Acute RVO: What’s Your Protocol?
Thought leaders review their treatment strategies.
STEVE LENIER, CONTRIBUTING EDITOR
As treatment options for RVO (Figure 1, page 37) continue to expand, physicians are faced with the challenge of determining the best treatment for their patients. What is best in terms of efficacy, and what is least invasive to patients? In this feature, top retina specialists discuss their protocols.
TREATMENT ORDER
At one time, use of laser was the gold standard, but that treatment has slowly been moved to the back burner. Most retina specialists are in agreement that use of an anti-VEGF agent is currently the best first-line therapy in most cases, though not with certain patients.
Antonio Capone, Jr., MD, of Associated Retinal Consultants, Royal Oak, MI, uses anti-VEGF treatment for younger, phakic patients in particular or in those that have a history of glaucoma, due to the propensity of steroids to cause cataracts and raise IOP. This is also true in a relatively young, sick patients.
For patients with dramatic vision loss or dramatic retinal thickening, Dr. Capone says, “While not common, I’ll use combination therapy, using an anti-VEGF agent and Ozurdex, particularly if in a second eye.”
Dr. Capone does imaging on the patient’s initial visit to determine the treatment order, and though he usually tries a pharmacologic approach first, he says, “I do use laser PRP for vein occlusions. Once edema resolves, I’ll use the laser to get a more even treatment.” He feels laser treatment is still useful to relieve the patient of the burden of long-term pharmacologic therapy.
Julia Haller, MD, of Wills Eye Institute, Philadelphia, PA, has a similar approach. For patients with visual loss due to acute RVO, Dr. Haller’s decision regarding treatment depends on the patient’s individual situation.
“If the patient is phakic I have a tendency to start with an anti-VEGF injection,” Dr. Haller says. “If the patient is pseudophakic and doesn’t have a history of glaucoma, I’ll also consider using a long-acting dexamethasone implant and sometimes I’ll consider trying one and then adding the other. Dexamethasone inhibits the release of VEGF and multiple inflammatory mediators. We can know very early if this treatment is going to have an effect.”
Most retina specialists are in agreement that the use of an anti-VEGF agent is currently the best first-line therapy in most cases, though not with certain patients.
Dr. Haller also takes into account how much edema the patient exhibits. “I like to get views of the periphery on fluorescein angiography (Figure 2, page 38) and see how ischemic the situation is because I also will often supplement the pharmacologic treatment with sectoral laser scatter photocoagulation,” she says.
Ron Gallemore, MD, PhD, of the Retina Macula Institute in Los Angeles, CA, explains his protocol. “For early non-edemic cases, where vision is 20/20 or 20/40, I may give them Durezol with an NSAID and topical diuretic, and that combination is effective about half the time for reducing edema in one to two weeks” he says. “If they haven’t improved at all after a week, they’ll get an anti-VEGF injection, which works 90% of the time.”

Figure 1. BRVO as demonstrated by widefield angiography. Given that more peripheral nonperfusion is visible, widefield angiography may be able to classify vein occlusions more accurately (imaged with the Optos 200 Tx).
IMAGE COURTESY OF MATTHEW M. WESSEL, MD, ANTON ORLIN, MD, AND SZILÁRD KISS, MD.
Dr. Gallemore gives patients a choice of agents. “I let them know that ranibizumab is now FDA-approved for RVO, while aflibercept is approved for CRVO, and bevacizumab is available off-label,” he says. “When appropriate, I inform them that there can be cost implications. Based on their choice, we proceed with treatment, with bevacizumab the most common choice in naïve patients. I explain that they often need multiple injections, a minimum of four, and possibly ongoing indefinitely. For patients resistant or partially responsive, we add ranibizumab, aflibercept, or Ozurdex.”
TREAT AND EXTEND
Treat-and-extend protocols may also be utilized for RVO, as with wet AMD. Dr. Gallemore says that once a decision is made to extend treatment intervals, the patient still needs to be followed closely.
