Recent studies have shown that the incidence of late intraocular lens (IOL) dislocations is rising, increasing the potential for necessary surgical intervention.1-4 This is not entirely unexpected, because the number of patients with IOL implants is increasing, and these patients are living longer. Consequently, the demand for vitreoretinal surgeons who can reposition or replace dislocated IOLs is expected to increase.
There are many ways to fixate an IOL in the eye when there is inadequate capsular support, including an anterior chamber IOL, an iris claw IOL, iris fixation sutures, scleral fixation of the IOL, and anchoring of the IOL haptics inside scleral tunnels. With scleral fixation, the IOL is fixated in the ciliary sulcus. Traditionally, the dislocated IOL is removed and a new one is implanted with scleral fixation sutures. The IOL fixation sutures are then passed via an ab externo or ab interno approach by passing long suture needles into a hollow 27-gauge needle or grasping the suture with microforceps. The haptics are anchored to the sclera with a nonabsorbable fixation suture. Alternatively, the dislocated IOL can be salvaged by repositioning it and fixating it to the sclera with either fixation sutures or by placing the haptics into scleral tunnels.5,6 This approach obviates the need for a large corneal wound because the dislocated IOL is not removed. However, this technique is more difficult to master and has a steeper learning curve than the IOL exchange approaches.
Passing scleral fixation sutures through the eye and attaching them to the IOL haptics can be technically challenging and cumbersome. The introduction of disposable microforceps has helped with grasping and pulling sutures or haptics in a straight line, but they are not designed for grasping or passing sutures at a 90° angle and must be bent to the appropriate angle. They can malfunction if bent too far, and they increase procedure cost. Implantation of the haptics in scleral tunnels has grown in popularity recently but also presents challenges.6 When the surgeon grasps the old haptics of a dislocated IOL with microforceps and pulls them out of the sclerotomy or microcannula, the haptics can break or deform. Additionally, some haptics can spontaneously slip out of the scleral tunnels, causing lens tilt or redislocation of the IOL immediately after surgery.6 For these reasons, some surgeons avoid scleral-fixated IOLs and use an anterior chamber IOL for their dislocation patients.
We have developed a technique that simplifies implantation of scleral-fixated IOLs using a 27-gauge microsuture passer (TruMed Design) to pass the scleral fixation sutures. It stabilizes the IOL with 3-point fixation, producing excellent IOL centration without tilt. The suture knots are rotated internally so that they are not exposed. We have been using this technique successfully in our practice since 1989. This report presents the long-term safety and efficacy of 79 consecutive patients who had scleral fixated IOLs implanted with this instrument and technique in our practice.
METHODS
After obtaining a waiver of HIPAA authorization from the Institutional Review Board of Temple University in Philadelphia, Pennsylvania, a retrospective chart review was performed of a consecutive series of 79 patients with scleral-fixated CZ70BD IOL implants (Alcon Laboratories) implanted with either 9-0 or 10-0 Prolene polypropylene fixation sutures (Ethicon) using the microsuture passer instrument in a retinal referral practice between 2004 and 2016. The microsuture passer used in these cases is designed to pass and retrieve sutures within the eye to fixate an IOL to the sclera. It has a 27-gauge curved shaft with an eyelet and a handle on the proximal end of the device (patent pending) (Figure 1). Statistics were measured with JMP, Version Pro 12 (SAS Institute Inc.). A P value <.05 was considered statistically significant.

TECHNIQUE
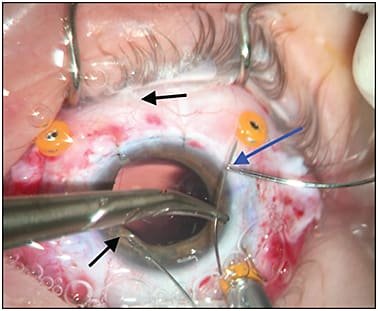
After the patient has been placed under anesthesia and prepped and draped, a speculum is placed to retract the eyelids. A segmental conjunctival periotomy is performed temporally and nasally. An infusion cannula is placed inferotemporally. A 7.5 mm clear corneal incision is created superiorly with the keratome. The anterior chamber is not entered. The toric IOL corneal marker is used to mark the 3 and 9 o’clock positions (Figure 2). At each marked position, 2 sclerotomies are created with the microcannula trocar or with a 25-gauge needle 1.5 mm to 2 mm posterior to the limbus, 2 mm to 3 mm above and below the marked midpoint line. Each sclerotomy is marked with the marking pen for easy identification later (Figure 3). The remaining 2 microcannulas are placed in the traditional locations with care to avoid the fixation suture sclerotomies. A pars plana vitrectomy is performed. As needed, the retained lens fragments or dislocated IOL are completely removed from the eye. The CZ70BD IOL implant is now transferred to the field and positioned above the eye on an instrument wipe. The clear corneal incision is now opened, if not previously done.


