technology
New
Technology Allows for Earlier Detection of Pre-CNV
Next-generation
PHP offers more comprehensive reporting for reliable test results.
ROCHELLE NATALONI, CONTRIBUTING
WRITER
Preferential hyperacuity perimetry is less familiar to retinal specialists than to their general ophthalmology counterparts — but not for long. Users say the technology, which monitors progression in age-related macular degeneration (AMD) patients and detects recent-onset choroidal neovascularization (CNV), will likely become integral to the management and comanagement of AMD.
Preferential hyperacuity perimetry (PHP) uses a form of perimetry that is similar to Humphrey visual fields testing, but instead of using white-on-white stimuli, it is based on Vernier hyperacuity — or the ability to perceive minute differences in the relative spatial localization of 2 objects in space.
"Regular monitoring with PHP affords more accurate and timely referrals and identifies those patients who can best be helped by treatment," says retinal specialist Nalin Mehta, MD, of the Colorado Retina Center in Denver. Dr. Mehta, who has worked with the device in his practice since its early developmental phase, says, "It enables intervention when treatment is most effective in preserving vision."
|
|
|
The new Foresee PHP from Notal Vision/MSS. |
WHAT DOES PHP DO?
Preferential hyperacuity perimetry maps and quantifies visual field defects consistent with the progression of intermediate dry AMD to the wet stage of the disease. By overcoming the brain's ability to compensate for small visual field defects, PHP can identify CNV lesions while in development and the patient still has good vision, allowing intervention when treatment is most effective. A study of 185 patients, by the Preferential Hyperacuity Perimetry Research Group, found that PHP testing can both detect recent-onset CNV resulting from AMD and differentiate it from intermediate AMD with high sensitivity and specificity.
The group reported that monitoring with PHP should detect most recent-onset CNV with few false-positive results at a stage when treatment usually would be beneficial and concluded that this monitoring should be considered in the management of the intermediate stage of AMD. Furthermore, the researchers added that the use of baseline and serial PHP testing may obviate the need for fluorescein angiography (FA) in some patients who have persistent symptoms suggestive of neovascular AMD, such as metamorphopsia, even when the clinical examination shows no obvious features of neovascular AMD.1
BENEFITS OF PHP
|
|
|
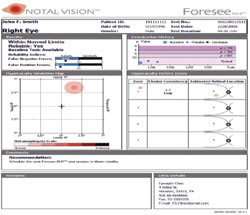
A screenshot of Foresee PHP results. |
Dr. Mehta says PHP fills a niche. "There's nothing like it out there. Before this technology, the average size lesion that could be picked up was about 3000 μm — or almost the size of a disc area — before the general ophthalmologists would become aware of it and refer the patient to a retina specialist for treatment. This instrument has the ability to pick up abnormalities in the patient's distortion field that come from lesions that are probably 60% to 70% smaller than what the norm had been up until now," says Dr. Mehta. "We're finding that with more frequent monitoring we're identifying these patients with better vision and that the lesions are less likely to be subfoveal. If we pick them up early enough, we may be able to treat effectively with thermal hot laser rather than doing damage control much further down the line."
INCREASED USE OF PHP
As the AMD population has grown in recent years, so has the use of PHP among general ophthalmologists — particularly those whose practices are comprised heavily of seniors. The PHP system, formerly known as the Preview PHP (Carl Zeiss Meditec, Dublin, Calif), was recently revamped, renamed, and reintroduced as the Foresee PHP (Notal Vision/MSS, Bloomington, Minn). The new version has improved ergonomics, which makes testing easier for both the patient and technician, but perhaps more importantly, the updated model provides a more comprehensive patient report.
The Foresee PHP report features data on the history of examinations, whether the visual field map is outside normal limits (and its p-value), test reliability, relative location of defects in the macular area, and the likelihood of each visual field defect being a true defect vs noise.
"The additional data give users a better idea of whether the pathology is true CNV," says Dr. Mehta. The report also includes recommendations for further actions. General ophthalmologists who use the Foresee PHP say this feature is particularly helpful in the efficient comanagement of patients with their retinal specialist colleagues.
Users say the test is patient-friendly and efficient. The patient is seated at a computer and with the help of a technician is guided through the process of responding via touchscreen technology to visual stimuli presented on the computer screen. A chin rest helps hold the patient's head in place. If a patient has unencumbered eye-hand coordination and is comfortable enough interfacing with the computer to respond in a timely fashion, they are considered a reliable candidate for the test, says Sara Sirkin, MD, a general ophthalmologist and PHP user.
