SURGICAL PRECISION
Lens Management for Vitrectomy
The role of pars plana lensectomy in a phaco-vit world.
Steve Charles, MD, FACS, FICS
There is a common misconception that cataracts invariably follow pars plana vitrectomy. In fact, clear lenses rarely develop cataracts after PPV. There are two separate mechanisms involved in cataracts after PPV: one for nuclear sclerosis progression and another for posterior subcapsular cataracts.
Some surgeons believe that an age threshold of 40 years old, or some say 50, determines whether nuclear sclerosis will develop after PPV; in fact, the presence or absence of nuclear sclerosis is the real issue. Rapid de novo nuclear sclerosis is highly unusual.
Dr. Nancy Holekamp has shown that partial pressure of oxygen in the vitreous cavity is permanently elevated after PPV by about 10 mm Hg. Nuclear sclerosis biochemistry is well understood to be an oxidative reaction. Ascorbate levels are nine times higher in the vitreous cavity than in the serum, and ascorbate is an anti-oxidant; ascorbate levels are much lower after PPV.
Of interest is that patients with proliferative diabetic retinopathy are much less likely than nondiabetic patients to develop progression of nuclear sclerosis after PPV, probably because of oxygen consumption by a retina rendered ischemic due to retinal capillary loss.
| Steve Charles, MD, FACS, FICS, is clinical professor of ophthalmology at the University of Tennessee College of Medicine in Memphis. Dr. Charles reports significant financial interest in Alcon. He can be reached via e-mail at scharles@att.net. |
Posterior subcapsular cataracts can occur immediately after PPV secondary to a metabolic insult to the lens epithelial cells (LECs), typically due to gas bubble contact with the posterior or, occasionally, the anterior surface of the lens if gas gains access to the anterior chamber.
Simply stated, the LECs, like the corneal endothelium, “drink” aqueous. Poor-quality infusion fluid, such as lactated Ringers, and inappropriate additives, such as dextrose or bicarbonate, can damage LECs, causing posterior subcapsular cataracts. Adding dextrose to the infusion fluid was appropriate before rapid serum glucose monitoring became available; dextrose 5% in water (D5W) intravenous infusion during vitrectomy, which is used to prevent hypoglycemia, resulted in greatly elevated serum glucose, making dextrose additive necessary on an osmotic basis.
Today's diabetic patients are euglycemic during PPV; adding dextrose is inappropriate. Balance salt solution and, even better, BSS Plus, eliminate the need to add bicarbonate to the infusion fluid. There is no need to add epinephrine or antibiotics; mixing errors can occur, as well as toxicity.
COMBINED VITRECTOMY AND PHACOEMULSIFICATION
The most significant advantage of combined phacoemulsification and vitrectomy (phaco-vit) is the elimination of a second procedure. In addition, phaco-vit eliminates the issue of inadvertent lens contact during peripheral vitrectomy, especially during PPV for retinal detachment.
Although phaco-vit is convenient for the patient and reduces cost, there are a number of disadvantages. For one, visualization can become an issue if phaco is performed first. The pupil typically becomes smaller during phaco; if miosis occurs, iris hooks must be placed, which can increase the surgical complexity and cost, as well as result in postoperative inflammation.
Corneal edema and striate keratopathy, as well as ophthalmic viscosurgical devices in the anterior chamber, can interfere with visualization, which can be a real issue with ILM peeling.
If phaco is performed after PPV, the cataract may limit the view, potentially interfering with ILM peeling as well.
Refractive outcomes are less predictable with phaco-vit than with phaco performed by a high-volume refractive cataract surgeon as a separate procedure on another day. This is because effective lens position is less predictable after PPV. Vitreoretinal surgeons rarely perform enough cataract surgery to be proficient in the use of toric intraocular lenses and femtosecond laser-assisted cataract surgery, which are rapidly becoming the standard of care.
A-scan ultrasound axial length errors are significant in the presence of epimacular membrane, macular hole, or vitreomacular membrane syndrome because the A-scan cannot calculate the axial position of the fovea after vitreomacular traction or after tangential traction is removed.
If significant media opacity is present, the Humphrey IOLMaster 500 or the Haag Streit LENSTAR LS900 cannot be used because they both measure axial length from the RPE using low-coherence optical technology.
