PHOTO ESSAY
Complete Spontaneous Resolution of Full-thickness Macular Hole With OCT-documented Restoration of Normal Foveal Contour
ELAD MOISSEIEV, MD • DAFNA GOLDENBERG, MD • ADIEL BARAK, MD • ANAT LOEWENSTEIN, MD
Macular holes are a common retinal pathology, occurring primarily in elderly patients and more frequently in women. They are usually unilateral. The vast majority of macular holes are idiopathic, but they can appear in myopic eyes and after trauma.1 Patients with macular holes usually complain of metamorphopsia and central vision loss.
| Elad Moisseiev, MD, Dafna Goldenberg, MD, Adiel Barak, MD, and Anat Loewenstein, MD, all practice in the Department of Ophthalmology at the Tel Aviv Sourasky Medical Center in Israel and the Sackler School of Medicine, also in Tel Aviv. The authors report no financial interest in any products mentioned in this article. Dr.Moisseiev may be reached via e-mail at eladmoi@netvision.net.il. |
STAGING
The severity of symptoms is in direct correlation with the stage of the macular hole.1 As first hypothesized by Gass,2 it is currently believed that macular holes are caused by vitreal traction on the macula during the natural course of age-related posterior vitreous detachment (PVD). As suggested and later revised by Gass,2,3 macular holes were commonly classified into four stages. Stage 1, also known as an "impending macular hole," was characterized by a foveal cyst within the retina. Stages 2 through 4 included full-thickness macular holes, which were further divided into smaller holes 400 μm in diameter (stage 2), holes larger than 400 μm in diameter (stage 3), and with complete PVD (stage 4).
The advances in optical coherence tomography (OCT) technology have made it a most valuable tool for the detection and staging of macular holes.1 It has shown that, as suggested by Gass,3 macular holes are caused by tangential vitreomacular traction and represent displacement of photoreceptors, rather than being areas of photoreceptor loss due to anteroposterior tractional forces and retinal tissue loss.1,4 OCT has improved the understanding of macular hole pathophysiology and has even led to the creation of a new OCT-based classification: Stage 1 macular holes include an OCT-documented intraretinal cyst or splitting. As above, these are "impending macular holes." Stage 2 macular holes are full-thickness holes, with OCT-documented vitreal traction. Stage 3 macular holes are full-thickness holes, with OCT-documented PVD, with or without an operculum.4
It has been clinically established that stage 1 impending macular holes have a 50% chance for spontaneous closure with resolution of symptoms1 and are therefore observed and not treated surgically. Closure of full-thickness macular holes is less frequent; therefore, these cases are usually treated surgically by pars plana vitrectomy, with or without ILM peeling, and gas or silicone tamponade. The Vitrectomy for Macular Hole trial reported a 16% spontaneous closure rate of grade 2 holes5 and a 4% spontaneous closure rate of grade 3 and grade 4 holes. It is important to note that, in this trial, closure was defined only as flattening of the edges.
Spontaneous resolution with hole closure and a restoration of the normal foveal contour is very rare in full-thickness macular holes (stages 2 through 4). Kakehashi et al. reported this occurrence in one of 17 eyes with grade 2 macular hole,6 Hikichi et al. found no such resolution in 48 eyes with grade 2 macular hole,7 and Casuso also reported a series of 15 eyes in which such resolution did not occur during five years of follow-up.8
A CASE OF SPONTANEOUS CLOSURE
We report on a 62-year-old female patient who presented with a grade 2 macular hole in her left eye. Visual acuity in the affected eye was 20/200. Spectralis HR-OCT demonstrated the full-thickness hole with vitreal traction on the attached operculum and also elevation of the photoreceptor layer (Figure 1). Best corrected visual acuity in the right eye was 20/50. Spectralis HROCT demonstrated vitreomacular traction and a small foveal cyst, consistent with a grade 1 macular hole (Figure 2).
