Case Study
Conservative Treatment of Ciliary Body Melanoma With Extraocular Extension
Plaque radiotherapy allowed this patient to avoid enucleation.
EMILY KOLBUS ∙ CARLOS BIANCIOTTO, MD ∙ CAROL L. SHIELDS, MD
Extraocular extension (EOE) of uveal melanoma is uncommon, affecting only a minority of patients.1-4 In the Collaborative Ocular Melanoma Study of 1,639 eyes with large- and medium-sized tumors undergoing enucleation, 98 (6%) had microscopic evidence of extrascleral extension.2 An analysis from Liverpool, United Kingdom, found EOE in 124 (15%) of 847 eyes that came to enucleation.4
Extraocular extension can appear on the surface of the globe in either the anterior or posterior segment of the eye. In the anterior segment, EOE is clinically visible as a brown sub-Tenon's fascia mass overlying the ciliary body; in the posterior segment, EOE is generally not clinically visible but is detectable with ultrasound or magnetic resonance imaging. Hosten and associates analyzed 70 eyes with EOE from uveal melanoma and found that MRI was better for detecting posterior EOE than ultrasonography.3
Extraocular extension is a known factor predictive of poorer survival prognosis.4,5 This finding is attributed to the correlation of EOE with various risk factors, such as larger tumor dimensions and more advanced disease, epithelioid cell type, closed loops on pathology, higher mitotic rates and monosomy of chromosome.3,4,5 Herein, we report on a patient with EOE who was managed conservatively with plaque radiotherapy.
| All authors are affiliated with the ocular oncology service at Wills Eye Institute in Philadelphia. Emily Kolbus is a student, Carlos Bianciotto, MD, is a fellow and Carol L. Shields, MD is co-director of the oncology service. The authors have no financial interest in any products mentioned. However, research support for this article was provided by the Eye Tumor Research Foundation, also located in Philadelphia. Dr. Shields can be contacted at carol.shields@shieldsoncology.com. |
CASE DESCRIPTION
A 77-year-old Caucasian male noticed a slowly enlarging spot on his right eye for 11 months. His past medical history included prostate cancer that had remained untreated due to low prostatic-specific antigen levels and inactivity, as well as non–insulin-dependent diabetes and hypertension.
On ocular examination, visual acuity was 20/25 OD and 20/40 OS. Intraocular pressures were 15 mm Hg in both eyes. The OS was unremarkable; findings were limited to the right eye. The anterior segment OD showed a posterior chamber intraocular lens and a pigmented lesion near the limbus superonasally underlying Tenon's fascia and conjunctiva, measuring 3 mm x 2 mm x 1 mm. Dilated ectatic sentinel vessels were noted. Transillumination revealed a circumscribed shadow involving the anterior chamber angle, ciliary body, and choroid measuring 12 mm in diameter. Gonioscopy confirmed angle infiltration by pigmented tumor between 1 and 2 o'clock.
Fundus exam OD disclosed a pigmented, dome-shaped ciliochoroidal mass superonasally measuring 12 mm in diameter by 5.4 mm in thickness without associated sub-retinal fluid or orange pigment. Ultrasonography confirmed an acoustically solid mass with medium internal reflectivity. These findings were consistent with ciliochoroidal melanoma with extraocular extension OD.
Options for management included enucleation, full-thickness eye-wall resection followed by scleral graft, or plaque radiotherapy. The tumor was treated with custom-designed I125 plaque radiotherapy with a dose of 8,000 cGy to the intraocular tumor apex and 32,900 cGy to the EOE over a four-day period. At the time of surgery, the EOE was not disturbed and the plaque was placed over the EOE with overlying local conjunctiva and Tenon's fascia intact.
Two years following plaque radiotherapy, the tumor showed complete regression to a thickness of 1.8 mm. The area of extraocular extension had decreased substantially to an atrophic area. Visual acuity remained 20/20 and there was no metastatic disease.
DISCUSSION
The treatment of uveal melanoma with EOE generally hinges on the extent of EOE and the intraocular tumor size. With massive EOE over 4 mm thick and large uveal melanoma of over 12 mm thickness, enucleation is generally offered. For smaller tumors, plaque radiotherapy can provide excellent control.6-8
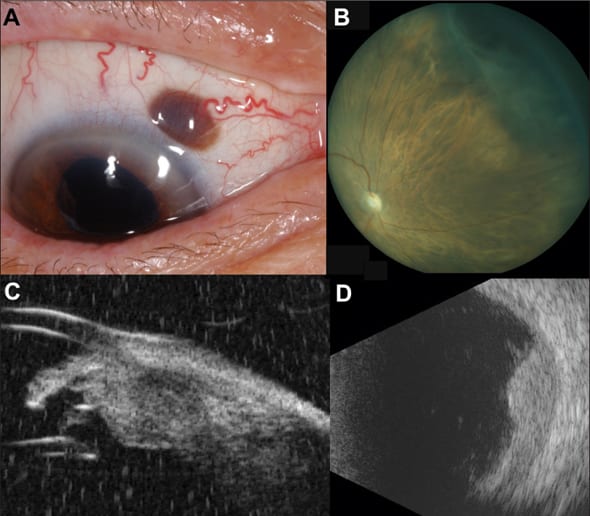
Figure 1. Extraocular extension of ciliary body melanoma before treatment: (A) EOE is noted superonasally, with an associated sentinel vessel. (B) Panoret photograph depicting the ciliary body melanoma superonasally. (C) Ultrasound biomicroscopy demonstrating the ciliary body mass with a small area of scleral thickening corresponding to the EOE. (D) B-scan ultrasound with a dome-shaped mass corresponding to the melanoma.
