Advances in Laser Technology for Photocoagulation
Delivering faster, safer, more accurate treatment.

By Rishi P. Singh, MD
Laser photocoagulation is a mainstay of retinal practice, having been validated as an effective treatment for clinically significant macular edema associated with diabetic retinopathy and retinal vein occlusions in landmark studies, such as the Diabetic Retinopathy Study,1 the Early Treatment Diabetic Retinopathy Study (ETDRS)2 and the Branch Vein Occlusion Study.3
As laser technology has evolved, we have built on our clinical experience and refined our techniques so that we can deliver treatment in a faster, safer, more accurate fashion. In this article, I will discuss two important advances in laser photocoagulation technology and their impact on patient outcomes.
PATTERN SCANNING LASER
The launch of the Pascal pattern scan laser photocoagulator (Topcon Medical Laser Systems, Inc.) in 2006 marked a major breakthrough in laser treatment for retinal disease. By rapidly delivering 532 nm laser pulses (56 spots in approximately 0.6 seconds) in predetermined patterns, the Pascal photocoagulator enables physicians to target specific pathology with less scatter and to create multiple, rapid, sequential burns (see “Photocoagulation Patterns With the Pascal Laser”). The result has been reduced treatment duration and less pain for patients when compared with traditional, single-spot laser photocoagulation.
Nagpal and colleagues compared the efficacy, collateral damage and convenience of panretinal photocoagulation to treat proliferative diabetic retinopathy using a 532 nm solid-state green laser versus the yellow Pascal laser.4 In this prospective, randomized trial, 60 patients underwent panretinal photocoagulation: one eye with the green laser and the other with the Pascal laser. The researchers compared the fluence, pain using the visual analog scale, time, laser spot spread with infrared images and retinal sensitivity. They found the Pascal laser produced less collateral damage and induced similar regression of neovascularization compared with the green single-spot laser. In addition, treatment with the Pascal laser was less time-consuming and less painful for patients.
| Photocoagulation Patterns With the Pascal Laser |
The Pascal photocoagulator features the following preset patterns for various pathologies: ■ Square arrays: Proliferative diabetic retinopathy ■ Triple arcs: Retinal tears, lattice degeneration, proliferative diabetic retinopathy ■ Modified macular grid: Diffuse diabetic macular edema ■ Single-spot: Conventional photocoagulation Pattern-specific controls, such as spot spacing, enable further customization so that patterns can be matched to retinal disease states and anatomical features. |
|---|
Jain and colleagues evaluated visual acuity and OCT thickness after Pascal photocoagulation of clinically significant diabetic macular edema in 100 eyes of 70 subjects.5 At 4 months post-treatment, there was an average improvement in visual acuity of 0.060 logMAR (an improvement from 20/45 to 20/40, or approximately three ETDRS letters) and a reduction of central OCT thickness of 40 um and 37 um (spectral domain [SD] and time domain OCT groups, respectively), both of which were statistically significant. The researchers concluded that Pascal photocoagulation for clinically significant macular edema appears safe and effective in the short term.
Another advantage of the Pascal photocoagulator is that the patterns are customizable to match a patient’s retinal disease. This technology has utility for central serous chorioretinopathy and retina tears, as well as diabetic eye disease and retinal vein occlusion.
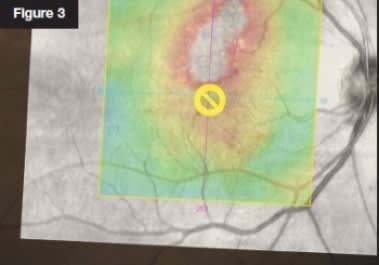
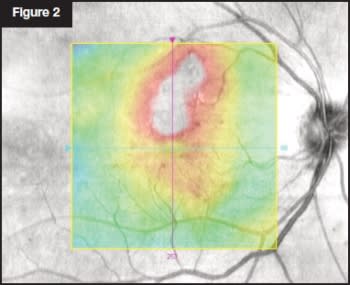
| Navigated Photocoagulation for DME | |
|---|---|
|
This 61-year-old man presented with center-involving diabetic |
|

