A Checklist for EHR For Retina Practices
Electronic health records will soon be mandatory, but you can ease the transition.
RISHI P. SINGH, MD
Like it or not, electronic health record (EHR) systems are slated to become commonplace in ophthalmology over the next few years, regardless of practice setting, geographic location, or subspecialty focus.
Retina in particular faces significant obstacles to this progression based on the unique features of its practice. For example, just in the management of AMD, monthly patient visits are routine and involve the acquisition of large amounts of diagnostic and procedural documentation over the lifetime of the patient.
In addition, ophthalmologists are accustomed to manual entry methods, such as hand drawings of pathology, which are poorly emulated and time-consuming in current EHR systems.
SLOW ADAPTATION
These obstacles, among others, are why adoption for EHR systems has been poor. In 2013, the AAO reported 32% of ophthalmology practices surveyed had already implemented an EHR, 15% had implemented an EHR for some of their physicians or were in the process of implementation, and another 31% had plans to do so within two years.1 Most worrisome about this study was that 20% had experienced a significant loss of productivity following the transition.
The Health Information Technology for Economic and Clinical Health (HITECH) Act has made $27 billion available in grants to providers to help offset some of these costs, but no textbook or preferred practices exist to follow regarding how to begin this process.
Rishi P. Singh, MD, is a staff physician at the Cole Eye Institute of the Cleveland Clinic in Ohio. He reports no financial interest in any of the products mentioned here. Dr. Singh’s e-mail is singhr@ccf.org.
At the Cleveland Clinic, we’ve successfully implemented an EHR system within our practice, and this article will highlight some of the important considerations and must-have items to ensure a fruitful transition.
TIMING IS EVERYTHING
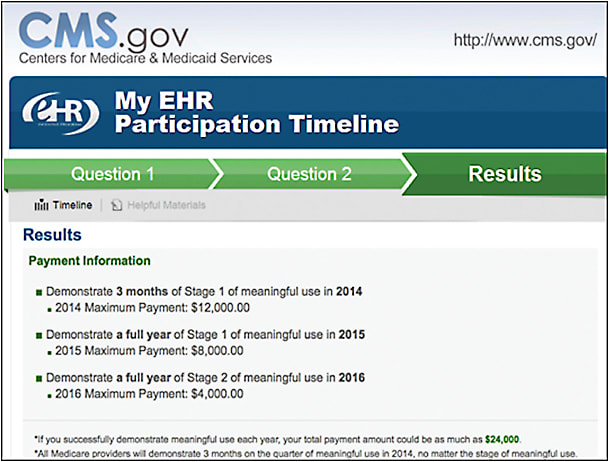
The Medicare EHR Incentive Program for eligible professionals started in 2011, and EHR incentive payments under Medicare will continue through 2016. The last year to begin participation in the Medicare EHR Incentive Program is 2014.
To qualify for Medicare EHR incentive payments, Medicare-eligible professionals must successfully demonstrate meaningful use for each year of participation in the program.
Medicare issues incentive payments to eligible professionals based on the calendar year. The reporting period for the first year consists of any 90 continuous days during the calendar year. The reporting period for all subsequent years is the entire calendar year.
Beginning in 2015, Medicare-eligible professionals who do not successfully demonstrate meaningful use will be subject to a payment adjustment. The payment reduction starts at 1% and increases each year a Medicare-eligible professional does not demonstrate meaningful use, to a maximum 5% reduction.
So if you are going to adopt this year, you must have at least 90 days of data to submit before the end of the year (Figure 1). However, no minimum number of patient encounters that you must achieve to receive remuneration through the program has been suggested.
CHOOSING THE RIGHT SYSTEM FOR YOU
The first item to consider when choosing the proper system is to make sure you are getting a government-certified product.2 It’s important to ensure that the product meets meaningful use stage 1 and 2 goals. Consider whether to partner with a hospital system or another practice, or go it alone.
Local hospital systems may offer usage of their EHR for a nominal charge, but few have ophthalmic-ready systems. The Cleveland Clinic is a certified provider of Epic Ophthalmology EMR (Epic Systems Corp., Verona, WI) to hospitals and practices for a minimal annual fee — much less than the cost of commercially available systems. A better option might be to share the cost of the IT system or to bargain collectively with the EHR vendors in cooperation with another nearby practice.
