, Sunness JS, Dibernardo CW, Melia BM, Dagnelie G. Prevalence of cystoid macular edema and stability in OCT retinal thickness in eyes with retinitis pigmentosa during a 48-week lutein trial. Retina. 2008;28(1):103-110.
- Testa F, Rossi S, Colucci R, et al. Macular abnormalities in Italian patients with retinitis pigmentosa. Br J Ophthalmol. 2014;98(7):946-950.
- Gregori NZ, Lam BL, Gregori G, et al. Wide-field spectral-domain optical coherence tomography in patients and carriers of X-linked retinoschisis. Ophthalmology. 2013;120(1):169-174.
- Khan NW, Jamison JA, Kemp JA, Sieving PA. Analysis of photoreceptor function and inner retinal activity in juvenile X-linked retinoschisis. Vis Res. 2001;41(28):3931-3942.
- Piao C-H, Kondo M, Nakamura M, Terasaki H, Miyake Y. Multifocal electroretinograms in X-linked retinoschisis. Invest Ophthalmol Vis Sci. 2003;44(11):4920-4930.
- Schorderet DF, Escher P. NR2E3 mutations in enhanced S-cone sensitivity syndrome (ESCS), Goldmann-Favre syndrome (GFS), clumped pigmentary retinal degeneration (CPRD), and retinitis pigmentosa (RP). Hum Mutat. 2009;30(11):1475-1485.
- Sharon D, Sandberg MA, Caruso RC, Berson EL, Dryja TP. Shared mutations in NR2E3 in enhanced S-cone syndrome, Goldmann-Favre syndrome, and many cases of clumped pigmentary retinal degeneration. Arch Ophthalmol. 2003;121(9):1316-1323.
- Audo I, Michaelides M, Robson AG, et al. Phenotypic variation in enhanced S-cone syndrome. Invest Ophthalmol Vis Sci. 2008;49(5):2082-2093.
- Hull S, Arno G, Sergouniotis PI, et al. Clinical and molecular characterization of enhanced S-cone syndrome in children. JAMA Ophthalmol. 2014;132(11):1341-1349.
- Yzer S, Barbazetto I, Allikmets R, et al. Expanded clinical spectrum of enhanced S-cone syndrome. JAMA Ophthalmol. 2013;131(10):1324-1330.
- Wolfensberger TJ, Mahieu I, Jarvis-Evans J, et al. Membrane-bound carbonic anhydrase in human retinal pigment epithelium. Invest Ophthalmol Vis Sci. 1994;35(9):3401-3407.
- Liew G, Moore AT, Webster AR, Michaelides M. Efficacy and prognostic factors of response to carbonic anhydrase inhibitors in management of cystoid macular edema in retinitis pigmentosa. Invest Ophthalmol Vis Sci. 2015;56(3):1531-1536.
- Grover S, Fishman GA, Fiscella RG, Adelman AE. Efficacy of dorzolamide hydrochloride in the management of chronic cystoid macular edema in patients with retinitis pigmentosa. Retina. 1997;17(3):222-231.
- Grover S, Apushkin MA, Fishman GA. Topical dorzolamide for the treatment of cystoid macular edema in patients with retinitis pigmentosa. Am J Ophthalmol. 2006;141(5):850-858.
- Genead MA, Fishman GA. Efficacy of sustained topical dorzolamide therapy for cystic macular lesions in patients with retinitis pigmentosa and usher syndrome. Arch Ophthalmol. 2010;128(9):1146-1150.
- Ikeda Y, Hisatomi T, Yoshida N, et al. The clinical efficacy of a topical dorzolamide in the management of cystoid macular edema in patients with retinitis pigmentosa. Graefes Arch Clin Exp Ophthalmol. 2012;250(6):809-814.
- Ikeda Y, Yoshida N, Notomi S, et al. Therapeutic effect of prolonged treatment with topical dorzolamide for cystoid macular oedema in patients with retinitis pigmentosa. Br J Ophthalmol. 2013;97(9):1187-1191.
- Fishman GA, Apushkin MA. Continued use of dorzolamide for the treatment of cystoid macular oedema in patients with retinitis pigmentosa. Br J Ophthalmol. 2007;91(6):743-745.
- Walia S, Fishman GA, Molday RS, et al. Relation of response to treatment with dorzolamide in X-linked retinoschisis to the mechanism of functional loss in retinoschisin. Am J Ophthalmol. 2009;147(1):111-115.
- Apushkin MA, Fishman GA. Use of dorzolamide for patients with X-linked retinoschisis. Retina. 2006;26(7):741-745.
- Genead MA, Fishman GA, Walia S. Efficacy of sustained topical dorzolamide therapy for cystic macular lesions in patients with X-linked retinoschisis. Arch Ophthalmol. 2010;128(2):190-7.
- Iannaccone A, Fung KH, Eyestone ME, Stone EM. Treatment of adult-onset acute macular retinoschisis in enhanced s-cone syndrome with oral acetazolamide. Am J Ophthalmol. 2009;147(2):307-312.e2.
- Busic M, Bjelos M, Bosnar D, Ramic S, Busic I. Cystoid macular lesions are resistant to topical dorzolamide treatment in enhanced S-cone syndrome child. Doc Ophthalmol Adv Ophthalmol. 2016;132(1):67-73.
- Yuzbasioglu E, Artunay O, Rasier R, Sengul A, Bahcecioglu H. Intravitreal bevacizumab (Avastin) injection in retinitis pigmentosa. Curr Eye Res. 2009;34(3):231-237.
- Artunay O, Yuzbasioglu E, Rasier R, Sengul A, Bahcecioglu H. Intravitreal ranibizumab in the treatment of cystoid macular edema associated with retinitis pigmentosa. J Ocul Pharmacol Ther. 2009;25(6):545-550.
- Moustafa G-A, Moschos MM. Intravitreal aflibercept (Eylea) injection for cystoid macular edema secondary to retinitis pigmentosa - a first case report and short review of the literature. BMC Ophthalmol. 2015;15:44.
- Strong SA, Gurbaxani A, Michaelides M. Treatment of retinitis pigmentosa-associated cystoid macular oedema using intravitreal aflibercept (Eylea) despite minimal response to ranibizumab (Lucentis): a case report. Case Rep Ophthalmol. 2016;7(2):389-397.
- Melo GB, Farah ME, Aggio FB. Intravitreal injection of bevacizumab for cystoid macular edema in retinitis pigmentosa. Acta Ophthalmol Scand. 2007;85(4):461-463.
- Scorolli L, Morara M, Meduri A, et al. Treatment of cystoid macular edema in retinitis pigmentosa with intravitreal triamcinolone. Arch Ophthalmol. 2007;125(6):759-764.
- Mansour AM, Sheheitli H, Kucukerdonmez C, et al. Intravitreal dexamethasone implant in retinitis pigmentosa-related cystoid macular edema. Retina. 2017 Feb 17. [Epub ahead of print]








