PEER REVIEWED
Gene Therapy for Age-Related
Macular Degeneration
DAVID KEEGAN, MD, PhD &
LUCIAN V. DEL PRIORE, MD, PhD
In its simplest form, gene therapy
involves replacing a defective or absent gene. This approach is being used for
the treatment of Leber's congenital amaurosis, which is due to a defect in the
RPE65 gene. However, this simple gene replacement approach is not likely to be
useful for the treatment of age-related macular degeneration (AMD), since this
multifactorial disease is unlikely to be due to
simple absence of a protein.
Current and future technologies allow elegant manipulation of the physiology of any micro-environment of the retina including the subretinal space. Gene therapy can be achieved by targeted cellular transfection, manipulation of inducible gene switches, the introduction of ribozyme technology that destroys or inactivates mutant proteins, and/or ex-vivo cellular manipulation with subsequent tissue transfer of transfected cells.
The purpose of this article is to provide an understanding of some of these concepts, with an appreciation of how these therapies may translate into the management of advanced AMD in the future. This is not an exhaustive review and the reader is directed to more complete reviews available in the recent literature.
|
|
|
Figure 1.
Intravitreal and subretinal gene-therapy delivery. |
BASIC MECHANISMS OF GENE THERAPY
The basic strategies of gene therapy can be separated into gene replacement, gene silencing, or delivery of a gene to produce a protein locally. These genes must be delivered in such a way as to introduce the gene into the cellular genome such that the local effect may be elicited.
■Replacing Absent or Defective
Gene/Protein.
The simplest application of gene therapy occurs when patients develop a disease
due to complete absence of a protein product. Typically, this occurs in
autosomal recessive diseases in which no protein is made, and absence of the
protein leads to disease. The concept here is that a viral vector can be
engineered to carry DNA that codes for the missing gene; the DNA is then
inserted into the host DNA or maintained as a plasmid within the host nucleus
such that transcription of healthy protein will occur. Several factors can be
used to ensure the specificity of targeted gene delivery, including targeted
vector delivery to a specific anatomic location, such as the vitreous cavity or
subretinal space (Figure 1); the use of a cell-specific promoter region on the
gene construct to limit gene expression to certain cells types (eg, using a
rhodopsin promoter to limit gene expression to photoreceptors as a means of
targeting these cells for photoreceptor-based treatments); use of viral vectors
that have a high affinity for a particular cell type; or performing gene therapy
ex vivo in explanted cells in culture, which can then be introduced into the
subretinal space or vitreous cavity. In principle, introduction of a specific
local source of protein production should be therapeutic if the disease is due
to protein absence; the poster child for treatment of autosomal recessive
retinal disorders is represented by recent groundbreaking pre-clinical studies
of gene therapy in a dog model of Leber's Amaurosis (RPE65-/-).1,2
The role of gene replacement therapy in the treatment of AMD is not known at the
current time, but it is unlikely that this
disease is due to absence of a
single protein.
■Gene Silencing. This approach is favored for the treatment of disorders that are due to the presence of a mutant or aberrant protein; normally these disorders are present in diseases that are dominantly inherited. Typically, a normal protein product is present as well due to expression of a normal gene on the other allele, but disease is caused by abnormal protein caused by expression of an abnormal gene. Here the goal of treatment is to destroy or remove the abnormal protein. This can be achieved using RNA inhibition (RNAi and siRNA) or ribozyme technology; where these agents are capable of binding to a cleavage site of the target RNA resulting in disruption of its transcription and expression (Figure 2). Ribozymes or siRNAs can be delivered with viral or liposomal vectors.