“Some patients can have rebound edema and be worse off if they’re not followed closely enough,” Dr. Gallemore says. “I’ll follow patients monthly for the first six months and use Amsler grid and a near chart so they can detect when the effect of the medication is wearing off. After the edema appears well treated — usually four to six injections — we try to extend treatment from four to six weeks; if there is loss of near vision or increasing distortion before then, we reduce the interval back to four weeks.”
Patients who travel frequently by air pose another challenge. Long-distance air travel has been associated with reduced oxygen tension, which can drive VEGF production, especially in an ischemic eye, Dr. Gallemore notes. “If I know they’re taking a long flight, I try to time their injections for about a week before travel and then check them sooner than usual, at three to four weeks,” he says. “If there’s recurrent edema, it sometimes precedes vision loss, and that’s the ideal time for treatment.”
In anti-VEGF–resistant cases, Dr. Gallemore uses steroids. If a patient is resistant to the treatment after a minimum of two anti-VEGF injections, but more frequently six to eight injections, he will switch the patient to Ozurdex.
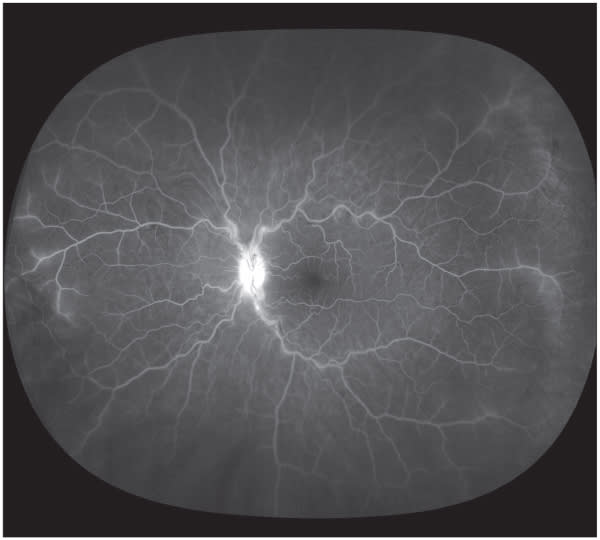
Figure 2. A widefield angiogram of a patient with nonischemic CRVO. Note the peripheral perivascular leakage that may not have been visible with traditional imaging. This patient may warrant closer follow-up (imaged with the Optos 200 Tx).
IMAGE COURTESY OF MATTHEW M. WESSEL, MD, ANTON ORLIN, MD, AND SZILÁRD KISS, MD.
He adds that in his recent clinical study (Retina, in press) for anti–VEGF-resistant patients with no response, partial response, or tachyphylaxis over time, in all cases, treatment with Ozurdex allowed the patients to recover vision.
TREATMENT WITHOUT ANTI-VEGF
For patients who decline anti-VEGF therapy or have had a stroke within the last four months, Dr. Gallemore says, “I’ll use Ozurdex or an intravitreal triamcinolone injection. I prefer Ozurdex because of its better safety profile, greater duration of action, and stronger evidence-based aid. Another advantage is that the implant may last longer — three to six months compared to three to six weeks.”
For certain patients with CRVO or recalcitrant edema, Dr. Gallemore will apply peripheral PRP laser. “Laser can sometimes reduce the need for subsequent injections, but there’s a chance of exacerbating edema because it causes VEGF release,” he says. “So you have to be cautious how and when you use laser treatment. For patients with chronic macular edema and peripheral ischemia, I document the macular leakage and peripheral ischemia at a follow-up appointment, proceed with anti-VEGF or Ozurdex injection that day, and bring the patient back for focal and PRP laser in the next one to two weeks. Pretreating with drugs before laser will blunt the post-laser VEGF spike that can occur and reduce the intensity of laser treatment required, and the pretreatment FA allows us to see the areas of leakage (Figure 3, page 40), which are suppressed by the injection itself.”
He adds, “I also use pre-anti-VEGF OCT to guide laser in some cases. I’ve been underwhelmed by the efficacy of laser compared to anti-VEGF and steroid, but it does play a role in the long-term management of most patients.”
