Progression and Regression of Retinoschisis in a Single Patient
HARVEY LINCOFF, MD ∙ VIMAL SARUP, MD ∙ DOMINIK URAM, MD ∙ INGRID KREISSIG, MD
Senile retinoschisis is a shallow elevation of the inner layers of the retina. It is asymptomatic, is usually nonprogressive, and yields an absolute scotoma that persists even if it regresses. Senile retinoschisis can be mistaken for retinal detachment, especially if there is a hole in the inner layers that is appropriately placed for the elevation, if it were of rhegmatogenous origin.1
This is a report about an eye with bullous retinoschisis with an appropriately placed retinal hole that was operated upon but progressed over 22 months, and then with out further treatment re gressed over 13 years, leaving an absolute scotoma the size of its former maximum ex tent. Byer has reported ex tension and regression in separate patients.2
CASE REPORT
A 38-year-old female was referred for an asymptomatic retinal elevation in the left eye. She was a moderate myope; her visual acuity was 20/20 in each eye through contact lenses. Fundus examination revealed a semitransparent, bullous elevation of the retina in the superotemporal quadrant with a round retinal hole at 1 o'clock (Figure 1). It looked like retinoschisis, but because the hole was appropriately placed for a rhegmatogenous detachment, the hole was tested with a laser application through the hole (Figure 2) and subsequently with a balloon buckle.3-5 Both tests confirmed retinoschisis. The patient was made aware of her inferonasal field defect and was asked to report any extension of it.

Figure 1. The presenting retinal elevation in the superotemporal quadrant of the left eye with an inner layer hole at 1 o'clock. The visual acuity is 20/20.

Figure 2. A laser test for retinoschisis performed through the break at 1 o'clock was positive and similar to the control burn in adjacent attached retina at the same latitude as the break.
Four months later, an examination revealed that the retinal elevation had asymptomatically extended inferiorly to 4 o'clock (Figure 3). Over the following 18 months, it further extended posteriorly and inferiorly to 6 o'clock.

Figure 3. Circumferential extension of the retinal elevation to 4 o'clock noted four months after initial presentation.
The extension was asymptomatic; it approached but did not invade the macula. A biomicroscopic examination revealed retinal defects — possible breaks in the periphery at 2.45, 3.45, and 5.15 o'clock (Figure 4). Binocular occlusion for 48 hours did not alter the shape or extent of the retinal elevation.

Figure 4. Further circumferential and posterior extension of the elevation 22 months after the initial exam. Three possible breaks are noted at 2.45, 3.45 and 5.15 o'clock. The macula is still intact and visual acuity was maintained at 20/20.
Because the macula was threatened, the possibility of retinal detachment was reconsidered and cryopexy and a circumferential buckle were applied to close the hole, at 1 o'clock and the three possible breaks below. Postoperatively, there was no change in the extent of the retinal elevation, and it was concluded that the extended elevation was indeed retinoschisis (Figure 5).

Figure 5. A circumferential buckle was placed after cryo application to the break at 1 o'clock and the three possible breaks 22 months after the initial examination.
Over the next year, there was some regression of the superior border of the retinal elevation (Figure 6). An examination 21 months later revealed further regression of the retinoschisis (Figure 7). An examination 62 months later revealed that the retinal elevation had further regressed, leaving only a thin rim of retinoschisis adjacent to the buckle (Figure 8).

Figure 6. Six months after the buckle, an examination revealed some regression at the superior pole of the retinal elevation.
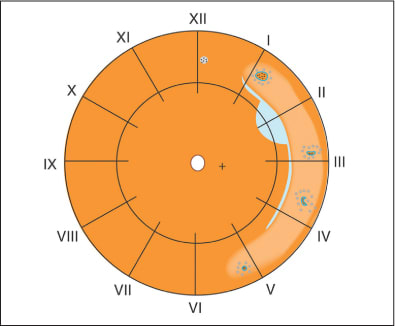
Figure 7. Additional regression of retinoschisis 27 months after surgery.

Figure 8. Further regression of retinoschisis observed 41 months after the buckle surgery. A thin rim of retinoschisis was still present at the posterior edge of the buckle.
When last seen, 15 years after the initial examination, the retina was completely attached. A visual field revealed an absolute scotoma consistent with the extent of the former extended schisis elevation (Figure 9). Optical coherence tomography confirmed retinal atrophy temporal to the macula (Figure 10).

Figure 9. A visual field examination 12.5 years after surgery revealed an absolute scotoma consistent with the extent of the retinal elevation at the time of surgery.

Figure 10. OCT revealed atrophic retina temporal to the macula.
DISCUSSION
The case was a diagnostic and therapeutic challenge because the retinal elevation had features of retinoschisis and retinal detachment. The presenting retinal elevation in the superotemporal quadrant was asymptomatic. The elevation shape was consistent with the position of the retinal hole, if it were a rhegmatogenous detachment. This prompted laser testing of the hole, which was positive for retinoschisis.
The subsequent progression, though asymptomatic, was cause for concern, and the finding of three inner layer retinal defects in the periphery of the extended retinal elevation reinforced the suspicion of retinal detachment. That the extended elevation through the temporal retina did not invade the macula was puzzling and contraindicated the diagnosis of rhegmatogenous retinal detachment. The failure of the retina to attach after the breaks were buckled was further evidence that the elevation was not rhegmatogenous but retinoschisis.
Progression is a recognized but infrequent feature of retinoschisis.6,7 Regression of retinoschisis is rare.8 In our patient, progression occurred over 22 months and regression took 13 years. It is unlikely that the placement of the buckle in any way modified the course of retinoschisis. It is noteworthy that the entire course, occurrence, progression, and regression were asymptomatic. This is a cardinal feature of retinoschisis that is frequently overlooked. RP
| Harvey Lincoff, MD, Vimal Sarup, MD, Dominik Uram, MD, and Ingrid Kreissig, MD all practice ophthalmology at New York Presbyterian Hospital-Weill Cornell Medical Center in New York. Dr. Kreissig is also affiliated with the University of Mannhein-Heidelberg, Germany. None of the authors reports any financial interest in any products mentioned in this article. Dr. Uram can be reached at dtu2101@columbia.edu. |
REFERENCES
- Lincoff H, Gieser R. Finding the retinal hole. Mod Probl Ophthalmol 1972;10:78-87
- Byer NE. Spontaneous regression of senile retinoschisis. Arch Ophthalmol. 1972;88:207-209.
- Lincoff H, Kreissig I, Stopa M. A modified laser test for the identification of retinoschisis. American Journal of Ophthalmology. 2003;136:925-926.
- Kingham JD. Retinal detachment masquerading as retinoschisis. Annals of Ophthalmology. 1981:13:849-851.
- Lincoff H, Kreissig I, Hahn YS. A temporary balloon buckle for the treatment of small retinal detachments. Ophthalmology 1979;86:586-92.
- Schepens CL. Retinoschisis. In: Schepens CL. Retinal Detachment and Allied Diseases. Vols 1 and 2. Philadelphia, PA: Saunders; 1983:216-222, 557-587.
- Byer NE. The natural history of senile retinoschisis. Mod Probl Ophthalmol. 1977;18:304–311.
- Byer NE. Long-term natural history study of senile retinoschisis with implications for management. Ophthalmology. 1986;93:1127–1137.