■Enhanced Production of Beneficial Protein. Another potential application of gene therapy is to introduce a gene that will result in an increase in the local concentration of a beneficial protein. Here, gene therapy would allow continuous expression of a protein that could be used to treat the disease. The best example of this approach in AMD is the recently reported phase 1 study using Adenoviral-vector delivered PEDF (AdPEDF.11) to suppress choroidal neovascularization in AMD.3 Other examples include the production of a soluble VEGF receptor (Flt-1)4 or delivery of growth factors in animal models of inherited retinal disease.5,6
GENE REGULATION

|
|
Figure
2. RNA interference using inhibitors of RNA (siRNA and
ribozymes). A. The therapeutic siRNA is delivered and enters the cell by endocytosis in a vector or liposomal system. The siRNA binds to host RNA-induced silencing complex (RISC) in the cell. This complex loses a strand from the siRNA, which then binds with host cell messenger RNA. This cleaves the host mRNA and prevents protein production. B. Ribozymes are small RNA molecules, generally of a "hammerhead" or "hairpin" configuration. They bind to specific cleavage sites on host messenger RNA and make them more susceptible to intracellular RNA hydrolases. Messenger RNA is cleaved and protein translation does not occur. |
|
|
In order for gene therapy to be safe and effective, it is important that techniques are developed to control the expression and behavior of the gene following insertion. Simple introduction of a therapeutic gene may not be sufficient in the long run if the protein product is produced at concentrations that are either too low or too high for the desired therapeutic effect. Careful regulation of gene expression, and therefore the levels of gene product, can be achieved using a relevant promoter element on the gene to deliver protein to the target tissue. Examples of this approach include the use of rhodopsin promoters in the photoreceptors, or PEDF promoters in the retinal pigment epithelium (RPE) and choroid, to regulate gene expression. Altered gene expression can also be secondary to changes in the cellular microenvironment such as hypoxia; here it is possible to use hypoxia-sensitive response elements (HRE) to regulate the expression of anti-angiogenic genes (Figure 3).
Target gene expression may be modified further by using a switch system chemosensitive to a tetracycline (eg, doxycycline); in the Tet-ON system the gene of interest is linked to a tetracycline response element (TRE) which in turn is modified by a reverse tetracycline-dependant transactivator (rtTA: Figure 4). Doxycycline binds to rtTA which in turn binds to and activates the TRE inducing upregulation of the target gene. The Tet-OFF system is mediated through the tetracycline-dependant transactivator (tTA), where the increase in gene activity occurs following removal of doxycycline. Unbound tTA binds to the TRE inducing gene expression.
The choice of gene delivery system can also aid the regulation of gene expression. Adenoviral vectors do not maintain long-term expression well as they do not integrate into the host genome, and thus they are ideal for acute rather than chronic disease. In contrast, adeno-associated viruses can maintain long-term expression due to stable host genome integration.
GENE THERAPY VECTORS
Gene therapy requires an efficient delivery system. Several factors control the efficiency of gene therapy and subsequent protein production:
■Gene insertion in target tissue. This is particularly important in relation to the retina, as transduction of neural retina is more difficult than RPE. This can be overcome by the choice of vector systems, since some viruses have a predilection for transfection of different target tissues. For example, AAV vectors can achieve good photoreceptor and RPE transduction whereas retroviral vectors only transfect dividing cells and may not be appropriate for retinal gene therapy (Table 1).
■Appropriate passenger genetic material (eg, switches or tissue/physiological specific promoters). See details of the Tet-ON or Tet-OFF system above and in Figure 4. Physiological promoters represent another attractive way of regulating local protein production. For example, in principle one can fine-tune the level of VEGF expression to the amount of VEGF by tying the expression levels of anti-VEGF agents to the presence of an upstream modulator of VEGF production, such as the HRE which controls VEGF production.7 An HRE responsive promoter sequence can be placed on the delivered gene, resulting in an anti-VEGF protein such as Flt-1, the soluble VEGF receptor, being produced. This type of system effectively creates a local auto-regulatory pathway (Figure 3).
Viral Vectors
Modified viruses are the most common vectors used in gene therapy as they allow effective intracellular delivery of genetic material. Several factors are important in determining the ideal viral vector for a certain therapeutic use, including the predilection of the viruses for certain tissues and cells, and the size of the DNA fragment that can be inserted with a given vector (eg, adeno-associated virus and photoreceptors).8 Potential viral vectors for ocular use include adenovirus, adeno associated virus, retroviruses, and lentiviruses.