When evaluating an EHR system, determine the level of customization the system will require to fit your practice needs. Does the EHR mimic your workflow or practice pattern? Do the items within the EHR represent all the specialties within your practice? Some EHRs are retina-specific.
Finally, visit your colleagues who have successfully implemented a system to understand what their real experiences have been. We visited many sites to determine the features and functions that we wanted to implement within our own system prior to the process.
Will your existing practice management appointment system “talk” to your new EHR? How about your revenue cycle system? You may consider a different EHR product based on its compatibility with your existing systems, or you might throw everything out and start from scratch.
PUTTING YOUR SYSTEM TO WORK
Choosing the right system is only half of the job. Having a multidisciplinary team, with a physician, tech, biller/coder, and administrator, is a good first step. As a consultant to ophthalmic practices for EHR issues, I have seen the situation too many times in which a younger physician without significant practice clout or a retiring physician is chosen for this role.
Try choosing a higher-volume provider that has an established practice and is tech-savvy. Before going live, walking through the workflow on your EHR with each of these providers can help in troubleshooting early problems.
Also, consider choosing a lower-volume time of year to reduce the economic impact of the implementation process. We chose to go live in March and to reduce our schedule by only 25% for the two weeks of the launch to give our physicians adequate time to acquaint themselves with the system. By bringing the clinical volume back to normal levels more quickly, we found that many physicians began to find and employ efficiencies to keep pace.
When considering big-bang rollouts vs gradual implementations, we chose a more gradual approach, which allowed us to troubleshoot the workflow, off-load patients to another provider, and train technicians by rotating them through the clinic before their launch.
Scribes are an important consideration for any practice. Nearly every study has shown that the utility of scribes decreases significantly as a practice becomes more familiar with EMR.
However, as one doctor put it to me, “They cost a tenth of what I cost.” This risk/reward proposition of scribes is something the practice will have to determine. In our case, we chose to hire additional technicians to serve as physician extenders within the clinic. Beware that without the proper documentation of a scribe’s work in the chart or an audit trail, you put yourself at high audit risk.
BUILDING THE TOOLBOX: ESSENTIAL ELEMENTS FOR EHR
Good features can ease the bumpy road to EHR implementation, and certain functions within the system can improve your workflow and practice efficiency. When we first made the transition to EHR, our group spent several months evaluating other systems to find just the right tools. Even if they were not initially within the system, we worked with the vendors and our own IT people to implement them.
These tools can be divided into three distinct groups: improving the user experience of both providers and support staff; increasing billing capture and processing; and integrating outcomes and administrative and research activities.
Improving the User Experience
Ergonomics are a key feature for user adoption and acceptance of any EHR system. By incorporating the largest monitors possible, we were able to distribute a dense amount of information across a larger space.
We added personal computers in the hallways to mimic the normal workflow, in which a physician reviews the chart before entering the room. Placing printers in the hallways minimized the distance physicians had to travel for printed prescriptions and patient instructions. All of these items eased the anxiety of the EHR workflow to which the physicians had to convert.
Drawing is a mainstay of ophthalmology practices, and ours was no different. We first created newer pictures to represent the portions of the eye that needed or required documentation.
We were able to create numerous stencils for each of the drawing photos, which allowed for both the annotation of the image and insertion of the text into the same exam field of the patient, eliminating duplication of work. We could then place the drawings within the chart, pull it forward to a new encounter for modification, or even add a letter to another provider (Figure 2).

Figure 2. Drawing into the EHR is easier with improved pictures and stencils, and using a tablet for entry.
We improved the letter writing and documentation capabilities of our system by implementing letter templates with drop-down menus for quick annotation. By adding an auto-correct feature to our system (converting common abbreviations, such as OD to right eye), we were able to communicate better what transpired with the patients to other physicians without ophthalmic backgrounds.
Finally, by adding the capability to fax letters directly from the EHR, our physicians could maintain more rapid contact with referring providers and their caregivers.
Increasing Billing Capture and Processing
The number of procedures in retina has quadrupled in the last five years, given the increase in the medical indications. As a result, it has become increasingly difficult to track these procedures and to submit charges in an efficient fashion.
We implemented a system of charge on completion, which has improved our billing compliance, led to significantly improved documentation of patient testing and procedures, and increased our efficiency in submitting claims and sending out billings.
The physician places an order for the procedure or diagnostic test. The order then generates a form for the physician to complete. Once complete, the signature of the form submits a charge with the specific procedural or diagnostic code to our billing team to review.