Vitreomacular surgery is a relative contraindication for phaco-vit because high visual and refractive expectations driven by modern-day refractive cataract surgery cannot be reliably achieved with this surgical approach. Phaco-vit is indicated if there is a cataract sufficient to limit visualization during non elective PPV, and it is typically indicated for diabetic tractional retinal detachments, posterior vitreoretinopathy, or giant breaks.
Posterior synechia are more common if gas bubbles are used, even with intermittent use of mydriatic agents. On occasion, gas may pass through the zonules into the anterior chamber, especially if the infusion cannula tip is allowed to tip anteriorly as fluid-air exchange is initiated.
PARS PLANA LENSECTOMY
Pars plana lensectomy is underutilized today because of the growth of phaco-vit. A one-compartment eye is essential for severe uveitis, phakic endophthalmitis, a traumatic cataract with a nonintact capsule plus retinal detachment, intraocular foreign bodies, or vitreous hemorrhage. A highly inflamed one-compartment eye with all of the lens capsule removed is much less likely to develop a cyclitic membrane, hypotony, or phthisis than a two-compartment eye or an aphakic eye with a capsule.
Highly myopic eyes with vitreomacular traction syndrome, macular schisis, or retinal detachment with PVR or giant breaks are ideal cases for pars plana lensectomy (PPL); these are often best left aphakic. Large refractive errors are common if phaco-vit and IOL implantation are utilized in these cases because of posterior staphyloma and calculation complexity.
Traditionally, the first step in PPL was to insert the MVR blade through the equator of the lens into the nucleus — a very bad idea. Many years ago, I adapted the techniques used in phaco to PPL. The first step in what I call endocapsular lensectomy is to perform an anterior vitrectomy and capsulorhexis with the vitreous cutter (Figure 1). This can be followed by hydrodissection performed through the posterior capsule rhexis (Figure 2).

Figure 1. Posterior capsulorhexis is performed with the vitreous cutter after anterior vitrectomy to prevent engagement of vitreous in the fragmenter.

Figure 2. Cortical cleaving hydrodissection is performed with a blunt 27-g cannula attached to a 3- to 5-mL syringe via a short length of tubing.
The fragmenter should be used at full power with continuous aspiration and sonification because aspiration without sonification causes plugging, and sonification without aspiration rapidly causes scleral burns. The fragmenter tip should be positioned in the equatorial plane of the lens, staying away from anterior and posterior capsule. Drilling into the lens and then pulling back while sonification is activated will allow lens material to be aspirated without plugging.
Remove all of the lens capsule with end-gripping forceps with serrated teeth by zonulorhexis if there is florid neovascularization, severe inflammation, or a scleral laceration nears the pars plicata (Figure 3). Removal of all of the capsule is not possible using the vitreous cutter; the forceps method is safer and more effective. Removal of the entire capsule reduces cyclitic membrane formation, hypotony, phthisis, concave iris secondary to iris-capsule synechia, and capsule-anterior adherence leading to vitreous base traction.
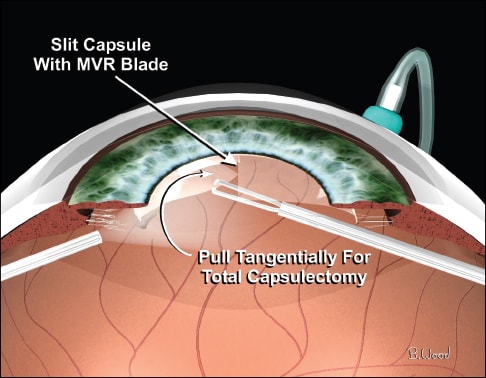
Figure 3. Zonulorhexis is performed in a circular fashion with the ILM or end-grasping forceps.
Capsule retention is indicated if there is no inflammation, infection, or neovascularization and the intent is to perform IOL implantation, either at time of surgery or at a later date. Although the intact capsule can retain silicone oil in the vitreous cavity, rapid and marked fibrous proliferation invariably occurs, rendering the capsule opaque.
This technique can buy time until the oil can be removed, but often fibrous PCO is so marked that the retina can be visualized, and B-scan ultrasonic imaging is ineffective with silicone oil in the vitreous cavity.
SUMMARY
PPL is a powerful technique that must be part of the vitreoretinal surgeon's armamentarium. Use of phaco-like techniques for lensectomy is superior to traditional methods. Phaco-vit is a crucial technique for vitreoretinal surgeons but is often overutilized because of the false belief that PPV always causes cataracts. Phaco-vit simply does not provide the refractive outcomes patients expect and deserve. RP