Ex vivo gene therapy, in which explanted cells
are transfected prior to reimplantation in the eye, can provide an attractive
treatment alternative for patients with age-related macular degeneration. In
principle, RPE modified ex vivo can be delivered into the subretinal space to
provide physiological levels of key molecules, such as anti-VEGF agents, PEDF,
growth factors such as ciliary derived neurotrophic factors (CNTF), or
anti-apoptotic agents including bcl-2
or caspase inhibitors. Caspases are
crucial enzymes in the apoptotic cascade and form an integral part of the final
pathway in the majority of causes of apoptosis. Caspase inhibition has been
shown to limit apoptosis in many cell systems including those subjected to
oxidative stress.9,10
The benefit of ex vivo gene therapy is the potential to accurately determine the protein production of these cells prior to inserting them into the eye. Disadvantages include difficulty sourcing cells for transplantation, the potential for immune rejection of the transplanted cells,11-13 and alterations in protein production that can develop after the cells are transplanted back into the eye.
Delivery of Vector
Delivery of the vector is an important consideration in gene therapy. The issues to be considered include safety, efficacy, reproducibility, and convenience. When considering vector delivery for eye disease, the following routes are most commonly considered:
►intravitreal injection (Figure 1A)
►subretinal injection (Figure 1B)
►subtenon's injection
►systemic delivery
All of these have been considered but the most likely route of delivery in initial trials (eg, the forthcoming gene therapy trial for Leber's Amaurosis) will be subretinal or intravitreal.3,14 However, the AdPEDF.11 trial has been expanded in animal models (pig) to assess the efficacy of the subtenon's route of delivery with encouraging results;15 if successful, this route would allow for a relatively non-invasive method for therapeutic delivery.
Issues that are relevant to the delivery technique include tissue penetration of the vector, the ability of the vector to enter the target cell by endocytosis or other means, the resistance of the gene and the agent to intracellular hydrolases to survive, and the half-life of the agent in the target tissue. In principle, genes that are incorporated in the host genome should be able to maintain expression for the life of the host cell, although this is not always the case.
POTENTIAL GENE
TARGETS FOR AMD
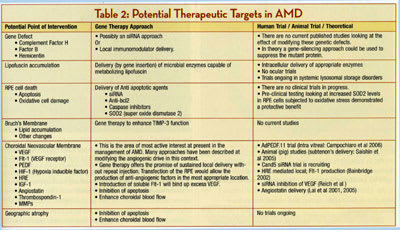
As described above, the initial steps in the development of AMD are not understood completely, thus making it difficult to outline a logical gene therapy approach to the management of early disease. However, previous studies have suggested a link between mutations in genes for complement factor H, factor B, hemicentin, fibulin, and/or ABCA4 that may confer or modify a patient's risk of acquiring the disease. Clinically, disease is associated with lipofuscin accumulation, lipid accumulation, and thickening and collagen cross-linking within Bruch's membrane; visual loss occurs through the development of geographic atrophy or choroidal neovascularization. Currently, the limited gene therapy trials in AMD are targeted at controlling neovascularization in advanced exudative AMD. Future studies may be directed at geographic atrophy.
■Gene Therapy for Neovascular AMD. The growth of abnormal choroidal vessels that characterize the end-stage of AMD is an obvious target for the application of therapies, specifically towards the VEGF molecule. To date, there has been just 1 gene therapy trial published in relation to AMD. Campochiaro and colleagues reported earlier this year on the results of their phase 1 clinical trial using adenoviral vector-delivered pigment epithelium-derived factor (AdPEDF.11) via intravitreal injection.3 This dose-escalation study was specifically designed to assess safety; a therapeutic benefit (less progression in growth of lesion size) was detected and doses >108 PU were used. No serious local or systemic adverse events were encountered. Mild inflammation and moderate pressure rises were reported, with one patient developing marked (grade 3) inflammation. Serum antibodies to adenovirus were unchanged in 27 patients, with only 1 patient demonstrating a temporary titre rise that returned to normal. It must be noted that only 28 patients (3 patients per dose level except 109.5 PU where 7 patients were enrolled) were treated in this study and safety data with trend effect are reported. Further studies with a larger cohort that look specifically at efficacy are ongoing.
This study coupled with the recent paper on gene therapy for retinoblastoma14 establishes adenovirus as a good potential vector for delivery of ocular gene therapy.
