Case Study
Meningitis Without Papilledema
An HIV-positive patient presents with an inflamed retina and choroid, as well as scattered intraretinal hemorrhages.
Frank Ruda, MD • Nancy Kunjukunju, MD • Anthony Mazzulla, MD
Cryptococcus neoformans, an encapsulated yeast, causes a primary lung infection, with secondary meningitis being the most recognized clinical manifestation among individuals with cell-mediated immunodeficiency.1 Secondary ocular involvement usually occurs after CNS infection via hematogenous dissemination or extension from the meninges or optic nerve.2 Intraocular manifestations may include vitritis, chorioretinitis, neuroretinitis and endophthalmitis.1 We present a patient with bilateral multifocal chorioretinitis due to disseminated cryptococcal infection.
CASE REPORT
A 54-year-old HIV-positive African-American male was admitted to the hospital for altered mental status. His initial viral load was 558,883 copies/mL and absolute CD4 T-cell count was found to be 8/µL.
Ophthalmology was consulted due to blurry vision. Visual acuity and confrontational visual fields were unable to be assessed. Pupils were reactive and without afferent pupillary defect. Applanation tonometry was normal. The anterior segment was quiet OU, and there was no vitritis. The dilated fundus exam revealed a bilateral multifocal choroiditis with posterior retinitis and scattered intraretinal hemorrhages OU (Figures 1 and 2).

Figure 1. Right eye: Multifocal choroiditis and retinal hemorrhages, fundus photo (left) and red-free (right).
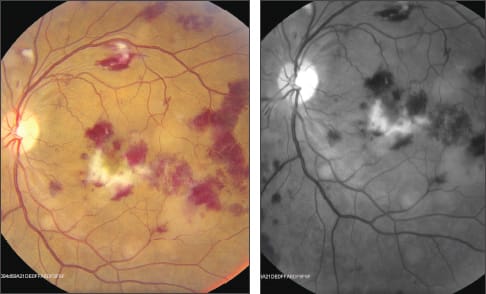
Figure 2. Left eye: Multifocal choroiditis and retinal hemorrhages, fundus photo (left) and red-free (right).
Lumbar puncture was performed with a documented opening pressure of 55 mm Hg. Cerebral spinal fluid (CSF) studies came back positive for heavy yeast, and subsequent CSF and blood cultures were positive for C. neoformans.
An infectious-disease specialist was consulted, and treatment consisted of intravenous amphotericin B and flucytosine. After four weeks of antifungal therapy, chorioretinal findings had diminished, and CSF cultures exhibited no growth (Figures 3 and 4, shown below).

Figure 3. Right eye showing improvement of choroiditis and diminished retinal hemorrhages, fundus photo (left) and red-free (right).

Figure 4. Left eye showing improvement of clinical picture and partial regression of retinitis, fundus photo (left) and red-free (right).
DISCUSSION
Ocular involvement is a rare sequela of cryptococcal meningitis, occurring in only 6% of patients.1 The most common ocular manifestation is papilledema.3 Our patient presented with a rare combination of multifocal choroiditis, retinitis and scattered intraretinal hemorrhages. RP
REFERENCES
1. Carney MD, Combs JL, Waschler W. Cryptococcal choroiditis. Retina. 1990;10:27-32.
2. Bisseru B, Bajaj A, Carruthers RH, Chhabbra HN. Pulmonary and bilateral retinochoroidal cryptococcosis. Br J Ophthalmol. 1983;67:157-161.
3. Kestelyn P, Taelman H, Bogaerts J, et al. Ophthalmic manifestations of infections with Cryptococcus neoformans in a patient with the acquired immunodeficiency syndrome. Am J Ophthalmol. 1993;116:721-727.
| Frank Ruda, MD, is a resident, and Nancy Kunjukunju, MD, and Anthony Mazzulla, MD, are on the faculty of the Oschner Clinic in New Orleans. None of the authors report any financial interest in any products mentioned here. Dr. Kunjukunju can be reached at nkunjukunju@gmail.com. |