Dr. Sirkin, of Sirkin Eyecare Center, Buffalo, NY, points to several instances when a patient's vision was saved because the test enabled her to detect macular changes more quickly [See sidebar: "Saving Viable Vision"]. "This device allows me to follow my AMD patients more closely and to identify changes more quickly so I can get them to the retina specialist and get them treated sooner, which is of course a big advantage," she says.
"If the PHP indicates a definite increase in the macular scotoma and I have some corroborating information from fundus photographs or OCT, I send the patient to one of several retinal specialists to whom I refer," says Dr. Sirkin. "They generally know that if I've seen changes on the PHP, odds are that FA will confirm those changes and then they can simply proceed with what's going to be the best treatment for the patient." Once treated, patients are referred back to Dr. Sirkin for continued monitoring.
|
Case Studies: Saving Viable Vision |
|
Below are several instances when viable vision was saved in AMD patients who might otherwise not have been as fortunate. Buffalo, NY, general ophthalmologist Sara Sirkin, MD, discusses her use of PHP visual field testing. Case 1. This male patient had 2 PHPs several months apart. Four months after the second test, he presented with vague complaints of not seeing things quite as clearly as he once had. This patient had previous cataract surgery and was a reliable patient. When Dr. Sirkin did the third PHP, a very subtle but definite change in pattern was identified. Dr. Sirkin did an OCT and saw an area slightly temporal to the foveal area that was suspiciously elevated. "I had enough suspicion that I sent him to a retina specialist," she says. Further testing identified a leak, and the patient was treated first with pegaptanib sodium (Macugen, OSI/Pfizer) and more recently with bevacizumab (Avastin, Genentech) and/or ranibizumab (Lucentis, Genentech). "He has maintained his vision, which had previously dropped from 20/30 to 20/50 and is now back to 20/30." Case 2: This female patient was a bilateral pseudophake who had macular drusen. She had 2 PHPs several months apart at Dr. Sirkin's practice. A third PHP revealed a definite suspicion of increase in scotoma. "After the test, I was actually able to see a minimal retinal change of a little hemorrhage," says Dr. Sirkin. The patient has been undergoing treatment since her pathology was identified and her vision has been maintained at 20/40. Case 3: A male patient (now deceased) who lost 1 eye to disease "long before the treatments and technology that we have today" began to have complaints following cataract surgery. Dr. Sirkin did a PHP, which showed increased scotoma. The patient was referred to a retina specialist who treated with pegaptanib sodium and/or bevacizumab and the patient maintained his 20/50 vision until his death. |
EARLY DETECTION
An estimated 80% of wet AMD patients are diagnosed too late for effective treatment. While a patient is asymptomatic and the Amsler grid is negative, the disease is already active and causing irreversible damage to the retina. With PHP testing, extrafoveal lesions can be identified at a stage when they can be effectively treated.
Foresee PHP users agree that the Amsler grid personifies the too-little, too-late cliché and a study comparing PHP to Amsler grid found that PHP had greater sensitivity.2
"You can put someone on high-dose antioxidants and give them an
Amsler grid to take home and consider checking them every 6 months, but the problem
with that is that the Amsler grid is a pretty lousy way of detecting progress to
CNV," says ophthalmologist John M. Weston, MD. "There are so many problems with
it. Compliance is a big issue, but even when patients follow through, they don't
know how to use it properly no matter how many times you go over it.
On top
of all that, there's really no way to control fixation."
PROBLEMS WITH THE AMSLER GRID
Dr. Mehta points out that the Amsler grid is apt to fail in detecting visual field defects until they are relatively large and subfoveal due to several reasons. First, there's the natural tendency to scan the world with the fovea and the fact that the Amsler grid does not force fixation. This causes patients to scan the grid with the fovea, ignoring nonfoveal lesions.
Probably the main reason for failure of the Amsler grid to serve as a tool for early detection of AMD lies in the ability of the human cortex to compensate for visual field defects, namely "'cortical completion." Furthermore, the interaction between neighboring lines in the periphery of the grid causes reduced detectability of visual fields, also known as "crowding."
Dr. Mehta says he and his retina colleagues are often referred AMD patients in the too early or too late stage. "This technology could help generalists refer patients at the appropriate stage when treatment by a retina specialist can best help save viable vision," he points out.