Other targets for treatment and/or prevention of neovascular AMD are listed in Table 2. Adeno-associated viral (AAV) delivery of angiostatin16 a plasminogen-derived fragment that is a potent inhibitor of angiogenesis17 or Flt-14 has been shown to suppress CNV in animal models. Other gene therapy based agents include the siRNA approach to inhibiting VEGF18 and recruitment is currently ongoing for the Cand5 siRNA (inhibitor of VEGF mRNA: Acuity Pharmaceuticals) trial.
■Gene Therapy for Geographic Atrophy. In AMD, changes lead to the accumulation of intracellular (RPE) lipofuscin and extra cellular deposits (drusen and basal laminar deposits) that contain complement complexes and other inflammatory markers19. These lead to alterations in the nature and thickness of Bruch's membrane and oxidative stress,20 leading to cellular changes in the RPE, inducing apoptosis with secondary neural retinal degeneration. An approach in geographic atrophy may be to introduce therapeutic genes into the host RPE to enhance their survival in this environment. This may be achieved in this environment using virally delivered anti-apoptotic factors eg, super-oxide dismutase 2 (SOD2); caspase inhibitors or agents that will increase resistance to apoptosis such as integrins (eg, av�3).
|
|
|
Figure 3. Gene regulation using a
physiologic promoter. |
CAN WE PREVENT AMD WITH GENE THERAPY?
It is apparent that diet and environmental factors such as smoking play a role in the course of the disease, but there is now strong evidence for a hereditable component.21-23 Recently, definitive gene mutations have been identified as common to a large number of AMD sufferers: complement factor-H,24,25 with modifiers (Factor B),26 HEMICENTIN-1,(27) fibulin, and ABCA4. These are exciting developments and may lead to a greater understanding of the underlying pathogenic mechanisms that are important in the development of the disease. Several authors have proposed a role for abnormal complement activation in the development of AMD; this role is supported by the presence of complement components in the extracellular milieu in AMD eyes;19 the development of AMD-like deposits in a knockout mouse28 and the presence of CD46, an important regulator of complement activation that is associated with the cell attachment protein �1�integrin, on the basal RPE surface.29 We are now in a better position than ever to appreciate the exact pathogenesis of AMD; this should hopefully lead to better therapies. In principle, it may be possible to alter specific protein levels in the macula by performing gene therapy in patients with a definitive AMD associated gene mutation; such an application may be possible in the future.
It is interesting to note that it may be possible to target intraocular lipofuscin accumulation with gene therapy in the future. There is a growing amount of evidence for the existence of microbes that can metabolize intracellular lipofuscin.30 Based on these observations, de Grey proposed a therapeutic approach to the age-related storage diseases, involving the identification of enzymes capable of degrading lipofuscin. These may be introduced into human cells by gene therapy as a means of removing the offending material.31 This future strategy is similar to the strategy currently employed for FDA-approved trials of enzyme-replacement therapy for 2 major lysosomal storage disorders, non-neuronopathic Gaucher disease and Fabry disease. Whether this approach will prove to be helpful in AMD remains to be determined.
SUMMARY
Research into AMD has advanced greatly in the past decade, particularly with the application of molecular techniques. The recent completion of the Human Genome Project will facilitate identification of gene mutations that may predispose patients to AMD, and in the future it may be possible to use gene therapy to modify the expression of these genes. The most immediate application of gene therapy in AMD will involve targeted therapy aimed at controlling late manifestations of this disease, such as geographic atrophy and choroidal neovascularization. The potential to deliver gene therapy to the eye without systemic side effects is great. We are currently enjoying the benefits of anti-VEGF agents; the use of gene therapy to modulate early and advanced disease is the next horizon in the management of this destructive condition.
REFERENCES
|
|
|
Figure 4. Tet-Off and Tet-On gene
switch system. A. Tet-Off system. In the absence of a tetracycline (eg, doxycycline), the tTA binds to the TRE and activates transcription of the gene of interest, eg, PEDF. Exogenous doxycycline inactivates tTA and gene transcription is silenced. B. Tet-On system. In this system, the rtTA is maintained in an inactive state in the absence of doxycycline and transcription of the gene is silenced. In the presence of drug, the rtTA binds to the TRE and activates the transcription of PEDF. |
1. Acland GM, Aguirre GD, Ray J, et al. Gene therapy restores vision in a canine model of childhood blindness. Nat Genet. 2001;28:92-95.