Gündüz and associates reported on 17 eyes with clinically evident extraocular extension (less than 3 mm thickness) from uveal melanoma that were treated with plaque radiotherapy.7 A median dose of 9,000 cGy to the apex of the intraocular component and 35,000 cGy to the EOE was administered.7 Both intraocular and extraocular tumor components showed complete control and the EOE showed regression with an average decrease of 1 mm in thickness. All patients retained the globe without local recurrence over median follow-up of five years, and systemic metastases were detected in three cases (18%). The final visual acuity was better than 20/40 in five eyes (29%) and better than 20/100 in 10 (59%). Cataract developed in seven eyes (41%) and neovascular glaucoma in two (12%). Importantly, the sclera remained intact without signs of necrosis.7
Bellmann and collaborators reviewed a series of 67 eyes with extraocular extension from uveal melanoma and noted that tumor recurrence and survival rates were similar in those receiving conservative eye treatment (proton beam or plaque brachytherapy) as compared to enucleation after a median follow-up of 38 months.8 Hence, plaque radiotherapy is a popular alternative to enucleation for tumors with small degrees of extraocular extension <3 mm in thickness.
In the long term, these patients are at risk for complications of plaque radiotherapy, such as maculopathy, papillopathy and cataract, leading to a decrease in visual acuity.9-10 The most important factors affecting visual acuity following plaque radiotherapy include increasing tumor thickness, worse initial visual acuity, proximity to foveola less than 5 mm, age greater than 60 years, subretinal fluid, diabetes mellitus, and hypertension.9-10
In a report by Shields and colleagues, long-term visual acuity in 1,106 consecutive patients with plaque-irradiated uveal melanoma, 68% of affected eyes demonstrated poor visual acuity by 10 years.10 The best vision results were seen in those patients with small tumors further than 5 mm from the optic disc or foveola.10 Therefore, patients with ciliary body melanoma, even those with EOE, could benefit from conservative plaque radiotherapy with tumor control, EOE control and relative visual acuity preservation. RP

Figure 2. Following treatment, the tumor and EOE have regressed: (A) Two years after plaque radiotherapy, the EOE has regressed to flat pigment. (B) High-power view of the involved area. (C) B-scan ultra-sonography demonstrating a flat scar in the area of the regressed melanoma. (D) Funduscopic visualization of the flat, regressed melanoma scar.
REFERENCES
1. Shields CL, Furuta M, Thangappan A, et al. Metastasis of uveal melanoma millimeter by millimeter in 8033 consecutive eyes. Arch Ophthalmol. 2009;127:989-998.
2. Collaborative Ocular Melanoma Study Group; Boldt HC, Byrne SF, Gilson MM, et al. Baseline echographic characteristics of tumors in eyes of patients enrolled in the Collaborative Ocular Melanoma Study: COMS report no. 29. Ophthalmology. 2008;115:1390-1397.
3. Hosten N, Bornfeld N, Wassmuth R, et al. Uveal melanoma: detection of extraocular growth with MR imaging and US. Radiology. 1997;202:61-67.
4. Coupland SE, Campbell I, Damato B. Routes of extraocular extension of uveal melanoma: risk factors and influence on survival probability. Ophthalmology. 2008;115:1778-1185.6.
5. Heindl LM, Hofmann TN, Adler W, et al. Intraocular tumor-associated lymphangiogenesis a novel prognostic factor for ciliary body melanomas with extraocular extension? Ophthalmology. 2010;117:334-342.2.
6. Blanco G. Diagnosis and treatment of orbital invasion in uveal melanoma. Can J Ophthalmol. 2004;39:388-396. Review.
7. Gündüz K, Shields CA, Shields JA, Cater J, Brady L. Plaque radiotherapy for management of ciliary body and choroidal melanoma with extraocular extension. Am J Opthalmol. 2000;130:97-102.
8. Bellmann C, Lumbroso-Le Rouic L, Levy C, et al. Uveal melanoma: management and outcome of patients with extraocular spread. Br J Ophthalmol. 2010; 94:569-5748.
9. Gündüz K, Shields CA, Shields JA, et al. Radiation complications and tumor control after plaque radiotherapy of choroidal melanoma with macular involvement. Am J Opthalmol. 1999;127:579-589.
10. Shields CA, Shields JA, Cater J, Gündüz K, et al. Plaque radiotherapy for uveal melanoma: long-term visual outcome in 1106 consecutive patients. Arch Ophthalmol. 2000;118:1219-1228.