The first suture is loaded into the microsuture passer (Figure 4). A needle (CIF, Ethicon) is left on one end of the suture to help weigh it down it while sutures are passed. Starting at the 9 o’clock position and then repeating at the 3 o’clock position, the loaded suture-passing instrument is passed through one of the sclerotomies and out through the clear corneal incision (Figure 5). The suture is grasped with a tying forceps and the suture passer is pulled back through the sclerotomy. The free end of the suture is then threaded through an eyelet on the IOL haptic. The trailing end is then passed through the other sclerotomy at 9 o’clock and out through the clear corneal incision to retrieve the trailing end of the suture. This is passed into the eyelet of the microsuture passer (Figure 5). The microsuture passer is withdrawn, pulling the suture back through the sclerotomy. The suture is pulled tight and to the side of the corneal incision to avoid tangling with the next suture. In an identical way, the second suture is passed through the sclerotomies at the 3 o’clock position and through the eyelet on the opposite haptic of the IOL (Figure 6). The new suture is also pulled tight and to the side of the corneal incision. The IOL is now inserted into the posterior chamber, guided into place by the fixation sutures at 9 o’clock (Figures 7-8). The superior haptic is intentionally left outside of the incision. The first fixation suture is now tightened to secure the IOL’s haptic to the ciliary sulcus with 3-point fixation. A temporary surgeon’s knot with 3 throws is used to secure the inferior haptic. The superior haptic is now inserted into the ciliary sulcus and guided into place by the other fixation suture. This is also temporarily tied with a surgeon’s knot. A corneal protector is placed on the cornea to prevent phototoxicity. The clear corneal incision is then closed with 10-0 nylon sutures. The tension on the fixation sutures is then carefully adjusted. The IOL is usually well centered at this point. The fixation sutures are permanently tied with care not to overtighten them. The fixation sutures are carefully rotated inside one of the sclerotomies so that the knot is internalized and not exposed on the outside of the sclera (Figure 9). The microcannulas are removed from the sclerotomies. The sclerotomies are closed with an absorbable suture. The infusion cannula is removed from the eye. The conjunctiva is closed with interrupted sutures. Eye drops containing antibiotic and steroid are administered. A patch and shield are placed over the eye.





RESULTS
This series included 79 eyes with follow-up of 0.5 years to 11.9 years (mean = 2.1 years). Baseline characteristics are summarized in Table 1. The mean age of the patients was 68 (age range: 23-89; 28 female, 51 male). The most common indications for requiring a scleral fixated IOL are listed in Table 2 and include: dislocated-subluxated IOL (42), dislocated lens fragments or crystalline lens (15), S/P complex retinal detachment repair (13), aphakia (7), and trauma (2).