|

|
|

|
NAVIGATED LASER PHOTOCOAGULATION
In November 2009, the U.S. Food and Drug Administration approved the Navilas laser (OD-OS GmbH) for image-guided treatment of retinal disorders. This technology is a huge leap forward, in that it replaces the standard slit-lamp delivery system with what the manufacturer calls a “navigated” system. The system integrates real-time, wide-field digital fundus imaging and computer-guided retinal photocoagulation delivery with a 532-nm laser.
The Navilas system overcomes several inherent limitations of slit-lamp delivery systems. For example, during treatment with a slit-lamp system, the surgeon must mentally superimpose treatment targets from a fluorescein angiography (FA) image onto the patient’s eye while viewing through a slit lamp and holding a contact lens. With the Navilas system, however, the surgeon can import and overlay images from various platforms, including OCT and FA, to help plan treatment. I particularly like being able to view OCT images, as OCT will detect areas of edema not visible on clinical examination. In addition, the laser tracks all eye movement so the laser application is very precisely regulated.
For optimal workflow in our office, we placed this laser in a diagnostic area rather than a treatment room. This allows for the direct importation of the OCT retinal thickness map to overlay on the fundus image taken by our photographer.
After the surgeon marks the treatment targets onto the image using the touchscreen or a mouse, he then overlays the planned treatment plan onto an image of the eye. An important safety feature, particularly for those of us who teach residents and fellows, is that you can also mark areas of the retina that should not be treated (for example, the fovea and optic nerve). A guide spot marks the fovea.
The treatment targets are then registered to the live image, which can be viewed on the monitor in true color, infrared or red-free, as well as FA. The Navilas is the only system that provides continuous imaging in all modalities at 25 frames per second. In addition, the 50-degree field of view on the monitor is pannable across the fundus. This facilitates easy treatment of peripheral retinal pathology, such as retinal tears.
Once the targets are registered to the live fundus image, the surgeon turns off the fluorescein image, leaving the live fundus view with small circles marking the laser targets. An advantage to this is that the surgeon can see the targets moving with the live fundus view on the monitor. Once treatment begins, the system continuously registers the laser to the fundus and tracks eye movement. This eye-tracking technology is an important safety feature of the Navilas. If the patient defixates or if registration is lost for some reason, the laser disarms itself. Once realignment is established, it becomes available again.
Finally, the system provides digital documentation of the entire procedure, including images of each laser application marked with circles and the laser parameters used at each location.
Several recent studies have validated the accuracy and safety of the Navilas system. Kozak and colleagues reported results from a series of cases involving 86 eyes of 61 patients with diabetic retinopathy and macular edema.6 They concluded that laser photocoagulation using the Navilas system is safe and achieves a higher rate of accuracy than standard manual-technique laser treatment. In another study, Kozak and colleagues reported results from a series of 25 consecutive eyes with perifoveal and retinovascular diseases treated with the Navilas.7 They concluded that precise retinal targeting resulted in highly accurate perifoveal laser application and no foveal damage. Six months after treatment, they identified significant decreases in central foveal thickness and significant improvements in visual acuity.
Kernt and colleagues investigated treatment-related pain and the accuracy of the Navilas system for treating clinically significant macular edema in 54 patients.8 They quantified treatment-related pain on a visual analog scale immediately after treatment and compared it with a matched control group that received conventional laser treatment. In addition, for Navilas-treated patients, the accuracy of spot placement on color images was analyzed 1 month after treatment. The investigators reported that navigated laser effects could be visualized to a high percentage on post-treatment color images, and their location showed a high concordance to targeted areas. Patients reported that treatment-related pain following Navilas laser photocoagulation was significantly lower than pain following conventional laser treatment.
SIGNIFICANT ADVANCES
Advances in laser technology, such as laser guidance systems and eye-tracking, have resulted in more accurate treatment and less pain for patients in comparison to conventional lasers. Because of these improvements, I believe there will be sustained usage in the near future. The combination of lasers with other imaging modalities in stand-alone devices, such as lasers incorporating SD-OCT, will likely follow in the coming years.
Dr. Singh is assistant professor of ophthalmology and staff physician at Cole Eye Institute, Cleveland Clinic, Cleveland, Ohio.
References
1. The Diabetic Retinopathy Study Research Group. Photocoagulation treatment of proliferative diabetic retinopathy. Clinical application of Diabetic Retinopathy Study (DRS) findings. DRS Report Number 8. Ophthalmology 1981;88:583-600.
2. Early Treatment Diabetic Retinopathy Study Research Group. Photocoagulation for diabetic macular edema. ETDRS report number 1. Arch Ophthalmol 1985;103:1796-1806.
3. The Branch Vein Occlusion Study Group. Argon laser photocoagulation for macular edema in branch vein occlusion. The Branch Vein Occlusion Study Group. Am J Ophthalmol 1984;98:271-282.
4. Nagpal M, Marlecha S, Nagpal K. Comparison of laser photocoagulation for diabetic retinopathy using 532-nm standard laser versus multispot pattern scan laser. Retina 2010;30:452-458.
5. Jain A, Collen J, Kaines A, Hubschman JP, Schwartz S. Short-duration focal pattern grid macular photocoagulation for diabetic macular edema: four-month outcomes. Retina 2010;30:1622-1626.
6. Kozak I, Oster SF, Cortes MA, et al. Clinical evaluation and treatment accuracy in diabetic macular edema using navigated laser photocoagulator NAVILAS. Ophthalmology 2011;118:1119-1124.
7. Kozak I, Kim JS, Oster SF, Chhablani J, Freeman WR. Focal navigated laser photocoagulation in retinovascular disease: clinical results in initial case series. Retina 2012;32:930-935.
8. Kernt M, Cheuteu RE, Cserhati S, et al. Pain and accuracy of focal laser treatment for diabetic macular edema using a retinal navigated laser (Navilas). Clin Ophthalmol 2012;6:289-296.








