Intraocular foreign body (IOFB) cases are challenging and can have variable visual outcomes. The clinical history, physical exam, and imaging are helpful in planning the surgical approach for patients with IOFBs.
EPIDEMIOLOGY
Between 20,000 and 68,000 serious vision-threatening ocular injuries occur in the United States every year.1,2 IOFBs are found in 8% to 25% of all open globe injuries (OGIs).3 Most IOFB patients are male, and most are between 21 and 40 years old.2 The most common location of injury is the work-place.2
IOFB FEATURES
Metallic IOFBs are by far most common, followed by organic material and nonmetallic inorganic material.2,4 In terms of management, glass IOFBs, which account for 6% to 9% of all IOFBs, can be observed if there is no other significant structural damage. Retained metallic IOFBs, on the other hand, can result in chalcosis and siderosis with retinal toxicity; they most often require removal.
LOCATION OF IOFBS
An IOFB can be associated with penetrating or perforating injury and can involve the anterior chamber (Figure 1), crystalline lens, posterior chamber, and even the orbit if a posterior exit wound is present. The different locations of the IOFB are important for the surgical approach. The location may also be important to the visual prognosis. One study found that posterior segment IOFBs are more likely to be associated with no-light-perception vision than anterior segment IOFBs.5

PATIENTS WITH IOFBS: EVALUATION
History
A thorough history is essential when evaluating a patient with an IOFB. The details about how the injury occurred, the use of protective eye wear, the time from injury to presentation, visual/ocular symptoms, and prior treatments should be obtained. The location of the injury (eg, work) and circumstances of the injury (eg, assault) are especially important items to document due to potential legal ramifications.
Findings of systemic involvement, such as loss of consciousness or concurrent bodily injuries associated with the trauma, should be managed with the assistance of other specialties if necessary. Prior ocular history and surgeries need to be obtained from the patient because the ability to complete a full exam is sometimes limited by the injury (eg, hyphema), and knowledge of this information is important in planning management for the patient. The history may also elucidate the material that the IOFB consists of, which is important because certain materials (eg, copper) can cause rapid and profound toxicity to the retina, while others (eg, vegetable matter) are more commonly associated with endophthalmitis.
Clinical Exam
It is important to ensure that other nonocular injuries associated with the trauma have been assessed and treated appropriately prior to initiating the ophthalmic exam. Many of these patients have concomitant head trauma or other traumatic injuries. A complete exam of the uninvolved eye is also important.
At presentation, the physician should check and document the visual acuity and relative afferent pupillary defect in the affected eye himself or herself. Intraocular pressure measurement should be deferred in patients with large lacerations. Other periocular trauma sequelae need to be evaluated, including retrobulbar hemorrhage, orbital fractures, ocular adnexa lacerations, and superficial foreign bodies. Some of these issues may need immediate attention (eg, retrobulbar hemorrhage), while others may require coordination of management with other ophthalmic subspecialties in the operating room (eg, canalicular lid laceration).
Examination of the injured eye with slit lamp biomicroscopy should be performed to evaluate the anterior segment for lacerations in the conjunctiva, cornea, and/or sclera. Seidel testing should be performed to aid in identifying leaking wounds. The anterior chamber should be evaluated for depth, cell, hypopyon, fibrin, hyphema, and/or lens material. Peaked pupils should raise suspicion for OGIs in ocular trauma patients. Additionally, the iris should be examined for transillumination defects (Figure 2) prior to dilation, which may suggest a potential IOFB.

Uveal tissue incarcerated in a laceration is a relative contraindication to pupillary dilation. If uveal incarceration is not present, dilation should be performed to fully evaluate the lens and posterior segment. The lens capsule should be examined for evidence of violation. Wrinkling of the lens capsule is suggestive of loss of nuclear or cortical material. The lens should also be examined for zonular dialysis and instability. IOFBs passing through the crystalline lens can cause a range of findings, from small focal cataractous changes to white cataracts, depending on the location of impact, size of IOFB, and time to presentation.