| Total Patients | 79 |
| Total Eyes | 79 |
| AGE (YEARS) | |
| Range | 23-89 |
| Mean | 68 |
| GENDER | |
| Male | 51 |
| Female | 28 |
| PREOPERATIVE LOGMAR VISUAL ACUITY (SNELLEN) | |
| Range | 0.08-3.00 (20/25-20/20000) |
| Mean | 1.41 (20/514) |
| LAST-RECORDED POSTOPERATIVE LOGMAR VISUAL ACUITY (SNELLEN) | |
| Range | 0.03-3.00 (20/20-20/20000) |
| Mean | 0.87 (20/144) |
| DURATION OF FOLLOW-UP (YEARS) | |
| Range | 0.5-11.9 |
| Mean | 2.1 |
| INDICATION (NUMBER OF EYES) | PREOPERATIVE VISUAL ACUITY (VA) (LOGMAR) | LAST-RECORDED POSTOPERATIVE VA (LOGMAR) |
|---|---|---|
| Overall (79) | 20/514 (1.19) | 20/144 (0.87) (P<.0001) |
| SURGICAL INDICATION | ||
| Dislocated-subluxated IOL (42) | 20/303 (1.19) | 29/91 (0.67) |
| Dislocated lens fragments-crystalline lens (15) | 20/1868 (1.98) | 20/166 (0.93) |
| S/P retinal detachment repair (13) | 20 /633 (1.50) | 20/873 (1.65) |
| Aphakia (7) | 20/469 (1.38) | 20/65 (0.51) |
| Trauma (2) | 20/2000 (2.0) | 20/246 (1.10) |
The preoperative Snellen visual acuities (VA) of the 79 patients ranged from 20/25 to 20/20000. The mean preoperative logMAR visual acuity was 1.41 (20/514 Snellen equivalent). The mean last-recorded postoperative visual acuity improved to 0.86 (20/144 Snellen equivalent) and ranged from 20/20 to 20/20000 (P<0.0001). Many of our scleral fixation IOL patients had serious retinal conditions that precluded them from obtaining excellent postoperative visual acuities. As expected, those patients with complex retinal detachments, macular degeneration, ruptured globe, severe blunt trauma, or a previous macular hole fared worse than those with aphakia, dislocated IOL, or dislocated lens fragments or crystalline lens (Table 2). The best visual acuity results were in the aphakic eyes (improving from 20/469 to 20/65), the dislocated IOL eyes (improving from 20/303 to 20/91), and the dislocated lens fragments and crystalline lens eyes (improving from 20/1868 to 20/166). Of the 79 eyes in our review, 23 eyes (28.8%) achieved a post-operative visual acuity of 20/40 or better at the last follow up. The traumatic eyes fared poorly (VA improving from 20/2000 to 20/246) and the complex retinal detachment eyes worsened (from 20/633 to 20/873).
There were no cases of endophthalmitis or malpositioned IOL. Complications included transient corneal edema in 27 patients (34%), elevated intraocular pressure in 16 patients (20%), transient hypotony in 12 patients (15%) that resolved spontaneously within the first week, exposed suture tips which appeared 1-3 months after surgery due to incomplete internal rotation were resolved with in-office trimming in 10 patients (12.5%), recurrent retinal detachment with proliferative vitreoretinopathy in 3 patients (4%) and suture breakage with dislocation of the IOL in 2 patients (2.5%). There were no cases of endophthalmitis, tilted IOL or malpositioned IOL.
For both cases that developed a broken fixation suture with subluxation of the IOL (Table 3), the IOLs were fixated with 10-0 Prolene sutures (8.3% of the 24 eyes operated on using the 10-0 Prolene fixation sutures). In the first patient, the 10-0 Prolene suture broke at 5 years and 3 months postoperatively. This dislocated haptic was “lassoed” with a 9-0 Prolene using the suture passer. In the second patient, the suture broke at 4 years and 2 weeks postoperatively. An IOL exchange was performed with placement of an AC IOL. There were no broken sutures with the 9-0 Prolene sutures (0/55) (P<.05). For this reason, we permanently switched to 9-0 Prolene sutures for scleral fixation after 2007 and have not had any other cases of suture breakage.