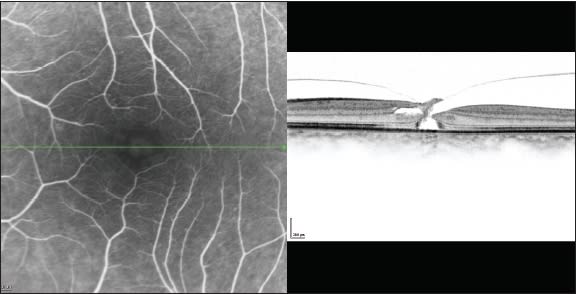
Figure 1. Spectralis HR-OCT of the left eye upon presentation, demonstrating a full-thickness macular hole smaller than 400 μm in diameter, with vitreal traction on the attached operculum (consistent with grade 2) and elevation of the photoreceptor layer.
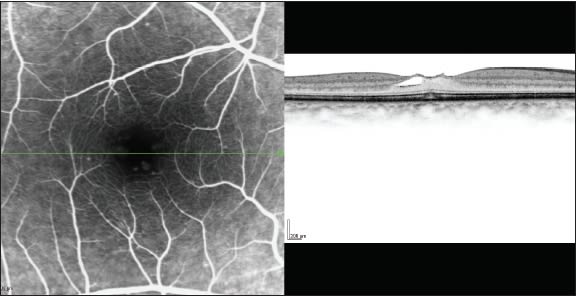
Figure 2. Spectralis HR-OCT of the right eye upon presentation, demonstrating vitreomacular traction and a small foveal cyst (consistent with a grade 1 impending macular hole).
Three months later, there was no change in metamorphopsia in the left eye and visual acuity was stable at 20/200, but upon examination, it seemed that the hole was closed. Stratus OCT demonstrated complete PVD with closure of the macular hole in the left eye. Foveal contour returned to an almost normal configuration, and a small subretinal cyst, photoreceptor discontinuity, and an operculum attached to the detached vitreous are all that remained of the once full-thickness macular hole (Figure 3). Over five months of follow-up, visual acuity of the left eye improved to 20/50, and Spectralis HR-OCT demonstrated almost complete absorption of the cyst and restoration of the normal foveal contour. Only a subtle discontinuity of the photoreceptor layer was still noticeable — a fact that may explain the still decreased visual acuity (Figure 4). The right eye remained unchanged during this period.

Figure 3. Stratus OCT of the left eye at the time of the scheduled surgery, demonstrating complete PVD with closure of the macular hole, restoration of an almost normal foveal contour, a small subretinal cyst, photoreceptor discontinuity, and an operculum attached to the detached vitreous.

Figure 4. Spectralis HR-OCT of the left eye after five months, demonstrating almost complete absorption of the cyst, restoration of a normal foveal contour, an operculum, and a remaining subtle discontinuity of the photoreceptor layer.
CONCLUSION
As documented by Spectralis HR-OCT, these images depict a rare clinical course of a grade 2 full thickness macular hole, regressing almost completely over a period of five months, with significant improvement of visual acuity. RP
REFERENCES
- La Cour M, Friis J. Macular holes: classification, epidemiology, natural history and treatment. Acta Ophthalmol Scand. 2002;80:579-587.
- Gass JD. Idiopathic senile macular hole. Its early stages and pathogenesis. Arch Ophthalmol. 1988;106:629-639.
- Gass JD. Reappraisal of biomicroscopic classification of stages of development of a macular hole. Am J Ophthalmol. 1995;119:752-759.
- Hee MR, Puliafito CA, Wong C, et al. Optical coherence tomography of macular holes. Ophthalmology. 1995;102:748-756.
- Kim JW, Freeman WR, Azen SP, el-Haig W, Klein DJ, Bailey IL. Prospective randomized trial of vitrectomy or observation for stage 2 macular holes. Vitrectomy for Macular Hole Study Group. Am J Ophthalmol. 1996;121:605-614.
- Kakehashi A, Schepens CL, Akiba J, Hikichi T, Trempe CL. Spontaneous resolution of foveal detachments and macular breaks. Am J Ophthalmol. 1995;120:767-775.
- Hikichi T, Yoshida A, Akiba J, Konno S, Trempe CL. Prognosis of stage 2 macular holes. Am J Ophthalmol. 1995;119:571-575.
- Casuso LA, Scott IU, Flynn HW Jr, et al. Long-term follow-up of unoperated macular holes. Ophthalmology. 2001;108:1150-1155.
- Ezra E. Idiopathic full thickness macular hole: natural history and pathogenesis. Br J Ophthalmol. 2001;85:102-108.