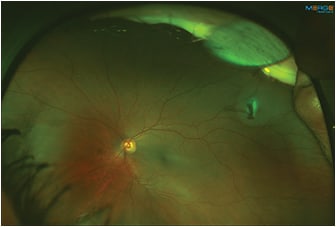
The posterior segment should be evaluated for an IOFB (Figure 3), which can be located in the vitreous, ciliary body, retina, choroid, or the posterior sclera. The posterior segment should be evaluated for traumatic posterior segment pathology such as vitreous hemorrhage, commotion, retinal tears, retinal detachment (Figure 4) or dialysis, choroidal detachment, choroidal rupture, sclopetaria, and a posterior exit wound. Dense vitreous hemorrhage or cataracts can preclude visualization of the posterior segment, so imaging modalities might be needed to identify an IOFB. In eyes that do not permit a clear view of the posterior segment, the presence of a metallic IOFB can be confirmed using a metal detector.

Imaging
Imaging is a very important part of the workup of a patient with an OGI. Computed tomography (CT) scans are fast, widely available, and effective at detecting a wide range of foreign bodies.6 Thin (1-mm) cuts with coronal (Figure 5), axial (Figure 6), and sagittal views are ideal to identify IOFBs and to assess the globe contour, site of posterior rupture, and any other cranial (eg, subarachnoid hemorrhage) or ophthalmic traumatic sequelae (eg, orbital fractures or retrobulbar hemorrhage). Although CT is able to detect most IOFBs well, wood IOFBs are usually hypodense and may be mistaken for air or fat.7 The presence of linear-appearing air should raise suspicion for a wood IOFB. Measuring the Hounsfield units of an IOFB identified on CT may provide some insight into its composition.6


Echography is not routinely used in the presence of an open globe due to the risk of expulsion of intraocular contents. However, if performed gently, it is useful for localization and identification of IOFBs, especially those located by the ciliary body, which may be harder to identify on exam.8 Plain x-ray is rarely used for IOFBs, but it is an option in cases where there is no access to a CT. Many IOFB materials are identifiable using x-ray, including metal, glass, slate, and polyvinyl chloride.6 Magnetic resonance imaging is usually avoided in open globes due to the concern for a ferromagnetic IOFB.
PRE-OPERATIVE MANAGEMENT
Initial Treatment
All patients should be started on broad-spectrum systemic and frequent topical antibiotics. A Fox shield should be placed to protect the eye from further damage. Tetanus immunization history should be obtained, and tetanus toxoid or tetanus immune globulin should be administered if necessary. The patient should be placed on nil per os (NPO) status in preparation for surgery. Any pain and nausea should be addressed, and the medical clearance for surgery should be obtained.
Counseling
After the presence of the IOFB is confirmed, the management plan should be discussed with the patient and family. Patients with better presenting vision are more likely to have better visual outcomes than those with worse presenting vision.9,10 Nevertheless, even patients with good presenting vision need to be counseled on the unpredictable final vision due to potential vision-threatening sequelae (eg, retinal detachment or endophthalmitis). There have been conflicting findings on the association between visual outcomes and IOFB features.5 However, anterior chamber IOFBs are associated with better visual outcomes than posterior segment IOFBs.5 The patient also should be informed that multiple surgeries could be needed to address all sequelae of the ocular trauma.
Timing
Generally, it is thought that an acute IOFB should be removed as soon as possible and that delaying surgery could result in higher rates of endophthalmitis and proliferative vitreoretinopathy (PVR). However, a study by Colyer and colleagues from the Walter Reed Army Medical Center showed that delayed IOFB removal (median time to IOFB removal was 21 days) with a combination of systemic and topical antibiotic coverage can result in similar visual outcomes as cases with prompt removal of IOFBs. However, those IOFBs could have potentially been sterilized by the heat from the exploding ordnance.11 Treating patients with intravitreal broad-spectrum antibiotics as prophylaxis for endophthalmitis is another option for those who have a delay in surgical management (eg, due to other traumatic injuries).