| PROLENE SUTURE USED | INCIDENCE OF FIXATION SUTURE BREAKAGE | NUMBER OF EYES |
|---|---|---|
| 9-0 | 0 | 55 |
| 10-0 | 2 | 24 |
| P value | <.05 |
DISCUSSION
Prior to 1986, the choices for a patient with inadequate capsular support were limited to an anterior chamber IOL, an iris-claw IOL, or an iris-suture fixated posterior chamber IOL.7-9 Complications were significant and included corneal decompensation, iris atrophy and chafe, chronic uveitis, pigment dispersion syndrome, glaucoma, hyphema, cystoid macular edema, and pseudophacodonesis.7 In 1986, Malbran et al reported using a “guide” suture for the fixation of a secondary IOL after intracapsular cataract surgery, ushering in a new era in which IOL implantation in the posterior chamber/ciliary sulcus was an option for patients with inadequate capsular support.8
Hu et al and others improved upon the Malbran technique in several ways.9-10 They added scleral flaps to cover the knot and minimize erosion of the suture knot through the conjunctiva, which posed a significant risk for endophthalmitis.7,9 Over time, however, some of the scleral flaps thinned and the knot could still erode through both the flap and the conjunctiva in a delayed fashion.11 Hoffman et al used a scleral tunnel to decrease the risk of conjunctival erosion, knot exposure, and endophthalmitis.12
Rotation of the knot into the eye reduces the risk of knot exposure and endophthalmitis.13-15 Yuksel et al reported a 20.6% rate of suture knot erosion with scleral flaps compared to 0% when the knots were buried in 56 eyes that underwent trans-scleral sutured IOL implantation.16 An advantage of the technique described here is that it is relative easy to bury the knots and thus there is no need to create a scleral flap. In 10/79 (12.5%) of the eyes in this series, one of the knots could not be safely rotated into the sclerotomy at the time of surgery and the knot was left exposed. The exposed knot tip was either trimmed or shrunk with the laser in the office. There were no cases of endophthalmitis in our series.
In early cases, some IOLs dislocated because the suture slipped off the haptic. This problem was circumvented by selecting an IOL with a loop at the end of the haptic or creating a bulb on the end of the haptic with the heat from a cautery.9 Alcon later introduced the CZ70BD IOL with strategically placed eyelets at the midpoint of the curve of the haptic.7 This simplified placement and eliminated slippage of sutures. The CZ70BD was the IOL of choice for scleral-fixated IOLs for nearly two decades. Recently, Khan et.al reported good results using a 4-eyelet IOL, the Akreos A060 (Bausch + Lomb), with Gore-Tex sutures (W. L. Gore & Associates) for scleral fixation.1,17,18 There were no cases of suture erosion or breakage with a mean follow-up of 325 days.17 The Akreos IOL is acrylic and foldable, allowing it to be inserted through a 2.8 mm incision. The CZ70BD is PMMA, not foldable, and requires a 7.5 mm incision. Both the CZ70BD and the Akreos AO60 must be special ordered before the surgery. Although this paper focused exclusively on the CZ70BD, the microsuture passer will work well with any IOL that has eyelets, including the Akreos AO60.
A late complication of scleral-fixated IOLs is suture breakage and dislocation of the lens. The reported rate of dislocation of scleral-sutured IOLs varies from a high of 27.9% to 2.2%. Vote et al reported a 27.9% rate of suture breakage with dislocation of the IOL in their series of 61 eyes that received a scleral fixated CZ70BD IOL with a mean follow-up of 6 years. Their surgical technique used 10-0 Prolene fixation sutures at the 6 o’clock and 12 o’clock positions under half-thickness triangular scleral flaps.19 Walter et al reported 2 of 89 eyes (2.2%) with suture breakage, also with 10-0 Prolene suture used for trans-scleral fixation of secondary IOLs during penetrating keratoplasty.20
Although several innovative techniques for scleral fixation of IOLs have been introduced during the past 5 years, this technique remains a viable option and has several advantages. The 90° curve simplifies suture passing and retrieval and eliminates the issues associated with bending the microforceps. Suture tangling and inversion of the IOL during implantation is reduced. The suture knot can be buried by rotating it inside of the eye in most cases without the need for a scleral flap. The 3-point fixation (2 sclerotomies and the eyelet on the IOL) holds the curvature of the haptic securely in the ciliary sulcus. Tilting and posterior subluxation of the IOL are minimized. Malposition of the IOL can be more problematic with 2-point fixation techniques. The microsuture passer is gentle on the sutures, with few broken sutures reported. It is less expensive than disposable microforceps. It can also be used to “lasso” the free haptic of a subluxated IOL. This was used to salvage and reposition the haptic of the subluxated IOL in one of our 2 patients with a broken fixation suture.
CONCLUSIONS
The microsuture passer simplifies the placement of scleral fixation sutures for implantation of scleral fixated IOLs. The suture knots are rotated internally, eliminating the need for a scleral flap. To minimize the risk of suture breakage, a previously documented complication, 9-0 Prolene sutures are preferred over 10-0 sutures for IOL fixation. This technique produces good long-term results and stability for scleral-fixated IOLs, and results in a well-centered IOL without tilt. RP
REFERENCES
- Bethke, W. Should RLE surgeons brace for dislocations? Rev Ophthalmol. 2017 January;74:18-19.