Carl Regillo, MD, of Wills Eye institute, also starts with anti-VEGF treatment. “We’re treating macular edema, and we can reduce or eliminate the edema,” he says. “Probably the most effective treatment is anti-VEGF therapy, so we usually start with Lucentis, Eylea, or Avastin. Eylea showed good success in its phase 3 studies, comparable to Lucentis in the setting of CRVO-related macular edema.”

Figure 3. Ultra-wide field angiogram of a patient with branch retinal vein occlusion in the right eye (left ). The fellow eye (right) has late peripheral leakage temporally.
IMAGES ORIGINALLY APPEARED IN TSUI I, BAJWA A, FRANCO-CARDENAS V, PAN CK, KIM HY, SCHWARTZ SD. PERIPHERAL FLUORESCEIN ANGIOGRAPHIC FINDINGS IN FELLOW EYES OF PATIENTS WITH BRANCH RETINAL VEIN OCCLUSION. INT J INFLAMM. 2013;464127, REUSED UNDER A CREATIVE COMMONS LICENSE.
Through the years, Dr. Regillo has used Avastin. “That’s what most of us do,” he says. “It’s the new gold standard for initial treatment of RVO-related macular edema with decreased VA. In the vast majority of patients, we can get vision to improve, but it’s going to be frequent, multiple injections every four to five weeks or so to keep the macula dry.”
In some patients, vein occlusion can improve over time, “but most need something to keep the macula dry,” Dr. Regillo says. “So we’ll think about introducing a steroid in the maintenance phase. The options there are triamcinolone, which is effective for around three to four months, and Ozurdex, which lasts about four months or so and is comparable to triamcinolone in effect but has a lower rate of increasing pressure. If a patient has glaucoma we’re a little more reluctant to use steroids.”
Dr. Regillo points out that focal/grid laser has only been shown to be beneficial for BRVO-related edema. He will do one or two grid laser treatments after anti-VEGF therapy to deal with edema that persists or recurs.
DOWNSIDES OF STEROIDS
Two frequently mentioned concerns of steroid use are the side effect profile and the cost.
Dr. Capone points out the concern about side effects depends on the individual patient, saying, “Many don’t have any problems at all. The major issue is IOP, but many patients tolerate it well, or the pressure elevations are easy to manage.”
He says cost can present a problem if the insurer won’t approve it. “Depending on the copay, I’ll still recommend Ozurdex because I think it’s a superior therapy with less treatment burden,” Dr. Capone says.
Dr. Haller notes the side effects of the dexamethasone implant are less than triamcinolone. “With any steroid you do have more side effects to worry about than with an anti-VEGF agent. That is traded off against the advantage of longer durability and a broader range of activity,” she says.
“In a vitrectomized eye, it’s the only drug that has long durability, so it’s probably the treatment of choice there,” Dr. Haller continues. “You may have some IOP issues, but those are rare in terms of being serious problems with the dexamethasone implant, which is why I prefer it over triamcinolone injections.”
THE COST FACTOR
Dr. Haller points out that Ozurdex is less expensive than monthly anti-VEGF injection with Lucentis or Eylea, and it is roughly comparable in cost to Avastin but more than Kenalog. If a patient doesn’t have insurance, she will consider the less expensive alternative. “Luckily the less expensive off-label alternatives are reasonable choices, I think Avastin is just about as good as Lucentis,” she says. Dr. Haller has used Eylea experimentally for several years, and says it is “an excellent drug.”
Dr. Gallemore says the expense of Ozurdex hasn’t been a concern in his office and the safety profile is better than that of triamcinolone. “Given the reduced frequency, the cost is comparable or less than anti-VEGF injections given every four to six weeks,” he says. “The insurance plans have been good about coverage as long as the medical necessity is clear. There are also patient assistance programs for most on-label treatments.”
LOOKING FORWARD
Dr. Haller believes improvements in current treatment methods lie ahead. Long-acting anti-VEGF preparations are being developed that have some promise, she notes. “The anti-VEGF drugs work, so to have them available in a long-acting form would be fabulous,” she adds.
Dr. Haller also believes there will be a better understanding of exactly how and when to use laser for RVO, and that some of the drugs currently in the pipeline for macular degeneration may help for RVO as well. RP