Anesthesia
General anesthesia has traditionally been used for OGIs. However, in select cases of IOFBs local anesthesia with sedation might be an option.12,13
SURGICAL MANAGEMENT
Closure of the Entry Wound
Closure of the entry wound is usually the first step of surgical management. While corneal wounds are easily identified, a conjunctival peritomy is needed to identify the full extent of most scleral wounds. Corneal wounds are often closed with 10-0 nylon suture and sclera can be closed with 9-0 or 8-0 nylon sutures. Buried sutures often improve the postoperative comfort of patients.
Anterior Chamber IOFBs
When removing an anterior chamber IOFB without involvement of the crystalline lens, care should be taken to protect the corneal endothelium and lens using viscoelastic. A paracentesis can be made in a location that allows for easy access to a foreign body. The viscoelastic cannula can be used to help orient the foreign body for easier removal. The paracentesis can then be enlarged to accommodate IOFB removal. Forceps designed for foreign body removal, such as Rappazzo forceps and straight forceps, can be used to remove the IOFB. For smaller IOFBs, 23-gauge serrated or MAXgrip forceps may be used. For very small IOFBs, aspiration can be performed with a soft cannula or the vitrector. Removal of fishhook IOFBs (Figure 7) in the cornea and anterior chamber can be challenging. Depending on the size of the hook and the presence of barbs, techniques such as the back-out, advance-and-cut, and cut-and-push-through can be used to minimize anterior ocular damage.14

Lenticular IOFBs
When dealing with a lenticular IOFB it is essential to evaluate the features of the lens that can help direct the approach. A pars plana approach lensectomy and vitrectomy for lens removal is preferred if the posterior capsule is violated or if there is marked lens instability/zonular dialysis. Otherwise, IOFB removal with phacoemulsification can be performed without a concurrent vitrectomy. Due to increased risk of endophthalmitis with primary IOL placement, the authors recommend leaving the patient aphakic initially.15 Additionally, lens calculations may be inaccurate due to the surgeon’s inability to correctly perform axial length and keratometry measurements at the time of an OGI.
Posterior Segment IOFBs
The most common approach for a posterior segment IOFB is a pars plana vitrectomy and removal through either a scleral or corneal wound. The standard three-port set-up is used. If there are media or lenticular opacities obscuring the view or a choroidal detachment, a 6-mm infusion or an anterior chamber maintainer can be used. The gauge size is based on the surgeon’s preference.
The first step is to remove the vitreous to allow for manipulation of the IOFB without causing vitreous traction. Posterior vitreous detachment (PVD) induction in these patients may be difficult due to the young age of most patients. Intravitreal diluted Kenalog or Triesence may be helpful when inducing a PVD. After the vitreous is meticulously removed, attention can be directed toward the IOFB removal.
The plan for IOFB removal should be made prior to manipulating the IOFB. Cases with concurrent significant lens trauma, which require lensectomy, are good candidates for IOFB removal through the cornea. If the IOFB is not too large, a corneal limbus wound can be made to remove it. If the IOFB is very large, a scleral tunnel can be considered. Use viscoelastic to protect the corneal endothelium prior to removal of the IOFB through the cornea.
In cases with an uninvolved lens or minimal focal changes, the lens can be preserved. Such patients are good candidates for removal through an existing sclerotomy or a separate pars plana sclerotomy. Preplaced sutures in large sclerotomy wounds may facilitate quick intraocular pressure stabilization and prevent complications, such as choroidal detachment or expulsion of intraocular contents after the IOFB is removed.