- Liu E, Cole S, Werner L, Hengerer F, Mammals N, Kohnen T. Pathologic evidence of pseudoexfoliation in cases of in-the-bag intraocular lens subluxation or dislocation. J Cataract Refract Surg. 2015;41(5):929-935.
- Pueringer SL, Hodge DO, Erie JC. Risk of late intraocular lens dislocation after cataract surgery. Am J Ophthalmol. 2011;152(4):618-623.
- Ascao FJ, Huerva V, Grzybowski A. Epidemiolgy, etiology and prevention of late IOL capsular bag complex dislocation: review of the literature. J Ophthalmol. 2015:805706.
- Khan MA, Gerstenblith AT, Dollin ML, Gupta OP, Spirn MJ. Scleral fixation of posterior chamber intraocular lenses using Gore-Tex suture with concurrent 23-gauge pars plana vitrectomy. Retina. 2014;34(7):1477-1480.
- Prenner JL, Feiner L, Wheatley HM, Connors D. A novel approach for posterior chamber intraocular lens placement or rescue via futureless scleral fixation technique. Retina. 2012;32(4):853-855.
- Lane SS, Lubniewski AJ, Holland EJ. Transsclerally sutured posterior chamber lenses: improved lens designs and techniques to maximize lens stability and minimize suture erosion. Semin Ophthalmol. 1992;7(4):245-252.
- Malbran ES, Malbran E, Negri I. Lens guide suture for transport and fixation in secondary IOL implantation after intracapsular extraction. Int Ophthalmol. 1986;9(2-3):151-160.
- Hu BV, Shin DH, Gibbs KA, Hong YJ. Implantation of a posterior chamber lens in the absence of capsular zonular support. Arch Ophthalmol. 1988;106(3):416-420.
- Holt DG, Young J, Stagg B, Ambati BK. Anterior chamber intraocular lens, sutured posterior chamber intraocular lens, or glued intraocular lens. Curr Opin Ophthalmol. 2012;23(1):62-67.
- Schechter RJ. Suture-wick endophthalmitis with sutured posterior chamber intraocular lenses. J Cataract Refract Surg. 1990;16(6):755-756.
- Hoffman RS, Fine IH, Packer M, Rozenberg I. Scleral fixation using suture retrieval through a scleral tunnel. J Cataract Refract Surg. 2006;32(8):1259-1263.
- Lewis JS. Sulcus fixation without flaps. Ophthalmology. 1993;100(9):1346-1350.
- Buckley EG. Scleral fixated (sutured) posterior chamber intraocular lens implantation in children. J AAPOS. 1999;3(5):289-294.
- Cordoves L, Gomez A, Mesa CG, Abreu JA. Sulcus transscleral sutured posterior chamber lenses. J Cataract Refract Surg. 1999;25(2):156-157.
- Yuksel B, Gulucu A, Uzunel UD, Kusbeci T. Retrospective comparison of scleral flap and scleral burial techniques to fixate a scleral sutured intraocular lens concurrently with penetrating keratoplasty. Int J Ophthalmol Clin Res. 2015;2:3.
- Khan, MA, Gupta OP, Smith RG, et al. Scleral fixation of intraocular lenses using Gore-Tex suture: clinical outcomes and safety profile. Br J Ophthalmol. 2016;100(5):638-643.
- Khan MA, Gupta O, Hsu J. Scleral fixation of a four-haptic intraocular lens using Gore-Tex suture. Retina Today. November/December 2015;35-37.
- Vote BJ, Tranos P, Bunce C, Charteris DG, Da Cruz L. Long-Term Outcome of Combined Pars Plana Vitrectomy and Scleral Fixated Sutured Posterior Chamber Intraocular Lens Implantation. Am J Ophthalmol. 2006;141(2):308-312.
- Walter KA, Wood TD, Ford JG, Winnicki J, Tyler ME, Reed JW. Retrospective analysis of a novel method of transscleral suture fixation for posterior-chamber intraocular lens implantation in the absence of capsular support. Cornea. 1998;17(3):262-266.