2. Acland GM, Aguirre GD, Bennett J, et al Long-term restoration of rod and cone vision by single dose rAAV-mediated gene transfer to the retina in a canine model of childhood blindness. Mol Ther. 2005;12:1072-1082.
3. Campochiaro PA, Nguyen QD, Shah SM, et al. Adenoviral vector-delivered pigment epithelium-derived factor for neovascular age-related macular degeneration: results of a phase I clinical trial. Hum Gene Ther. 2006;17:167-176.
4. Bainbridge JW, Mistry A, De Alwis M, et al. Inhibition of retinal neovascularisation by gene transfer of soluble VEGF receptor sFlt-1. Gene Ther. 2002;9:320-326.
5. Wu WC, Lai CC, Chen SL, et al. Long-term safety of GDNF gene delivery in the retina. Curr Eye Res. 2005;30:715-722.
6. Schuettauf F, Vorwerk C, Naskar R, et al. Adeno-associated viruses containing bFGF or BDNF are neuroprotective against excitotoxicity. Curr Eye Res. 2004;29:379-386.
7. Su H, Arakawa-Hoyt J, Kan YW. Adeno-associated viral vector-mediated hypoxia response element-regulated gene expression in mouse ischemic heart model. Proc Natl Acad Sci U S A. 2002;99:9480-9485.
8. Ali RR, Sarra GM, Stephens C, Alwis MD, et al. Restoration of photoreceptor ultrastructure and function in retinal degeneration slow mice by gene therapy. Nat Genet. 2000;25:306-310.
9. Van De Water TR, Lallemend F, Eshraghi AA, et al. Caspases, the enemy within, and their role in oxidative stress-induced apoptosis of inner ear sensory cells. Otol Neurotol. 2004;25:627-632.
10. Jiang S, Moriarty-Craige SE, Orr M, Cai J, Sternberg P Jr, Jones DP. Oxidant-induced apoptosis in human retinal pigment epithelial cells: dependence on extracellular redox state. Invest Ophthalmol Vis Sci. 2005;46:1054-1061.
11. Lund RD, Ono SJ, Keegan DJ, Lawrence JM. Retinal transplantation: progress and problems in clinical application. J Leukoc Biol. 2003;74:151-160.
12. Del Priore LV, Sheng Y, Johnson E, et al. Identification of transplanted retinal pigment epithelium with a novel chromosomal marker. Curr Eye Res. 2003;26:125-31.
13. Del Priore LV, Ishida O, Johnson EW, et al. Triple immune suppression increases short-term survival of porcine fetal retinal pigment epithelium xenografts. Invest Ophthalmol Vis Sci. 2003;44:4044-4053.
14. Chevez-Barrios P, Chintagumpala M, Mieler W, et al. Response of retinoblastoma with vitreous tumor seeding to adenovirus-mediated delivery of thymidine kinase followed by ganciclovir. J Clin Oncol. 2005;23:7927-7935.
15. Saishin Y, Silva RL, Saishin Y, et al. Periocular gene transfer of pigment epithelium-derived factor inhibits choroidal neovascularization in a human-sized eye. Hum Gene Ther. 2005;16:473-478.
16. Lai CC, Wu WC, Chen SL, et al. Recombinant adeno-associated virus vector expressing angiostatin inhibits preretinal neovascularization in adult rats. Ophthalmic Res. 2005;37:50-56.
17. Wahl ML, Kenan DJ, Gonzalez-Gronow M, Pizzo SV. Angiostatin's molecular mechanism: aspects of specificity and regulation elucidated. J Cell Biochem. 2005;96:242-261.
18. Reich SJ, Fosnot J, Kuroki A, et al. Small interfering RNA (siRNA) targeting VEGF effectively inhibits ocular neovascularization in a mouse model. Mol Vis. 2003;9:210-216.