After creating the wound for removal, attention can be directed toward removal of the IOFB. IOFBs may develop overlying inflammatory membranes or scar tissue that need to be removed with forceps prior to manipulating the IOFB. A range of instruments can be used to then grasp the IOFB and remove it through the wound. Options include multiple disposable forceps and reusable forceps, such as the diamond-dusted Wilson, Machemer, basket, and Rappazzo forceps. For very round IOFBs, such as a BB pellet, specific reusable and disposable BB pellet forceps are available. If those instruments are not available, the Alcon loop scraper can be used as a snare for small foreign bodies. If the foreign body is very large, a snare can be fashioned by passing a loop of Prolene suture through a blunt needle attached to a TB syringe, with the ends of the suture exiting the syringe. Moving the plunger of the syringe up and down will enlarge and tighten the snare. A 0.12-gauge forceps can be used when removing the foreign body to help open the wound more widely.
A bimanual technique also can be employed to remove the IOFB. In phakic patients this requires chandelier illumination. The IOFB can be grasped and elevated with one instrument that can safely elevate the IOFB but not easily remove it (eg, an intraocular magnet or backflush cannula). After elevation, it can be grasped by one of the aforementioned forceps and removed. In aphakic or pseudophakic patients, an alternative method is to use the initial instrument to elevate the IOFB anteriorly enough to use coaxial viewing.
After the IOFB is removed, a thorough peripheral retinal exam should be performed to look for any tears. If the IOFB was embedded in the retina, laser demarcation of the defect may be required and may be performed before or after removal of the foreign body. Any tears, breaks, or retinal detachments should be treated. If tamponade is required, air, gas, or silicone oil may all be used safely.
Scleral Buckle Placement
The role of a scleral buckle placement in patients with posterior segment IOFBs is unclear. A small study found a 24% reduced risk of retinal detachment in posterior segment IOFB patients treated with a scleral buckle at the time of IOFB removal surgery. However, this difference was not statistically significant.16
POSTOPERATIVE CONSIDERATIONS
Endophthalmitis
If the patient is noted to have endophthalmitis before or during the surgery, a vitreous and vitreous wash culture should be performed to identify the organism and obtain antibiotic sensitivity data. Broad-spectrum intravitreal antibiotics such as vancomycin and ceftazidime should be used. In cases with organic IOFBs, intravitreal antifungals can be used as well. There are some data that suggest that silicone oil may be a more beneficial tamponade for cases with endophthalmitis.16-18 Even in the absence of endophthalmitis at the time of surgery, prophylactic intraocular injections of broad-spectrum antibiotics should be considered since they have been shown to decrease the rate of traumatic endophthalmitis.19
Retinal Detachment
Patients treated with IOFB removal should be followed closely in the postoperative period for retinal detachment and PVR. Trauma is a risk factor for the development of PVR.20 In a study of metallic IOFBs, approximately 27% of patients required additional retinal detachment surgery.10
Cataract
Cataract formation is common after trauma. One study of metallic IOFBs found that 14% of patients who did not have cataract removal at the initial surgery required cataract extraction during a mean follow-up period of 180 days.10 It is important to assess for factors that may direct the surgeon toward a pars plana approach for cataract removal, including violation of the capsule and zonular dialysis.
Other
Other common posttraumatic sequelae that need to be monitored include high or low intraocular pressure, vitreous hemorrhage, and pain.10 Patients with poor vision in the affected eye should be fitted for polycarbonate lenses to protect the better-seeing eye.
Conclusion
IOFB cases are complex and require a careful history, physical exam, imaging, and presurgical planning. A variety of unique instrumentation and techniques can be used to remove the IOFBs. Patients need to be closely followed for potential post-traumatic complications, including retinal detachment and cataracts. Counseling patients about the uncertain visual prognosis and potential need for additional surgery is crucial. RP
REFERENCES
- Parver LM, Dannenberg AL, Blacklow B, Fowler CJ, Brechner RJ, Tielsch JM. Characteristics and causes of penetrating eye injuries reported to the National Eye Trauma System Registry, 1985-91. Public Health Rep. 1993;108:625-632.
- Loporchio D, Mukkamala L, Gorukanti K, Zarbin M, Langer P, Bhagat N. Intraocular foreign bodies: a review. Surv Ophthalmol. 2016;61:582-596.