"By the time it shows up on an Amsler grid, a lesion is 1000 μm to 2000 μm and that's tougher to treat. Even with our new treatment modalities, we know that the less damage that has occurred: the smaller the lesion, the better the patient is likely to respond. With PHP, we can catch these patients at a much earlier stage," says Dr. Weston, a general ophthalmologist in private practice at the Weston Eye Center in Roseburg, Ore.
EARLY AND GOOD REFERRALS
Early referral before widespread changes occur throughout the macula is key. Dr. Weston says he relies on the Foresee PHP to narrow down — in an automated fashion — the patients who can gain the most by being referred to a retinologist.
"This system automates the process for me," he says. "We're monitoring patients in a maximal fashion, catching changes at the earliest possible time when treatment is likely to result in even better vision. It's much less of a guessing game for me now."
Retina specialists appreciate good referrals — meaning patients who are ripe for treatment — and Dr. Weston says the Foresee helps him oblige. "PHP improves good referrals by pinpointing high-risk individuals who have characteristics indicating that they are going from dry to wet AMD. Studies have shown that to be the case, and our experience in my practice has shown that as well," he says.
The ideal time for patients to undergo PHP testing is at the stage when National Eye Institute's Age-Related Eye Disease Study (AREDS) guidelines recommend high-dose antioxidants, according to Dr. Weston. "The intermediate drusen patient is the classic patient," he points out.
WHO SHOULD USE PHP
Dr. Mehta says he thinks the generalist's practice is the best place for this instrument, but he adds that, "given that we see so many AMD patients early in the progression of their disease, it can be very useful in a retina practice as well." Another reason for this, he says, is that often generalists are not comfortable following patients once they get more than a few drusen. "If these physicians don't have this technology available — and a lot of them don't — then we retina specialists may be the next best place for the technology because we probably understand its potential more than most generalists anyway."
There is some debate regarding the ideal frequency of PHP testing. The manufacturer recommends that once a patient is deemed an appropriate candidate for PHP, thenthe test should be performed quarterly. Dr. Mehta suggests that the decision should be that of the treating ophthalmologist and based on how frequently the patient is seen. "General ophthalmologists will be using this as a clinical screening tool; however, patient selection is very important. If they used it to get a baseline on every patient, they'd risk overutilization for something that's going to have very low yield. I use the same threshold as the AREDS, offering the test to patients with moderate to severe macular degeneration and then repeating it every 3 to 4 months," he says.
NON-NEOVASCULAR POSITIVES
Early PHP clinical research indicated a relatively high rate of false-positive results for healthy individuals, which appeared to be a limitation of the device.3 Dr. Mehta clarified this by explaining that those "false positives" were actually non-neovascular positives and may actually be another of PHP's features as opposed to a limitation.
"These really weren't 'false positives' because every one was positive for a reason. If it wasn't because the patient had wet AMD, it was because they fell into one of several other categories that apparently trigger this 'positive' outcome. For instance, having a large area of geographic atrophy can trigger the instrument to show a defect that looks suspicious for wet AMD, but one that does not show anything leaking. Also, if a patient has a large pigment epithelial detachment, this will also distort the macula in a similar way that a wet macular degeneration would," he explains. "If a patient has an RP detachment they should be sent to a retina specialist anyway, because they could be harboring new vessel growth."
Dr. Mehta says if the Foresee PHP is used correctly and regularly, and if the generalist is comfortable with the instrument, it is likely that the yield of patients who are referred for FA and OCT will have a better likelihood of having high-risk pathology that will need intervention. "Intuition and data tells me that PHP can help with earlier diagnosis, earlier intervention, and ultimately better prognosis. So the implications are huge in terms of maintaining usable viable vision for a longer period of time," he says.
REFERENCES
1. Alster Y, Bressler NM, Bressler SB, et al. Preferential Hyperacuity Perimeter (PreView PHP) for detecting choroidal neovascularization study. Ophthalmology. 2005;112:1758–1765.
2. Loewenstein A, Malach R, Goldstein M, et al. Replacing the Amsler grid: a new method for monitoring patients with age-related macular degeneration. Ophthalmology. 2003;110:966–970.
3. Goldstein M, Loewenstein A, Barak A, et al. Results of a multicenter clinical trial to evaluate the Preferential Hyperacuity Perimeter for detection of age related macular degeneration. Retina. 2005; 25:296–303.
Rochelle Nataloni is a freelance writer based in the Philadelphia area.