19. Hageman GS, Luthert PJ, Victor Chong NH, et al. An integrated hypothesis that considers drusen as biomarkers of immune-mediated processes at the RPE-Bruch's membrane interface in aging and age-related macular degeneration. Prog Retin Eye Res. 2001;20:705-32.
20. Zarbin M. Current concepts in the pathogenesis of age-related macular degeneration. Arch Ophthalmol. 2004;122:598-614.
21. Seddon JM, Cote J, Page WF, Aggen SH, Neale MC. The US twin study of age-related macular degeneration: relative roles of genetic and environmental influences. Arch Ophthalmol. 2005;123:321-327.
22. Gorin MB, Breitner JC, De Jong PT, et al. The genetics of age-related macular degeneration. Mol Vis. 1999;5:29.
23. Yates JR, Moore AT. Genetic susceptibility to age related macular degeneration. J Med Genet. 2000;37:83-87.
24. Hageman GS, Anderson DH, Johnson LV, et al. A common haplotype in the complement regulatory gene factor H (HF1/CFH) predisposes individuals to age-related macular degeneration. Proc Natl Acad Sci U S A. 2005;102:7227-7232.
25. Haines JL, Hauser MA, Schmidt S, et al. Complement factor H variant increases the risk of age-related macular degeneration. Science. 2005;308:419-421.
26. Gold B, Merriam JE, Zernant J, et al. Variation in factor B (BF) and complement component 2 (C2) genes is associated with age-related macular degeneration. Nat Genet. 2006;38:458-462.
27. Schultz DW, Klein ML, Humpert AJ, et al. Analysis of the ARMD1 locus: evidence that a mutation in HEMICENTIN-1 is associated with age-related macular degeneration in a large family. Hum Mol Genet. 2003;12:3315-3323.
28. Ambati J, Anand A, Fernandez S, et al. An animal model of age-related macular degeneration in senescent Ccl-2- or Ccr-2-deficient mice. Nat Med. 2003;9:1390-1397.
29. McLaughlin BJ, Fan W, Zheng JJ, et al. Novel role for a complement regulatory protein (CD46) in retinal pigment epithelial adhesion. Invest Ophthalmol Vis Sci. 2003;44:3669-3674.
30. de Grey AD. Bioremediation meets biomedicine: therapeutic translation of microbial catabolism to the lysosome. Trends Biotechnol. 2002;20:452-455.
31. de Grey AD, Alvarez PJ, Brady RO, et al. Medical bioremediation: prospects for the application of microbial catabolic diversity to aging and several major age-related diseases. Ageing Res Rev. 2005;4:315-338.
BIBLIOGRAPHY
Bainbridge JW, Mistry A, Binley K, et al. Hypoxia-regulated transgene expression in experimental retinal and choroidal neovascularization. Gene Ther. 2003 Jun;10(12):1049-54.
Edwards AO, Ritter R 3rd, Abel KJ, Manning A, Panhuysen C, Farrer LA. Complement factor H polymorphism and age-related macular degeneration. Science. 2005;308:421-444.
Klein RJ, Zeiss C, Chew EY, et al. Complement factor H polymorphism in age-related macular degeneration. Science. 2005;308:385-389.
Lai CC, Wu WC, Chen SL, et al. Suppression of choroidal neovascularization by adeno-associated virus vector expressing angiostatin. Invest Ophthalmol Vis Sci. 2001;42:2401-2407.
Reichel MB, Bainbridge J, Baker D, Thrasher AJ, Bhattacharya SS, Ali RR.
An immune response after intraocular administration of an adenoviral vector containing a beta galactosidase reporter gene slows retinal degeneration in the rd mouse. Br J Ophthalmol. 2001;85:341-344.
David Keegan, MD, PhD, is in the Department of Ophthalmology, Columbia University, New York, NY. He can be e-mailed at djk2112@columbia.edu. Lucian V. Del Priore, MD, PhD, is a professor and Robert L. Burch III Scholar in the Department of Ophthalmology, Columbia University, New York, NY. Dr. Del Priore is also in private practice at Vitreous-Retina-Macula Consultants of New York in Manhattan. He can be e-mailed at lvdelpriore@gmail.com. Neither author has a financial interest in any of the information contained in this article.