- Kuhn F, Morris R. Posterior segment intraocular foreign bodies: management in the vitrectomy era. Ophthalmology. 2000;107:821-822.
- Fulcher TP, McNab AA, Sullivan TJ. Clinical features and management of intraorbital foreign bodies. Ophthalmology. 2002;109:494-500.
- Chaudhry IA, Shamsi FA, Al-Harthi E, Al-Theeb A, Elzaridi E, Riley FC. Incidence and visual outcome of endophthalmitis associated with intraocular foreign bodies. Graefes Arch Clin Exp Ophthalmol. 2008;246:181-186.
- Modjtahedi BS, Rong A, Bobinski M, McGahan J, Morse LS. Imaging characteristics of intraocular foreign bodies: a comparative study of plain film X-ray, computed tomography, ultrasound, and magnetic resonance imaging. Retina. 2015;35:95-104.
- Pinto A, Brunese L, Daniele S, et al. Role of computed tomography in the assessment of intraorbital foreign bodies. Semin Ultrasound CT MR. 2012;33:392-395.
- Deramo VA, Shah GK, Baumal CR, et al. Ultrasound biomicroscopy as a tool for detecting and localizing occult foreign bodies after ocular trauma. Ophthalmology. 1999;106:301-305.
- Williams DF, Mieler WF, Abrams GW, Lewis H. Results and prognostic factors in penetrating ocular injuries with retained intraocular foreign bodies. Ophthalmology. 1988;95:911-916.
- Ehlers JP, Kunimoto DY, Ittoop S, Maguire JI, Ho AC, Regillo CD. Metallic intraocular foreign bodies: characteristics, interventions, and prognostic factors for visual outcome and globe survival. Am J Ophthalmol. 2008;146:427-433.
- Colyer MH, Weber ED, Weichel ED, et al. Delayed intraocular foreign body removal without endophthalmitis during Operations Iraqi Freedom and Enduring Freedom. Ophthalmology. 2007;114:1439-1447.
- Scott IU, Mccabe CM, Flynn HW, et al. Local anesthesia with intravenous sedation for surgical repair of selected open globe injuries. Am J Ophthalmol. 2002;134:707-711.
- Scott IU, Gayer S, Voo I, Flynn HW Jr, Diniz JR, Venkatraman A. Regional anesthesia with monitored anesthesia care for surgical repair of selected open globe injuries. Ophthalmic Surg Lasers Imaging. 2005;36:122-128.
- Chao DL, Erickson BP, Rachitskaya AV. Penetrating ocular fishhook injury. JAMA Ophthalmol. 2015;133:347-348.
- Andreoli CM, Andreoli MT, Kloek CE, Ahuero AE, Vavvas D, Durand ML. Low rate of endophthalmitis in a large series of open globe injuries. Am J Ophthalmol. 2009;147:601-608.
- Azad RV, Kumar N, Sharma YR, Vohra R. Role of prophylactic scleral buckling in the management of retained intraocular foreign bodies. Clin Exp Ophthalmol. 2004;32:58-61.
- Bali E, Huyghe PH, Caspers L, Libert J. Vitrectomy and silicone oil in the treatment of acute endophthalmitis. Preliminary results. Bull Soc Belge Ophtalmol. 2003;288:9-18.
- Ozdamar A, Aras C, Ozturk R, Akin E, Karacorlu M, Ercikan C. In vitro antimicrobial activity of silicone oil against endophthalmitis-causing agents. Retina. 1999;19:122-126.
- Soheilian M, Rafati N, Mohebbi MR, et al. Prophylaxis of acute posttraumatic bacterial endophthalmitis: a multicenter, randomized clinical trial of intraocular antibiotic injection, report 2. Arch Ophthalmol. 2007;125:460-465.
- Cardillo JA, Stout JT, LaBree L, et al. Post-traumatic proliferative vitreoretinopathy: the epidemiologic profile, onset, risk factors, and visual outcome. Ophthalmology. 1997;104:1166-1173.