Once reviewed electronically, the biller can submit the charge to the local carrier from processing. This has changed our billing cycle from weeks to two days. It has also decreased the potential for miscoding because it has completely eliminated manual entry.
Finally, it allows for a transparent review process for the indications and necessity of procedures (Figure 3, page 61).

Figure 3. Charge on completion module: Once a doctor files an order for a image, the demographics are sent downstream to the device. Once the doctor reads the image, an automatic charge is filed for the modality used.
Integrating Outcomes and Administrative and Research Activities
The Cleveland Clinic has supported an outcomes program within each institute since 2005. Past years relied on the use of manual entry and physician reporting for the outcome results, which had inherent reporting biases. When we developed the entry system for our EHR, we undertook a conscious effort to use discrete documentation whenever possible.
For example, few areas have plain text boxes for entry. Rather, buttons and check boxes are used for the documentation of imaging, procedures, and exam elements. This allows for the collection of outcomes metrics in an almost automated fashion.
In addition, using the discrete elements within our system, we created additional data streams to determine a multitude of administrative and research functions. For example, we can now monitor our usage of bevacizumab (Avastin, Genentech, South San Francisco, CA) in real time to determine whether our pharmacy needs to be restocked. We can evaluate the wait times by ophthalmology specialists in an effort to allocate the proper technician-to-physician ratios.
Finally, our practice has been able to monitor the frequency of use of our lasers and diagnostic modalities, so we can adjust schedule templates to maximize patient flow. Research has become easier with only a few clicks necessary to analyze multiple patient charts, rather than the arduous process of chart retrieval and review.
Overall, these features have allowed for the ongoing evaluation and management of the physician-patient experience. They will hopefully lead to future enhancements for both.
CONSIDER PURCHASING AN IMAGE MANAGEMENT SYSTEM
Because of HIPAA, patients will expect images of their pathologies when they walk out of your door in the years ahead. We upgraded our health records system with a new image management system to reduce the time that we spent waiting for visual field printouts and OCT scans.
We also wanted to minimize the effects on our satellite facilities of lost documents, studies buried in paper charts, and incomplete image management software. The potential for errors was high because we could not see progression when baseline images were not available. Patient review required logging in and out among multiple databases, which was very inefficient.
We decided on the Forum Eye Care Data Management system (Carl Zeiss Meditec, Jena, Germany), which stores images for multiple instruments and effectively links those images to EMR systems. With Forum, we can export a full image that can be manipulated.
We use two servers for Forum, fewer than we had for our old system. Our new system allows us to create an easier workflow, saving staff time. We benefit from one point of demographic data entry and elimination of spelling or charting errors. A standardized integration interface, directly linking our EHR to Forum, also makes a difference.
ACCOUNT FOR REFERRALS
When considering which system to use, consider how it will interact with your referring providers. Can you fax letters directly to a provider? How is the provider database loaded? Will your referring physicians receive a boilerplate document or something more useful?
Our current system allows us to send the doctor, patient, referring physician, or care team a letter with our notes from the visit. The letter template allows you to bring in drawings and exam findings directly.
In addition, we can now send OCT scans, angiographs, fundus photographs, and other images to referring doctors through our Doctor Connect system, enabled by Forum. Referring physicians are happier to receive briefer notes on their patients and view images on their progress.
CONCLUSIONS
With all of the efforts needed to navigate the process and the pitfalls along the way, why would practices choose to go forward? Having now three years of experience using EHR, it has taught me how invaluable it can be.
Patient calls can be answered quickly and efficiently. I’m communicating more than ever with referring and primary care physicians. I can perform chart reviews and clinical research studies within days and not weeks. Finally, patients have now come to expect information on demand, which EHR allows, enabling these patients to become better partners in their care. RP
REFERENCES
1. Boland MV, Chiang MF, Lim MC, et al; American Academy of Ophthalmology Medical Information Technology Committee. Adoption of electronic health records and preparations for demonstrating meaningful use: an American Academy of Ophthalmology survey. Ophthalmology. 2013;120:1702-1710.
2. Find certified EHR technology products. CCHIT website. Available at: http://www.cchit.org/find. Accessed April 9, 2014.
3. My EHR participation timeline. CMS website. Available at: http://cms.gov/Regulations-and-Guidance/Legislation/EHRIncentivePrograms/Participation-Timeline.html. Accessed April 9, 2014.








